The Prevalence of Myocardial Injury After Noncardiac Surgery (MINS) and the Correlation with 30-day Outcomes and Frailty in Vascular Surgery
Poh Chua1, Kien Chan1, Dale Currigan2, Lucy Stopher3, Warren D Raymond4, Shirley Jansen3,4,5 and Charles A Inderjeeth1,4,5*
1Department of Geriatric Acute and Rehabilitation Medicine, Sir Charles Gairdner, and Osborne Park Hospital
2Department of Anaesthetics, Sir Charles Gairdner Hospital
3Department of Vascular and Endovascular Surgery, Sir Charles Gairdner Hospital
4University of Western Australia, Perth, Western Australia
5Curtin University, Perth, Western Australia
Submission: October 09, 2023; Published: October 27, 2023
*Corresponding author: Charles Inderjeeth, Department of Geriatric Acute and Rehabilitation Medicine, Sir Charles Gairdner & Osborne Park Healthcare Group, Hospital Avenue, Nedlands, Western Australia
Email: Charles.inderjeeth@health.wa.gov.au
How to cite this article: Poh Chua, Kien Chan, Dale Currigan, Lucy Stopher, Warren D Raymond, Shirley Jansen and Charles A Inderjeeth*. The Prevalence of Myocardial Injury After Noncardiac Surgery (MINS) and the Correlation with 30-day Outcomes and Frailty in Vascular Surgery. OAJ Gerontol & Geriatric Med. 2023; 7(4): 555720. DOI: 10.19080/OAJGGM.2023.07.555720
Abstract
Objective:
To determine the prevalence of Myocardial Injury after Non-cardiac Surgery (MINS) in patients who underwent major vascular intervention, the association of MINS with post-surgical complications, and to assess the prognostic value of utilising the Rockwood Clinical Frailty Scale (CFS) and Reversed Cardiac Index Score (RCRI) in MINS.
Methods:
Patients aged 50 years or older undergoing major vascular intervention were included. High sensitivity cardiac troponin was measured preoperatively and on day 1, 2 and 3 postoperatively. Patients were followed for 30 days and scored using the CFS and RCRI.
Results:
127 patients were included (mean age 71.0 ± 10.1, 70.1% females). 40.9% (n=52/127) had MINS; 75% were asymptomatic. MINS group had more premorbid coronary artery disease, heart failure, atrial fibrillation, and diabetes. A higher proportion had MINS in the urgent/emergency surgery (P=0.002) and carotid endarterectomy surgery (P=0.021) groups. MINS group had an increased median length of stay (9 days vs 6 days, P=0.039) and higher 30-day adverse outcomes [34.6% vs 6.7%, P <0.001]. This included postoperative heart failure (15.4% vs 1.3%, P=0.016) and myocardial infarction (25% vs 0). Mortality was not significantly different (5.8% vs 2.7%, P=0.39. A higher proportion of patients with MINS had CFS ≥ 4 (71.2%), and RCRI ≥ 3 (51.9%).
Conclusions:
MINS is common, more frequently asymptomatic, and present in frail older patients with comorbidities undergoing vascular intervention. MINS is associated with poorer 30-day outcomes, especially cardiac complications and longer stay. Routine troponin levels may allow early identification and pre-emptive medical optimisation.
Keywords: Vascular Surgery; Emergency Surgery; Myocardial Injury; Medical Therapy
Keywords: BMT: Best Medical Therapy, CFS: Rockwood Clinical Frailty Scale, MINS: Myocardial Injury After Non-Cardiac Surgery, RCRI: Revised Cardiac Index Score, CCS: Canadian Cardiovascular Society
Introduction
Myocardial injury after noncardiac surgery (MINS) is defined by an elevation in cardiac troponin secondary to myocardial ischaemia occurring within 30-day after noncardiac surgery regardless of whether the patient has cardiac symptoms [1,2]. This definition includes patients who meet the universal criteria for myocardial infarction [3]. Previous literature has shown that MINS is common, being diagnosed in 8.0% of patients after non-cardiac surgery and 19% of patients after vascular surgery [1,2,4]. It is associated with an increased 30-day mortality (9.8% to 12.5% in MINS versus 1.1% to 1.5% in patients without MINS) [1, 2]. Concerningly, more than 50% of patients with MINS in these studies were asymptomatic [2,4]. Therefore, MINS could have been missed without routine cardiac troponin monitoring perioperatively. The International Perioperative Guidelines recommend the utilization of cardiac troponin as a cardiac biomarker screening tool to detect perioperative cardiac events and improve perioperative cardiac risk stratification [5-7].
