Abstract
The growing geriatric population presents unprecedented challenges for dental practitioners regarding medication safety and polypharmacy management. This comprehensive review examines academic literature published between 2015 and 2025, incorporating the 2023 American Geriatrics Society Beers Criteria, to analyze medication safety considerations in geriatric dental practice. With elderly patients taking an average of 4±3 medications per individual and experiencing polypharmacy rates of 94%, understanding drug interactions, age-related pharmacological changes, and potentially inappropriate medications (PIMs) is crucial for safe dental care. This review synthesizes current evidence on drug-drug interactions, xerostomia prevalence, anticoagulation management, and prescribing protocols specific to elderly dental patients. Key findings reveal that 45.7% of dental patients have preexisting diseases, with drug-drug interactions occurring in 40.7% of cases, including 2.3% major, 25.0% moderate, and 13.4% minor interactions. The 2023 Beers Criteria identifies specific medications that dental practitioners should avoid or use with caution in elderly patients. Xerostomia affects 62.5% of elderly patients using polypharmacy, particularly those using antihypertensive medications, significantly impacting oral health outcomes. Evidence-based recommendations include systematic medication reconciliation, implementation of clinical decision support systems, and adoption of modified prescribing protocols that consider age-related pharmacokinetic changes. This review provides dental practitioners with comprehensive, evidence-based guidance for ensuring medication safety in the rapidly expanding geriatric patient population.
Keywords:Geriatric dentistry; Polypharmacy; Medication safety; Beers criteria; Drug interactions
Introduction
The demographic transition toward an aging population fundamentally challenges contemporary dental practice, particularly regarding medication safety and polypharmacy management [1,2]. Comprehensive geriatric assessment has emerged as a critical framework for evaluating complex oral problems in older adults across multiple dimensions, including systemic conditions, dependency levels, and medication-related risks [3]. The intersection of physiological aging, multiple comorbidities, and extensive pharmacological interventions creates a complex clinical environment where medication errors and adverse drug events can have profound consequences for elderly dental patients.
Age-related physiological changes significantly alter drug pharmacokinetics and pharmacodynamics, affecting absorption, distribution, metabolism, and elimination of medications commonly used in dental practice [4,5]. These changes, combined with the high prevalence of polypharmacy among elderly patients, substantially increase the risk of adverse drug reactions and drug-drug interactions during dental treatment [6,7]. Studies demonstrate that 68-95% of persons 65 years or older take medication, with elderly patients averaging 1.4 to 4.3 drugs per individual, and polypharmacy rates reaching 94% in dental patient populations [6,7].
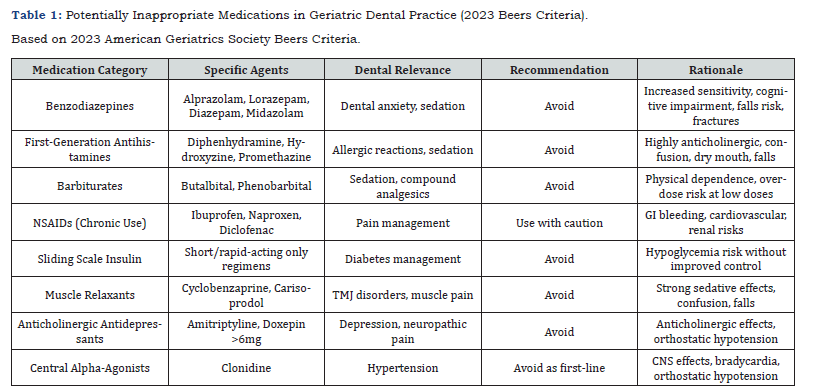
The American Geriatrics Society’s 2023 Beers Criteria provides essential guidance for identifying potentially inappropriate medications in older adults, offering explicit recommendations for drugs that should typically be avoided in elderly patients or used under specific circumstances [8,9]. This updated framework addresses medications commonly encountered in dental practice, including benzodiazepines, NSAIDs, and anticholinergic agents, providing evidence-based recommendations for safer prescribing practices [3,8]. However, specific guidelines for medication management in dental settings remain limited, highlighting the critical need for comprehensive protocols tailored to geriatric dental practice.
