Embolic Stroke and Nephrotic Syndrome: A Case Report and Literature Review
Nishanth Kodumuri, Sonal Mehta, Charmaine Jenkins , Ravish Kothari and X Michelle Androulakis*
Department of Neurology, University of South Carolina School of Medicine, USA
Submission: January 30, 2017; Published: February 06, 2017
*Corresponding author: X Michelle Androulakis, MD, MS, Assistant Professor of Clinical Neurology, University of South Carolina School of Medicine, Eight Medical Park, Suite 420, Columbia, SC 29203, USA, Tel: (803] 545-5060; Email: Michelle.Androulakis@uscmed.sc.edu
How to cite this article: Nishanth K, Sonal M, Charmaine J, Ravish K, X Michelle A. Embolic Stroke and Nephrotic Syndrome: A Case Report and Literature Review. Open Access J Neurol Neurosurg. 2017; 2(4): 555591. DOI: 10.19080/OAJNN.2017.02.555591
Abstract
Nephrotic syndrome (NS) is less commonly associated with arterial thrombosis than venous thrombosis. We report a case of a 43-year- oldwomanwho presented with an acute embolic stroke confirmed on MRI, about 3 months after the diagnosis of NS. The standard stroke evaluations did not show evidence ofcardiac source of embolism, large vessel atherosclerosis or any primary hypercoagulable disorders. Laboratory tests revealed impaired renal function and extremely high nephrotic range proteinuria and a renal biopsy showed primary membranous glomerulonephropathy. Subsequently, she was discharged on anticoagulation and responded well to the treatment. This case illustrates the importance of considering hypercoagulable evaluation due to nephrotic syndrome as a potential cause of embolic stroke, and the initiation of anticoagulation therapy in a timely manner. We also present a literature review on the association between nephrotic syndrome and acute stroke.
Keywords: Stroke; Nephrotic syndrome; Hypercoagulable state; Arterial thrombosis
Introduction
It has been shown that patients with nephrotic syndrome (NS) are prone to thrombo-embolic phenomena [1, 2]. The risk of thrombo embolism is increased during the first 6 months of the onset of NS3. In adults with NS, arterial thrombo embolic events are not as well characterized and less commonly reported than venous thrombo embolism [4]. Acute ischemic stroke is a rare complication of NS [5,6,7] and this link has not been widely reported in the literature.
Although the exact pathogenesis of cerebral infarction is not clearly understood, it has been postulated that a hyper coagulable state in NS may play an important role in ischemic stroke [3,8]. Few studies have suggested that hyper coagulability in NS is associated with the steroid and diuretic administration [9]. Although there are case reports of NS and stroke [7,10-16], we report this case to illustrate the importance of considering hypercoagulability from NS as a potential cause of embolic stroke, and to initiate anticoagulation treatment if appropriate. Additionally, we performed an extensive literature search for NS and association with ischemic stroke.
Case Report
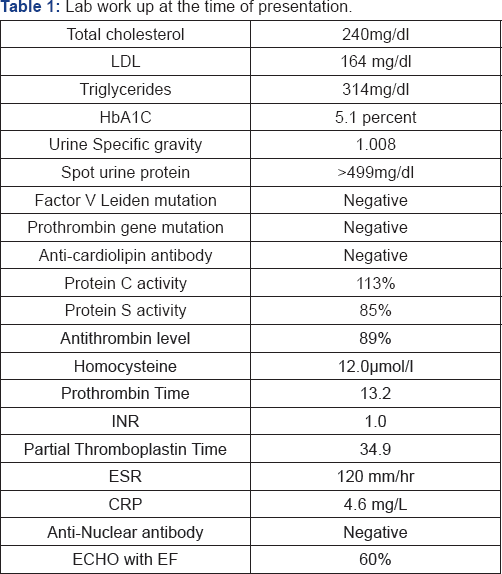
A 43-year-old, left-handed, woman presented with sudden onset of left sided weakness and word finding difficulty three months after the diagnosis of NS. Her other pertinent medical history included COPD, hypertension and was a smoker, with no significant family history for coagulation disorders. NS with membranous glomerulonephropathy was confirmed with biopsy during this admission. Medication history at the time of presentation included cyclophosphamide, prednisone, spironolactone, Lasix, Lisinopril and metoprolol. Her vitals were stable at presentation and general physical examination was benign. Her neurologic examwas significant for mild anomia and left sided weakness. Her laboratory tests showed significant proteinuria, mild hyperlipidemia and the standard hypercoagulable workup was normal. Other laboratory values are as detailed in Table 1.