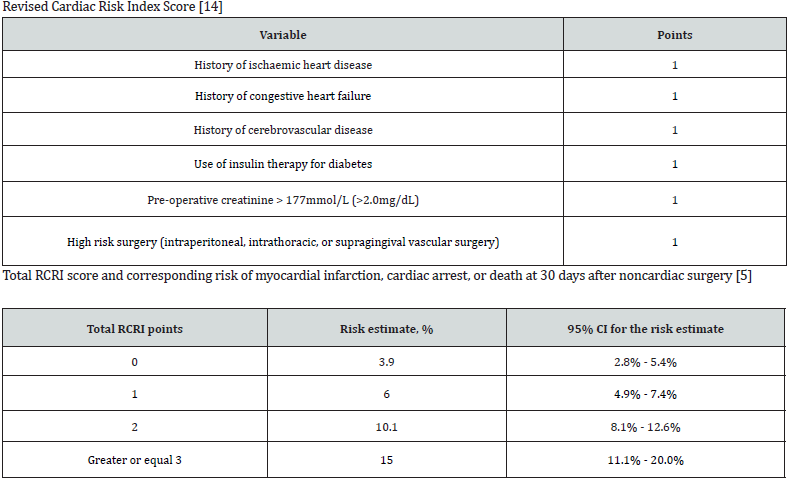
Despite the recognition of frailty as an independent and strong risk factor for adverse postoperative outcomes, the association between the frailty scores and MINS has not yet been explored [8,9]. The Canadian Cardiovascular Society (CCS) perioperative guideline recommends using the Revised Cardiac Index Score (RCRI) to evaluate perioperative cardiac risk but has not been fully validated in patients with MINS [5-7]. Our study, therefore, was designed primarily to explore the prevalence of MINS in vascular surgery patients at our tertiary institution in Perth, Western Australia, and its association with post-surgical complications within the first 30-day period, how it relates to frailty scores and the association between MINS and RCRI score.
Methods
Study Design
This was a single centre, cross-sectional, prospective follow-up study conducted at the Department of Vascular and Endovascular Surgery, Sir Charles Gairdner Hospital (SCGH) in Perth, Western Australia. This is a 600 bed tertiary teaching hospital in the North Metropolitan area. The Vascular Geriatric service in the hospital provides shared care with the vascular surgeons in patients above 50 years of age to optimize patients perioperatively, identify acute medical issues, facilitate management plans and discharge planning.
The study recruitment period was from 26th October 2019 to 26th October 2020. The inclusion criteria include patients aged above 50 years of age who underwent major vascular intervention, including endovascular aortic repair, open abdominal aortic aneurysm repair, thoracic aortic stent grafting, peripheral arterial reconstruction (i.e., femoral bypass, endarterectomy, and embolectomy), below and above-knee amputation, and extracranial cerebrovascular surgery (i.e., carotid endarterectomy, carotid-subclavian bypass and carotid body tumour removal). All participants had at least one overnight stay in the hospital after surgery. Surgeries were categorised as emergency surgery if surgery occurred within 24 hours; and as urgent surgery if it occurred between 24 to 72 hours of hospital admission. Participants were excluded if they underwent minor vascular surgery, such as toe amputation and or lower limb angioplasty, or if no postoperative blood samples could be obtained.
The high sensitivity cardiac troponin blood test (Troponin I Abbott Architect) was measured at 24 and 48 hours preoperatively and 24, 48 and 72 hours postoperatively. An elevated troponin level was defined as >26ng/L in males and >16ng/L in females [10], or the detection of a rise or fall of cardiac troponin with at least one value above the 99th percentile in a normal reference population [11]. MINS was identified in our study based on the detection of an elevated troponin level on any day between Day 1 until Day 3 and up to 30-day after surgery. In those with preoperative raised troponin, we defined MINS only if there was a further rise and fall from the preoperative baseline troponin. We conducted follow-up for 30 days to monitor for any additional troponin tests performed during this period.
Participants who had elevated troponin were assessed for cardiac ischaemic symptoms [chest, arm, neck, jaw pain or discomfort, and dyspnoea] or ECG changes [ST-segment elevation or depression, T wave inversion or the presence of pathological Q waves]. If any of these cardiac ischaemic features were present in line with positive troponin, these patients were referred to cardiology. Conversely, due to no set standardised management guidelines for patients with elevated troponin but without cardiac ischaemic symptoms or ECG changes, these patients were referred to cardiology at the discretion of the treating team or in consultation with the vascular geriatric team.