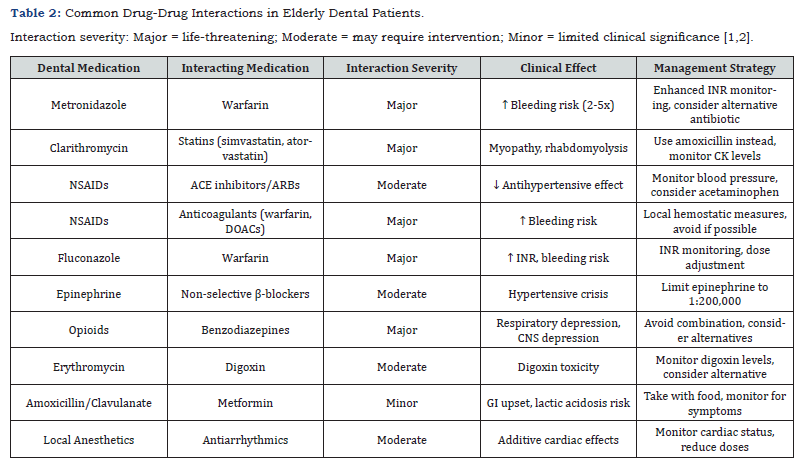
Drug-drug interactions represent a significant safety concern in elderly dental patients, with recent studies revealing interaction rates of 40.7% among dental patients, including potentially dangerous major interactions in 2.3% of cases [2]. Common interaction patterns involve dental medications such as antibiotics, analgesics, and local anesthetics with cardiovascular medications, anticoagulants, and central nervous system drugs frequently prescribed to elderly patients [2,6]. These interactions can lead to serious complications, including bleeding episodes, cardiovascular instability, and central nervous system depression.
Medication-induced xerostomia emerges as a particularly problematic consequence of polypharmacy in elderly dental patients, affecting 62.5% of those using multiple medications [7,10]. This condition significantly impacts oral health outcomes, increasing the risk of dental caries, periodontal disease, and oral infections while complicating dental treatment planning and prosthetic management [7,10]. The cumulative effect of multiple xerostomia-inducing medications creates synergistic reductions in salivary flow, particularly among patients using antihypertensive medications [2,7].
Methods
A comprehensive systematic review was conducted to examine polypharmacy and medication safety in geriatric dental practice, following established guidelines for literature review methodology [11]. The search strategy encompassed peer-reviewed academic literature published between 2015 and 2025, with particular emphasis on studies incorporating the 2023 American Geriatrics Society Beers Criteria and evidence-based medication safety protocols.
Literature Search Strategy
Electronic databases including PubMed/MEDLINE, Scopus, Web of Science, and CINAHL were systematically searched using Medical Subject Heading (MeSH) terms and keywords related to geriatric dentistry, medication safety, polypharmacy, and drug interactions [1]. Primary search terms included combinations of “geriatric dentistry,” “medication safety,” “polypharmacy,” “drug interactions,” “elderly patients,” “Beers criteria,” “potentially inappropriate medications,” and “dental prescribing” [1,2,6]. Additional searches targeted specific medication classes commonly used in dental practice, including local anesthetics, analgesics, antibiotics, and their interactions with medications frequently prescribed to elderly patients [12-14].
Boolean operators were employed to combine search terms effectively, with filters applied for human participants aged 65 years and older, English language publications, and study designs including randomized controlled trials, observational studies, systematic reviews, and meta-analyses [1]. The search was supplemented by manual review of reference lists from included articles to identify additional relevant publications and ensure comprehensive coverage of the topic.
Inclusion and Exclusion Criteria
Inclusion criteria encompassed peer-reviewed articles, systematic reviews, clinical trials, and observational studies focusing on medication safety considerations in elderly dental patients aged 65 years and older [1,2,6]. Studies were included if they addressed age-related pharmacokinetic and pharmacodynamic changes, drug interactions relevant to dental practice, polypharmacy effects on oral health, or safety protocols for geriatric dental care [4,7,15]. Additional inclusion criteria required studies to provide quantitative data on medication use patterns, drug interaction frequencies, or clinical outcomes related to medication safety in dental settings.
