360° Fusion for Mid Lumbar Traumatic Instable Burst Fractures in Osteoporotic Patients
Tony Van Havenbergh*, Pieter Van Loo, Raf Van Paesschen, Kris De Smedt and Dirk Berghmans
Department of neurosurgery, GZA Hospitals, Belgium
Submission: February 04, 2017; Published: February 17, 2017
*Corresponding author: Tony Van Havenbergh, Department of neurosurgery, GZA Hospitals, Oosterveldlaan 24B-2610 Wilrijk, Antwerp, Belgium, Tel: 323-443-3772; Fax: 323-443-3018; Email: tony.vanhavenbergh@GZA.be
How to cite this article: Tony V H, Pieter V L, Raf V P, Kris D S, Dirk B. 360o Fusion for Mid Lumbar Traumatic Instable Burst Fractures in Osteoporotic Patients. Open Access J Neurol Neurosurg. 2017; 2(4): 555594. DOI: 10.19080/OAJNN.2017.02.555594
Abstract
The authors present a small review of the occurrence, classification and treatment of osteoporotic unstable mid lumbar burst fractures. The review is illustrated by 2 cases.
Keywords: Lumbar burst fractures; 360° fusion; Osteoporosis
Introduction
Mid lumbar traumatic burst fractures are not so uncommon. They mostly occur in high energy axial loading traumas. In patients with a predisposing osteoporotic situation though, severe burst fractures at the mid lumbar level can develop after relatively minor trauma [1-3]. The fragments of the vertebra can cause a narrowing of the spinal canal and in some cases devastating neurological deficit. Thoraco lumbar burst fractures can be classified using the Denis classification [4], the AO- classification of Magerl [5] and a load sharing classification according to Mc Cormack [6]. These fractures can lead to severe functional impact. Long term complications in terms of kyphosing and persistent pain are common if not treated properly [7,8]. Especially in the osteoporotic patient a first line stable reconstruction of the spine is mandatory to prevent long term complications. We present 2 cases of L3 burst fractures in patients with an osteoporotic predisposition.
Case 1
A 56 year old lady presented after falling of a staircase. She immediately experienced a stabbing pain in the lumbar region with irradiation in both legs. Upon admission there was no neurological deficit. X-ray of the lumbar spine showed a burst fracture of L3. On CT there was an almost 90% stenosis at the L3 level, caused by a fragment of the L3 burst fracture. Patient was transferred to the neurosurgery department. She was initially stabilized through a posterior approach with a pedicle screw and rod fixation from L1 to L5. The bone quality was poor because of known osteoporosis. Through distraction, a partial reposition of the L3 fragment in the spinal canal was achieved and an adjuvant laminectomy and facetectomy was performed to fully decompress the spinal canal. A dural tear was encountered with rootlets bulging out. The dural tear was repaired. Patient was neurologically intact after the surgery. In view of the osteoporosis we decided to add an anterior stabilization to prevent pseudarthrosis and kyphotic complication on the medium long term. In a second stage, an anterolateral approach was done to L3 with corporectomy and interposition of an expandable cage. Patient recovered well after this procedure and could be mobilized within 2 days. She was discharged for further rehab at the 4th postoperative day.
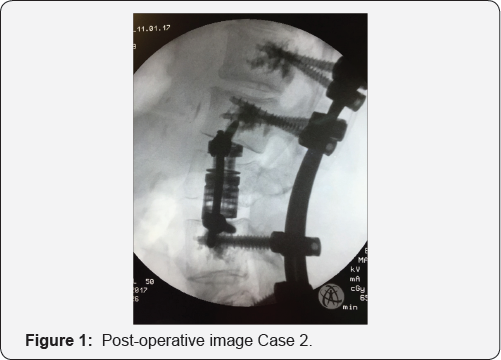
Case 2
A 63 year old female patient was admitted through emergency ward after she stumbled and fell on her buttocks. She suffered immediate excruciating low back pain, she was neurologically intact. X-ray and CT of the lumbar spine demonstrated a burst fracture of L3 with a fragment in the spinal canal causing a 50% canal stenosis and a suspicion of severe osteoporosis. The patient received a 2 step surgery consisting of posterior pedicle screw stabilisation from L2 to L5with cement augmentation of the screws and an additional antero lateral approach with partial corporectomy of L3 and expandable cage interposition (Figure 1). Her recovery was uneventful with immediate pain relief and discharge on day 3 after her anterior surgery.