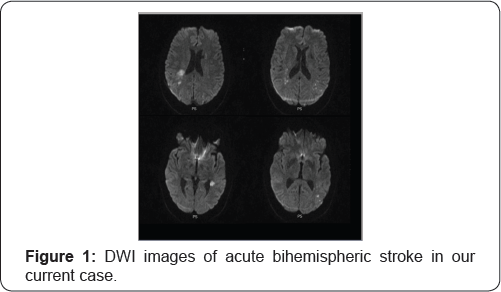
Further work up included an MRI which revealed bi hemispheric regions of diffusion restriction, consistent with acute infarcts (Figure 1). Her cardiac work up was essentially normal. Vascular imaging of the brain was obtained with a CT angiogram which showed a left MCA occlusion at the M3- M4 segments, without evidence of any proximal large artery atherosclerosis. Given the bihemispheric infarcts, an underlying embolic source was likely. After an exhaustive cardiac work up did not reveal any source of cardio embolism, the possibility of hypercoagulability with significant proteinuria due to NS was considered the likely etiology, and anticoagulation was initiated.
Literature Review
Systematic searches of peer-reviewed, published, research papers indexed in PubMed, EMBASE, and Science Direct from inception until Nov. 2016 were undertaken using key search terms related to ‘Nephrotic Syndrome', ‘ischemic stroke', and ‘infarction'. We identified 30 reported cases of acute ischemic strokes with NS after eliminating 10 cases with nephropathy related to DM. The age at the presentation ranged from 14 -73 years with a mean age of 40.7, and standard deviation 15.7 years. 70% of the cases (21/30) were male. Among 30 there were only 5 cases without a biopsy-proven diagnosis of NS, most of the cases (8/30) were membranous disease. The other cases were associated with Memberano proliferative Glomerulo nephritis, minimal change disease, IgA nephropathy, IgM nephropathy, Focal Segmental Glomerulo sclerosis and nodular glomerulopathy (Table 2). These infarcts have been described in various vascular distributions.

Discussion
In this case of acute embolic stroke in the setting of NS (primary membranous glomerulopathy) with a normal coagulation profile, the initial differential diagnoses for the etiology of the embolic infarcts werecardioembolism, atherombolism and a primary hypercoagulable state. The work up for these, as outlined in the case were negative. Our standard hypercoagulable panel was normal in this case, butthis maybe confounded by the concomitant use of steroids. Other clotting factors that are not included in the standard hypercoagulable panel may be affected due to large amounts of urinary protein loss [17]. Marsh et al reported a similar case of stroke in NS with normal coagulation profile except for activated free protein S level [5]. As Fibrinogen is an acute phase reactant and has been associated with elevations in acute stroke with uncertain prognostic value, the fibrinogen level was not checked in our case. [18,19] Increased fibrinogen levels after vascular event is associated with recurrence of stroke and MI [20]. As the likelihood of hypercoagulability secondary to NS was high on the differential, she was discharged on anticoagulation and high intensity statin. She has remained stable since then, with no further vascular events.