Exclusion criteria included case reports with fewer than 10 patients, studies focusing solely on pediatric or young adult populations, non-English language publications, and studies conducted exclusively in non-dental healthcare settings without relevance to oral health [1]. Studies older than 2015 were excluded unless they provided essential background information or historical context for current practices.
Evidence Synthesis and Quality Assessment
The review incorporated evidence from clinical practice guidelines, including the 2023 American Geriatrics Society Beers Criteria for Potentially Inappropriate Medication Use in Older Adults, antimicrobial stewardship guidelines for dental practice, and evidence-based pain management recommendations for elderly patients [8,12,14]. Quality assessment of included studies followed established criteria for evaluating methodological rigor, relevance to elderly populations, and applicability to dental practice settings [1,11].
Data extraction focused on medication use patterns, drug interaction frequencies, xerostomia prevalence, prescribing protocols, and clinical outcomes related to medication safety in elderly dental patients [2,6,7]. Particular attention was given to studies examining the implementation of medication reconciliation processes, clinical decision support systems, and quality improvement interventions targeting medication safety in dental practice [1,12,16].
Results
Demographics and Medication Use Patterns
Recent studies examining elderly dental patients reveal significant demographic and clinical characteristics that impact medication safety considerations [1,2,6]. A comprehensive analysis of 105 dental patients found that 45.7% had preexisting diseases, with cardiovascular diseases being most prevalent at 19.0% [2]. The most common dental diagnoses included apical lesions (47.6%) and tooth extractions (53.3%), indicating frequent exposure to pharmacotherapy in dental settings [2].
Polypharmacy prevalence among elderly dental patients ranges from 68-95%, with studies consistently demonstrating high medication use rates [6,7]. Brazilian research involving 96 elderly patients found an average medication consumption of 4±3 medications per individual, with polypharmacy significantly associated with xerostomia but not dysgeusia [2,7]. Cross-sectional studies in dental settings report polypharmacy rates of 94%, substantially higher than community-dwelling elderly populations [6].
The most commonly prescribed medications among elderly dental patients include antihypertensive agents, with valsartan used by 36% of patients, atorvastatin by 31.3%, and metformin by 30% [6]. Cardiovascular medications, particularly antihypertensives and diuretics, represent the largest therapeutic category, followed by diabetes medications and lipid-lowering agents [7]. This medication profile creates significant challenges for dental practitioners due to the high potential for drug interactions and oral health complications (Table 1).
Drug-Drug Interactions in Dental Practice
Comprehensive analysis of drug-drug interactions in elderly dental patients reveals alarming rates of potentially dangerous combinations [2,6]. A cross-sectional study of 150 elderly patients visiting dental clinics identified 212 drug interactions among commonly prescribed dental medications, with 21.7% classified as minor, 68.3% as moderate, and 9.9% as major interactions [6]. More recent research examining 105 dental patients found drug interactions in 40.7% of cases, with 2.3% major, 25.0% moderate, and 13.4% minor interactions [2].
The most clinically significant interactions involve anticoagulants, NSAIDs, and antibiotics commonly prescribed in dental practice. Warfarin interactions with metronidazole, clarithromycin, and azole antifungals represent particularly dangerous combinations that can lead to significant bleeding complications [2,6,15]. However, evidence supports continuing anticoagulation during most dental procedures when INR levels remain within therapeutic ranges, as the thrombotic risk of discontinuation often outweighs bleeding risks [15].
NSAID interactions with cardiovascular medications present another major concern, particularly in elderly patients with multiple comorbidities [6,12,13]. These interactions can antagonize antihypertensive effects, increase bleeding risk when combine with anticoagulants, and cause nephrotoxicity, especially in patients with compromised renal function [6,12]. Age-specific analysis reveals that patients aged 31-60 years experienced 61.3% of major drug interactions, while those ≥61 years faced 38.7%, highlighting the complex relationship between age and medication interaction risk [2] (Table 2).