Discussion
Burst fractures of the mid lumbar spine are not uncommon. These fractures can cause severe complications such as neurological deficit or untreatable pain due to sagittal balance disruption. In about 60% there is an important impact on quality of life [1-3]. The severityof these fractures can be defined with different classifications. The most commonly used classifications are: The Denis classification [4] where the posterior, middle and anterio column is taken into account. The AO Magerl [5] score defining compression [A], distraction [B] or axial torque [C]. The Load Sharing Score by McCormack [6-8] based on comminution, apposition and kyphosis. Based on these scoresthere is a consensus on which fractures should be treated surgically and which can be treated conservatively [9]. In general the high grade instable fractures are indications for surgical stabilization [10]. The reason is the high risk for progressive hyperkyphosis leading to severe disability. There is an ongoing discussion on how to treat these instable midlumbar burst fractures. Some advocate posterior stabilization [11] without bony augmentation, others advocate adjuvant bone grafting, Some prefer unique anterior stabilization [12]. The role of vertebroplasty or kyphoplasty is still under debate, but the application of cement in a severely fractured vertebral body, especially with a disruption of the posterior wall, is questionable. In osteoporotic unstable communitive fractures with a load sharing score of >7, a combined posterior and anterior stabilization seems the best option for long term good outcome [13-15]. Using minimally invasive techniques as well for posterior as anterior approaches, one can minimize surgical trauma to the patient and provide very early mobilization.
Conclusion
Unstable osteoporotic lumbar burst fractures can cause severe disability by neurological deficit but also by chronic pain through sagittal balance disruption. 360° lumbar stabilization can be performed with minimally invasive techniques leading to direct mobilization of the patients.
References
- Briem D, Lehmann W, Rueckner AH, Windolf J, Rueger JM, et al. (2004) Influencing the quality of life after burst fractures of the thoraco lumbar transition. Arch Orthop Trauma Surg 124(7): 461-468.
- Post RB, Keizer HJE, Leferink VJM, Sluis CK (2006) Functional outcome 5 years after non-operative treatment of type A spinal fractures. Eur Spine J 15(4): 472-478.
- Bakhsheshian J, Dahdaleh NS, Fakurnejad S, Scheer JK, Smith ZA (2014) Evidence-based management of traumatic thoraco lumbar burst fractures: a systematic review of non operative management. Neurosurg Focus 37(1): E1.
- Denis F, Armstrong GWD, Searls K, Matta L (1984) Acute thoraco lumbar burst fractures in the absence of neurologic deficit. Clin Orthop Relat Res 189: 142-149.
- Magerl F, Aebi Gertzbein SD, Harms J, Nazarian S (1994) A comprehensive classification of thoracic and lumbar injuries. Eur Spine J 3(4): 184-201.
- Mc Cormack T, Karaikovic E, Gaines RW (1994) The load sharing classification of spine fractures. Spine 19(15): 1741-1744.
- Koller H, Acosta F, Hempfing A, Rohrmüller D, Tauber M, et al. (2008) Long-term investigation of nonsurgical treatment for thoraco lumbar and lumbar burst fractures: an outcome analysis in sight of spinopelvic balance. Eur Spine J 17(8): 1073-1095.
- Been HD, Poolman RW, Ubags LH (2004) Clinical outcome and radiographic results after surgical treatment of post-traumatic thoraco lumbar kyphosis following simple type a fractures. Eur Spine J 13(2): 101107.
- Thomas KC, Bailey CS, Dvorak MF, Kwon B, Fisher C (2006) Comparison of operative and non operative treatment for thoraco lumbar burst fractures in patients without neurological deficit: a systematic review. J Neurosurg Spine 4(5): 351-358.
- Sasso RC, Renkens K, Hanson D, Reilly T, Mcguire RA, et al. (2005) Unstable thoraco lumbar burst fractures. J Spinal Disord Tech 19(4): 242-248.
- Altay M, Ozkurt B, Nuri Aktekin C, Ozturk AM, Dogan Ö, et al. (2007) Treatment of unstable thoraco lumbar junction burst fractures with short- or long-segment posterior fixation in Magerl type A fractures. Eur Spine J. 16(8): 1145-1155.
- Bence T, Schreiber U, Grupp T, Steinhauser E, Mittelmeier W (2007) Two column lesions in the thoraco lumbar junction: anterior, posterior or combined approach? A comparative biomechanical in vitro investigation. Eur Spine J 16(6): 813-820.
- Korovessis P, Baikousis A, Zacharatos S, Petsinis G, Koureas G, et al. (2006) Combined anterior plus posterior stabilization versus posterior short-segment instrumentation and fusion for mid-lumbar (L2-L4) burst fractures. Spine 31: 859-868.
- Hitchon PW, Torner J, Eichholz KM, Beeler SN (2006). J Neurosurg Spine 5(2): 117-125.
- Payer M (2006) Unstable burst fractures of the thoraco-lumbar junction: treatment by posterior bisegmental correction/fixation and staged anterior corpectomy and titanium cage implantation. ActaNeurochir (Wien) 148(3): 299-306.






