Thrombosis is a major complication of NS. Although both arterial and venous thromboses occur, arterial thrombosis is rare and has been described in the femoral arteries commonly [7], but not in cerebral vasculature. Venous thrombosis is more common in the adult patient population while arterial thrombosis is more common in the pediatric patient population [4]. Primary hypercoagulable states like congenital or hereditary deficiencies of protein C, protein S and antithrombin-IIIare relatively rare inherited conditions that lead to endothelial dysfunction [21].
Secondary hypercoagulable states can be associated with underlying conditions such as pregnancy, malignancy, NS or oral contraceptive use [21]. Hypercoagulable states result from the imbalance between the pro-coagulant and anticoagulant factors. The primary glomerular defect in NS results in leakage of high amount of high molecular weight protein, which consist many hemostatic regulatory proteins [22,23]. The overall hypoproteinemia is compensated by increased hepatic synthesis of high molecular weight clotting factors V, VII, VIII and X [24,25]. Increased urinary excretion of natural anticoagulant protein S, anti-thrombin III [26,27] has been reported.
Taken together, the net hemostatic balance is shifted towards a pro-coagulable state. As steroids may increase the concentration of anti-thrombin III and factor VIII [10], the levels of these clotting factors can be normal in NS patients taking steroids. Furthermore, diuretics can also lead to hypercoagulability due to hypovolemia and hemoconcentration. NS is also associated with thrombocytosis and platelet hyperaggregability [25]. In addition, immunologically mediated glomerular damage triggers extrinsic coagulation pathway and thus hypercoagulability [28]. Our review of current literature suggests that most of the acute stroke cases in NS are amongst young, predominantly male patients, and have relatively fewer other vascular risk factors. Hypercoagulable panels were not consistently abnormal, which is indicative of the limitations of current standard laboratory testing for this type of patients.
Conclusion
In patients with cryptogenic ischemic stroke with concomitant nephrotic syndrome, anticoagulation for the secondary prevention of stroke and other thrombo-embolic events should be considered. Future prospective or randomized trials are needed to evaluate the link between NS and acute stroke as well as efficacy of anticoagulation therapy
References
- Kendall Alan G, Reinhard C Lohmann, John B Dossetor (1971) "Nephrotic syndrome: a hypercoagulable state. Arch Intern Med 127(6): 1021-1027.
- Llach F (1985) Hypercoagulability, renal vein thrombosis, and other thrombotic complications of nephrotic syndrome. Kidney Int 28(3): 429-439.
- Mahmoodi BK, Ten Kate MK, Waanders F, Veeger NJ, Brouwer JL, et al. [2008) High Absolute Risks and Predictors of Venous and Arterial Thromboembolic Events in Patients With Nephrotic Syndrome Results From a Large Retrospective Cohort Study. Circulation 117[2): 224-230.
- Orth Stephan R, Eberhard Ritz [1998) The nephrotic syndrome.” New England Journal of Medicine 338(17): 1202-1211.
- Marsh EE, Jose Biller, Harold P Adams, Jeffrey M Kaplan (1991) Cerebral infarction in patients with nephrotic syndrome. Stroke 22(1): 90-93.
- Fuh JL, Teng MM, Yang WC, Liu HC (1992) Cerebral infarction in young men with nephrotic syndrome. Stroke 23(2): 295-297.
- Iwaki, Hirotaka, Masaru Kuriyama, Shuichiro Neshige, Shinichi Takeshima, Takahiro Himeno, et al. (2015) Acute ischemic stroke associated with nephrotic syndrome: Incidence and significance— Retrospective cohort study. eNeurologicalSci 1[3): 47-50.
- Lopez-Yunez, Alfredo M, and Jose Biller (2001) Nephrotic syndrome and stroke. Uncommon Causes of Stroke. Cambridge University Press: Cambridge, UK, pp. 177-189.
- Ueda N, Kawaguchi S, Niinomi Y, Nonoda T, Matsumoto J, et al. (1987) Effect of corticosteroids on coagulation factors in children with nephrotic syndrome. Pediatric Nephrology 1(3): 286-289.