Xerostomia and Medication-Induced Oral Complications
Medication-induced xerostomia represents a significant clinical challenge in elderly dental patients, with prevalence rates reaching 62.5% among those using polypharmacy [7]. This condition directly correlates with the number of medications used, particularly anticholinergic agents and antihypertensive medications [10]. Research demonstrates that polypharmacy is significantly associated with xerostomia (p<0.05), with antihypertensive medications showing the strongest correlation [7,10].
The clinical impact of medication-induced xerostomia extends beyond patient comfort, significantly affecting oral health outcomes and dental treatment planning [10]. Reduced salivary flow increases the risk of dental caries, periodontal disease, and oral infections while complicating denture retention and oral hygiene maintenance [7]. Over 400 medications can cause salivary dysfunction, with the cumulative effect of multiple xerostomia-inducing medications creating synergistic reductions in salivary flow [7].
Anticholinergic burden assessment reveals that patients with anticholinergic burden scores ≥1 demonstrate significantly higher rates of hyposalivation (61.0%) compared to those with no anticholinergic burden (6.8%) [7]. This finding emphasizes the importance of comprehensive medication review and consideration of cumulative anticholinergic effects when planning dental treatment for elderly patients [10].
Potentially Inappropriate Medications in Dental Practice
Application of the 2023 American Geriatrics Society Beers Criteria to dental practice reveals significant opportunities for medication optimization in elderly patients [3,8]. Studies utilizing Beers Criteria assessment found that more than 30% of older adults visiting dentists were prescribed potentially inappropriate medications, with benzodiazepines and long-acting NSAIDs being among the most commonly prescribed inappropriate drugs [3].
The 2023 Beers Criteria specifically addresses medications commonly used in dental practice, including first-generation antihistamines, benzodiazepines, barbiturates, and certain analgesics. These medications are flagged due to increased risks of falls, cognitive impairment, and adverse drug events in elderly patients [8,17]. Benzodiazepines, frequently prescribed for dental anxiety, carry strong recommendations for avoidance due to increased sensitivity in older adults and risks of cognitive impairment, delirium, falls, and fractures [8].
NSAIDs, while recommended as first-line therapy for dental pain in younger adults, require careful consideration in elderly patients due to increased risks of cardiovascular, gastrointestinal, and renal complications [12,13,18]. The 2024 ADA guideline acknowledges these concerns while maintaining NSAID recommendations, emphasizing the need for individualized risk-benefit assessment in elderly patients [12, 13].
Emergency Department Utilization and Medication Safety
Emergency department visits related to medication errors in elderly dental patients represent a significant public health concern [1,19,20]. Systematic review evidence demonstrates that older adults receiving dental opioids have 23% higher emergency department visit rates when concurrently taking incompatible medications [20]. Prescription overlaps lasting more than three days increase hospitalization risk by 47%, highlighting the importance of careful medication coordination [1].
Emergency department-based geriatric medication safety programs show promising results for improving medication management [20]. Studies demonstrate that multidisciplinary teams including clinical pharmacists and geriatricians achieve significant improvements in potentially inappropriate medication deprescribing, with clinical pharmacist reviews resulting in 32% reduction in PIMs [1]. Computerized clinical decision support systems show even greater impact, with studies reporting 40% reduction in PIM ordering when implemented in emergency departments [20].
These findings have direct implications for dental practice, as they demonstrate the effectiveness of systematic medication review processes and clinical decision support systems in reducing medication-related adverse events [20]. Implementation of similar systems in dental practice could significantly improve medication safety outcomes for elderly patients [12,16].
Medication Reconciliation and Safety Interventions
Research on medication reconciliation processes in dental practice reveals significant opportunities for improving medication safety [21]. A prospective study of 130 dental patients found 618 medication discrepancies among 860 reported medications, with medication omission being the most common error (71.7%). Of omitted medications, 64.6% had potential oral adverse effects, 7.9% could interact with local anesthetics or vasoconstrictors, and 19.1% had potential bleeding effects [12].
Pharmacist-led intervention studies demonstrate significant improvements in medication reconciliation accuracy [12]. Implementation of structured medication review processes, including interactive software content within electronic medical records and mandatory educational sessions for dental providers, resulted in significant reductions in medication discrepancies and omissions [12]. These interventions prove that systematic approaches to medication reconciliation can effectively improve medication safety in dental practice settings [21].
Comprehensive geriatric assessment tools have been developed specifically for dental practice, incorporating medication review as a critical component [3,6]. These tools include assessment of dependency levels, cognitive function, fall risk, and medication burden, providing a framework for individualized treatment planning that considers medication safety [6]. Expert consensus emphasizes that dependency level, social support, and systemic factors, including medication effects, are critical for selecting appropriate levels of dental care [3].
Discussion
Age-Related Pharmacological Considerations
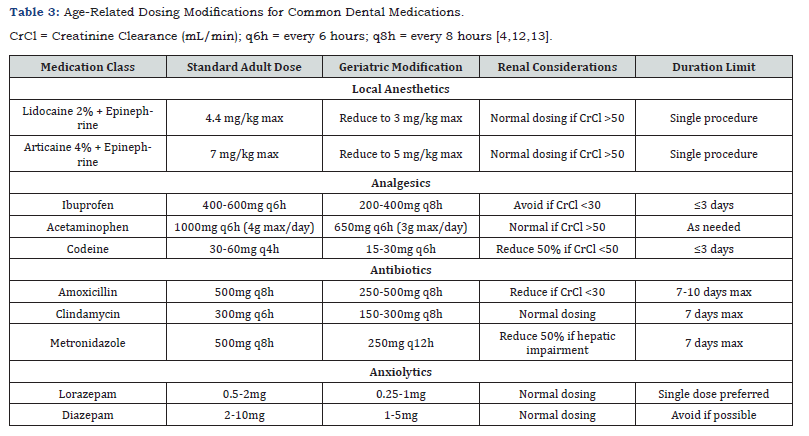
The physiological changes associated with aging create fundamental alterations in drug handling that significantly impact medication safety in dental practice [4]. Pharmacokinetic changes include decreased hepatic blood flow and reduced cytochrome P450 enzyme activity, resulting in prolonged drug half-lives and increased accumulation risk for medications commonly used in dentistry [4,5]. Local anesthetic studies in elderly patients demonstrate significantly lower clearance and volume of distribution compared to younger individuals, though routine dosage adjustments may not be necessary for standard dental procedures [4].
Pharmacodynamic changes present equally important considerations, with elderly patients demonstrating increased sensitivity to central nervous system medications [4]. This enhanced sensitivity has direct implications for sedation protocols, analgesic prescribing, and the use of medications with anticholinergic properties [5]. The cumulative effect of multiple medications with similar mechanisms of action can produce synergistic adverse effects that exceed the sum of individual drug effects [7,10].
Renal function decline represents perhaps the most clinically significant pharmacokinetic change, with glomerular filtration rate decreasing approximately 1% per year after age 40 [4]. This progressive decline necessitates dose adjustments for renally eliminated medications, including some antibiotics commonly prescribed in dental practice [4,5]. Failure to account for reduced renal function can lead to drug accumulation and increased toxicity risk.
Clinical Decision Support and Technology Integration
The development of clinical decision support systems specifically designed for geriatric dental treatment shows promising results for improving medication safety [16]. Bayesian network models incorporating patient demographics, medical history, and medication profiles achieve F1-scores of 89.31% for therapeutic plan recommendations. These systems provide general practitioners with expert-level decision support, helping identify potentially inappropriate medications and drug interactions before prescribing dental medications [16].
The integration of technology-based solutions addresses the complexity of medication management in elderly dental patients by providing real-time decision support at the point of care [16]. Interactive software content within electronic medical records can guide dental providers through systematic medication reconciliation processes, reducing the likelihood of overlooking important drug interactions or contraindications [12]. These technological interventions complement clinical expertise by providing comprehensive databases of drug interactions and dosing recommendations specific to elderly patients (Table 3).