- Sasaki Y, Raita Y, Uehara G, Higa Y, Miyasato H [2014) Carotid thromboembolism associated with nephrotic syndrome treated with dabigatran.” Case Reports in Nephrology and Dialysis 4[1): 42-52.
- Leno C, Pascual J, Polo JM, Berciano J, Sedano C (1992) Nephrotic syndrome, accelerated atherosclerosis, and stroke. Stroke 23(6): 921922.
- De Gauna RR, Alcelay LG, Conesa MJ, Asarta AP [1996) Thrombosis of the posterior inferior cerebellar artery secondary to nephrotic syndrome. Nephron 72(1): 123-123.
- Nandish, Shailesh S, Romesh Khardori, Elamin M Elamin [2006) Transient ischemic attack and nephrotic syndrome: Case report and review of literature. Am J Med Sci 332(1): 32-35.
- Yeh SM1, Lee JJ, Hung CC, Chen HC (2011) Acute cerebral infarction in a patient with nodular glomerulopathy-Atypical features and differential diagnosis. Kaohsiung J Med Sci 27(1): 39-44.
- Babu A, Boddana P, Robson S, Ludeman L [2013) Cerebral infarction in patient with minimal change nephrotic syndrome. Indian journal of nephrology 23(1): 51-53.
- Gigante A, Barbano B, Liberatori M, Sardo L, Gasperini ML, et al. (2013) Nephrotic syndrome and stroke. Int J Immunopathol Pharmacol 26(3): 769-772.
- Vaziri ND (1983) Nephrotic syndrome and coagulation and fibrinolytic abnormalities. Am J Nephrol 3(1): 1-6.
- Bots ML, Nikitin Y, Salonen JT, Elwood PC, Malyutina S, et al. (2002) Level of fibrinogen and risk of fatal and non-fatal stroke. EUROSTROKE: a collaborative study among research centers in Europe. J Epidemiol Community Health 56 suppl 1: Í8-Í13.
- Di Napoli, Mario, Francesca Papa, Vittorio Bocola (2001) Prognostic influence of increased C-reactive protein and fibrinogen levels in ischemic stroke. Stroke 32(1): 133-138.
- Rothwell PM, Howard SC, Power DA, Gutnikov SA, Algra A, et al. (2004) Fibrinogen concentration and risk of ischemic stroke and acute coronary events in 5113 patients with transient ischemic attack and minor ischemic stroke. Stroke 35(10): 2300-2305.
- Nachman RL, Silverstein R (1993) Hypercoagulable states.” Annals of Internal Medicine 119(8): 819-827.
- Eddy AA, Symons JM Symons (2003) Nephrotic syndrome in childhood.” The Lancet 362(9384): 629-639.
- Valentini Rudolph P, William E Smoyer (2007) Nephrotic syndrome. Clinical pediatric nephrology, p. 2.
- Schlegel Nicole (1996) Thromboembolic risks and complications in nephrotic children.” Seminars in thrombosis and hemostasis 23(3): 271-280.
- Kerlin, Bryce A, Rose Ayoob, William E Smoyer (2012) Epidemiology and pathophysiology of nephrotic syndrome-associated thromboembolic disease. Clin J Am Soc Nephrol 7(3): 513-520.
- Hanevold CD, Lazarchick J, Constantin MA, Hiott KL, Orak JK (1996) Acquired free protein S deficiency in children with steroid resistant nephrosis.” Annals of Clinical & Laboratory Science 26(3): 279-282.
- Remuzzi G, Mecca G, Marchesi D, Livio M, de Gaetano G (1979) Platelet hyperaggregability and the nephrotic syndrome. Thromb Res 16(3-4): 345-354.
- Kanfer A (1970) Coagulation studies in 45 cases of nephrotic syndrome without uremia.” Thrombosis et diathesis haemorrhagica 24(3): 562.






