Emergency department studies demonstrate the effectiveness of computerized clinical decision support systems in reducing potentially inappropriate medication use, with 40% reductions in PIM ordering reported when these systems are properly implemented [20]. Similar technology could be adapted for dental practice settings, providing alerts for drug interactions, dosing recommendations based on renal function, and guidance on appropriate medication selection for elderly patients [1,16].
Anticoagulation Management in Dental Practice
Management of anticoagulated elderly patients requires careful balance between bleeding and thrombotic risks [15,22]. Current evidence strongly supports continuing anticoagulation for most dental procedures when patients maintain therapeutic anticoagulation levels [22]. Studies consistently demonstrate that the thrombotic risk associated with anticoagulation discontinuation typically exceeds the bleeding risk of continuing therapy during dental procedures [15].
Recent research comparing different anticoagulant classes reveals important safety considerations for elderly patients [22]. While direct oral anticoagulants (DOACs) generally demonstrate favorable safety profiles compared to warfarin, individual patient factors must guide selection [15]. The shorter half-life of DOACs allows for more flexible perioperative management when temporary discontinuation is necessary, though this should be coordinated with prescribing physicians [15,22].
Local hemostatic measures prove effective for managing bleeding in anticoagulated patients undergoing dental procedures. These techniques, combined with careful patient selection and appropriate procedure planning, enable safe dental treatment while maintaining therapeutic anticoagulation [15]. The key principle involves avoiding unnecessary anticoagulation interruption while ensuring adequate hemostatic support during and after dental procedures.
Pain Management and Analgesic Selection
Pain management in elderly dental patients requires modified approaches that consider age-related pharmacological changes and increased comorbidity burden [18]. The 2024 ADA guideline maintains NSAIDs as first-line therapy for dental pain but acknowledges the need for careful risk-benefit assessment in elderly patients [12,13]. Alternative approaches, including acetaminophen- based regimens and multimodal pain management strategies, may provide safer options for many elderly patients [13,18].
Opioid prescribing in elderly dental patients presents particular challenges due to increased sensitivity, drug interaction potential, and abuse risk [23]. Recent evidence demonstrates concerning trends in opioid prescribing for elderly dental patients, with 10% having concurrent prescriptions for incompatible medications [14]. The implementation of prescription drug monitoring programs shows promise for reducing inappropriate opioid prescribing and identifying high-risk patients [14].
The principle of “start low, go slow” applies particularly to analgesic prescribing in elderly patients, with initial doses typically reduced to 25-50% of standard adult doses [5,23]. Duration of therapy should be minimized, with reassessment at 48-72 hours for continued need [23]. Non-pharmacological approaches should be emphasized whenever possible to minimize systemic drug exposure while maintaining effective pain control.
Antimicrobial Stewardship Considerations
Antimicrobial stewardship principles take on added importance in elderly dental patients due to increased infection risk, altered pharmacokinetics, and potential for drug interactions. Self-medication with non-prescribed antibiotics represents a growing concern among older adults, with 6.4% of elderly patients in one study admitting to self-treatment with antibiotics for symptoms such as cold or pain [24]. This practice increases the risk of inappropriate antibiotic use and potential interactions with prescribed medications.
Antibiotic selection in elderly patients requires consideration of age-related pharmacokinetic changes, comorbidities, and interaction potential. Amoxicillin remains a preferred first-line option due to its favorable safety profile, though dose adjustments may be necessary based on renal function. Alternative antibiotics should be selected carefully, avoiding agents with high interaction potential or significant adverse effect profiles in elderly patients [24].
The development of antibiotic resistance represents a particular concern in elderly populations due to frequent healthcare exposure and antibiotic use. Dental practitioners play a crucial role in antimicrobial stewardship by prescribing antibiotics judiciously, selecting appropriate agents and durations, and educating patients about proper use and completion of prescribed courses [24].
Quality Improvement and Safety Systems
Implementation of systematic quality improvement initiatives targeting medication safety in elderly dental patients shows significant promise for reducing adverse events [20]. Medication reconciliation programs demonstrate measurable improvements in medication accuracy, with pharmacist-led interventions reducing discrepancies and omissions [12]. These programs prove particularly valuable in dental practice settings where patients may receive care from multiple providers without centralized medication management.
Multidisciplinary approaches to medication safety yield superior outcomes compared to single-provider interventions [1]. Studies demonstrate that teams including clinical pharmacists, geriatricians, and dental providers achieve greater improvements in potentially inappropriate medication deprescribing and overall medication safety [20]. This collaborative approach addresses the complexity of medication management in elderly patients while leveraging the expertise of multiple healthcare disciplines.
Continuous quality monitoring and feedback systems enable ongoing improvement in medication safety practices. Regular review of prescribing patterns, adverse event tracking, and staff education programs help maintain high standards of medication safety [11]. These systems should include mechanisms for identifying trends, implementing corrective actions, and measuring the effectiveness of safety interventions.
Conclusion
This comprehensive review of polypharmacy and medication safety in geriatric dental practice reveals significant challenges and opportunities for improving care quality in the rapidly expanding elderly population. The high prevalence of polypharmacy, reaching 94% in some dental patient populations, combined with complex drug interaction patterns affecting 40.7% of elderly dental patients, creates a clinical environment requiring specialized knowledge and systematic safety approaches.
The 2023 American Geriatrics Society Beers Criteria provides essential guidance for identifying potentially inappropriate medications in elderly dental patients, with more than 30% of older adults visiting dentists receiving at least one flagged medication. Implementation of these criteria, combined with systematic medication reconciliation processes, offers evidence-based strategies for reducing medication-related adverse events in dental practice.
Medication-induced xerostomia, affecting 62.5% of elderly patients using polypharmacy, represents a significant clinical challenge that extends beyond patient comfort to impact fundamental oral health outcomes. The cumulative effect of multiple medications, particularly anticholinergic agents and antihypertensives, creates complex management challenges requiring coordinated care approaches and ongoing monitoring.
Evidence-based interventions, including clinical decision support systems, pharmacist-led medication reconciliation, and multidisciplinary care teams, demonstrate significant improvements in medication safety outcomes. These approaches achieve reductions in potentially inappropriate medication use, decreased emergency department utilization, and improved overall safety profiles for elderly dental patients.
The evolving landscape of geriatric dental care requires continued investment in education, technology, and quality improvement initiatives. As the elderly population continues to expand, dental practitioners must be prepared to provide safe, effective care that addresses the unique medication-related challenges of this vulnerable population. Through implementation of evidence- based safety protocols, utilization of clinical decision support tools, and commitment to continuous quality improvement, dental teams can significantly improve outcomes while minimizing medication-related risks for elderly patients.
Future research priorities should focus on developing standardized protocols for medication management in dental practice, evaluating the effectiveness of technology-based interventions, and establishing outcome measures for medication safety in elderly dental patients. Long-term studies examining the impact of systematic medication safety interventions on clinical outcomes, quality of life, and healthcare utilization will provide valuable evidence for optimizing care delivery in this growing population.
References
- Carrasco LA, Polk DE, Urquhart O, Aghaloo T, Claytor JW, et al. (2024) Evidence-based clinical practice guideline for the pharmacologic management of acute dental pain in adolescents, adults, and older adults. The Journal of the American Dental Association 155(2): 102-117.
- By the American Geriatrics Society Beers Criteria® Update Expert Panel (2023) American Geriatrics Society 2023 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. Journal of the American Geriatrics Society 71(7): 2052-2081.
- Guimarães DdM, Parro YM, Muller HS, Coelho EB, Martins VdP, et al. (2023) Xerostomia and dysgeusia in the elderly: prevalence of and association with polypharmacy. Brazilian Journal of Oral Sciences 22: e236637.
- Zhao X, Luo J, Pan X, Fang L, Liu C (2025) Efficacy and safety of anticoagulants in elderly atrial fibrillation patients: a systematic review and network meta-analysis. BMC Cardiovascular Disorders 25(1): 396.
- Waldinger R, Weinberg G, Gitman M (2020) Local Anesthetic Toxicity in the Geriatric Population. Drugs & Aging 37(1): 1-9.
- Wongiam N, Praditpornsilpa K, Vacharaksa A (2025) Comprehensive geriatric assessment for oral care in older adults: a focus group study. BMC Geriatrics 25(1): 232.
- Madej B, Glassberg RA (2025) Navigating medication risks in elderly patients: Essential tips for dental hygienists RDH Magazine.
- Abbaszadeh E, Ganjalikhan HN, Rad M, Torabi M (2022) Drug-Drug Interactions in Elderly Adults in Dentistry Care: a Cross-Sectional Study. J Dent (Shiraz) 23(4): 459-466.
- Roberts EP, Roberts BS, Burns A, Goodlet KJ, Chapman A, et al. (2020) Prevalence and dental professional awareness of antibiotic self-medication among older adults: Implications for dental education. Journal of Dental Education 84(10): 1126-1135.
- Colibășanu D, Ardelean SM, Goldiș FD, Drăgoi MM, Vasii SO, et al. (2025) Unveiling Drug-Drug Interactions in Dental Patients: A Retrospective Real-World Study. Dentistry Journal 13(6): 255.
- Dézsi CA, Bence DB, Dézsi AD (2017) Management of dental patients receiving antiplatelet therapy or chronic oral anticoagulation: A review of the latest evidence. European Journal of General Practice 23(1): 197-202.
- Pergolizzi JV, Peter M, Ann LJ, Christopher G, Varrassi G (2020) The pharmacological management of dental pain. Expert Opinion on Pharmacotherapy 21(5): 591-601.
- Wehler CJ, Panchal NH, Cotchery DL, Farooqi OA, Ferguson DK, et al. (2021) Alternatives to opioids for acute pain management after dental procedures: A Department of Veterans Affairs consensus paper. The Journal of the American Dental Association 152(8): 641-652.
- Skaar DD, O Connor HL (2012) Use of the Beers criteria to identify potentially inappropriate drug use by community-dwelling older dental patients. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology 113(6): 714-721.
- Thanathornwong B, Suebnukarn S, Ouivirach K (2023) Clinical Decision Support System for Geriatric Dental Treatment Using a Bayesian Network and a Convolutional Neural Network. hir. 29(1): 23-30.
- Crighton AJ, McCann CT, Todd EJ, Brown AJ (2020) Safe use of paracetamol and high-dose NSAID analgesia in dentistry during the COVID-19 pandemic. British Dental Journal 229(1):15-18.
- Hung PL, Chen JY, Chen MT, Li PL, Li WC, et al. (2019) The impact of a medication reconciliation programme at geriatric hospital admission: A pre-/postintervention study. British Journal of Clinical Pharmacology 85(11): 2614-2622.
- Choi HJ, Stewart AL, Tu C (2017) Medication discrepancies in the dental record and impact of pharmacist-led intervention. International Dental Journal 67(5): 318-325.
- Shoaee S, Heydari MH, Hessari H, Mehrdad N, Khalilazar L, et al. (2023) Development and initial validation of the Comprehensive Geriatric Oral Health Assessment Tool. Clinical and Experimental Dental Research 9(5): 879-886.
- Teoh L, McCullough MJ, Moses G (2022) Preventing medication errors in dental practice: An australian perspective. Journal of Dentistry 119: 104086.
- Sarasin DS, Brady JW, Stevens RL (2020) Medication Safety: Reducing Anesthesia Medication Errors and Adverse Drug Events in Dentistry Part 2. Anesth Prog 67(1): 48-59.
- Skains RM, Hayes JM, Selman K, Zhang Y, Thatphet P, et al. (2025) Emergency Department Programs to Support Medication Safety in Older Adults: A Systematic Review and Meta-Analysis. JAMA Network Open 8(3): e250814-e.
- Mair A (2019) Medication safety in polypharmacy: technical report.
- Budnitz DS, Shehab N, Lovegrove MC, Geller AI, Lind JN, et al. (2021) US Emergency Department Visits Attributed to Medication Harms, 2017-2019. JAMA 326(13): 1299-1309.






