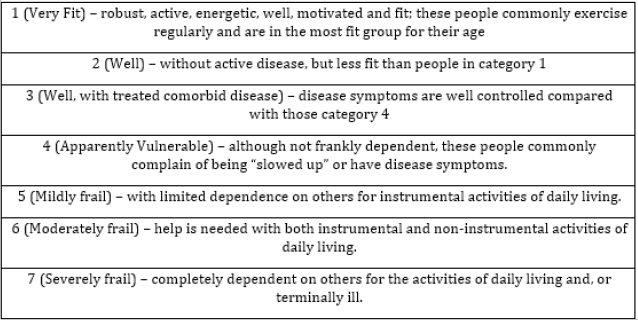
We collected data on patient demographics, baseline characteristics, co-morbidities, and medications. The definitions of each baseline characteristic are listed in (Appendix 1). Patients were scored on admission using the Rockwood Clinical Frailty Scale (CFS) (Appendix 2). We chose CFS to measure frailty as it is convenient and practical in the preoperative setting [9,12,13]. However, if there was no documented CFS during admission, the investigator calculates the CFS score by reviewing the medical records and consolidated database of electronic clinical patient information software (I-soft Clinical Manager) to identify patient demographics, pre-morbid function, medical history, and functional assessment by the allied health team.
The Revised Cardiac Index Score (RCRI) is a tool used to evaluate perioperative cardiac risk and complications [14]. The participants were scored based on the collected medical data information (baseline characteristics and comorbidities) (Appendix 3). Patients were followed up for 30-days. If the participant remained an inpatient, the outcome data was collected from face-to-face interviews, medical records, computerized blood test and imaging results. In discharged participants, 30-day outcome data was collected via a telephone interview, verified with medical records (inpatient notes, chart review, discharge summaries, pathology, and imaging results). Mortality was confirmed using the hospital electronic medical records in addition to a phone call to relatives.
Study Outcomes
The primary outcome was to assess the prevalence of MINS in vascular patients who underwent major vascular intervention.
The secondary outcomes were:
(i) The association between MINS and 30-day outcomes (fatal cardiac arrest, congestive heart failure, myocardial infarction, cardiac revascularisation, pulmonary embolism, deep vein thrombosis, stroke, and mortality).
(ii) The association between MINS and frailty using the CFS.
(iii) The association between MINS and the Revised Cardiac Risk Index (RCRI) Score
Statistical Analyses
Results were presented as a mean with standard deviation, median with interquartile range or as a frequency and proportion. Between-group differences were assessed with the t-test, Mann- Whitney U-test, Chi-square test, linear [β with 95% confidence interval (95%CI)] and logistic regression [odds ratio (OR) with 95%CI], as appropriate. The association between MINS with 30- day complications was assessed with logistic regression. The association between MINS and length of stay was assessed with univariate and multivariate linear regression adjusted for age, sex, and RCRI categories.
Ethical Consideration
The Quality Improvement team at Sir Charles Gairdner Hospital Western Australia approved this study with the Governance Evidence Knowledge and Outcome (GEKO) approval number 34014.
Results
Recruitment
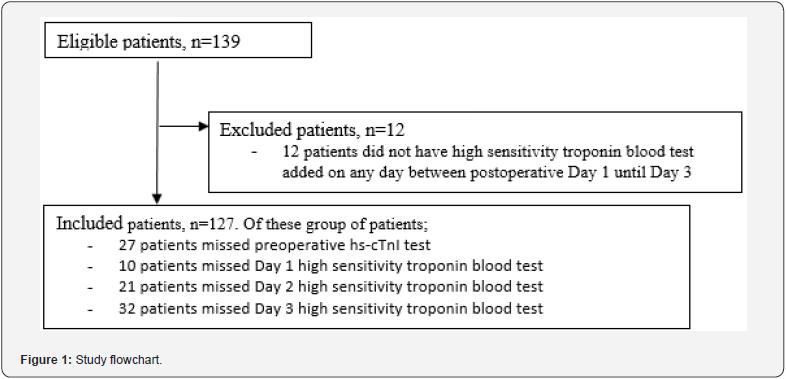
Of a total of 139 patients screened, 127 met eligibility and were included in this study (Figure 1); 12 patients were excluded because they were discharged early and there were no postoperative blood samples that could be obtained. Of the included patients, 27 patients (21.3%) did not have preoperative troponin blood tests within the 24-to-48-hour timeframe. A total of 67 patients missed one or more postoperative routine blood tests between days 1 and 3 (Figure 1) because they were discharged early.
Primary Outcome
Prevalence of MINS
Of the 127 included patients, MINS was found in 52 patients (40.9%). This included 20/21 (95.2%) patients who had an elevated troponin level preoperatively with a subsequent rise and fall in troponin level postoperatively. Of those diagnosed with MINS, 13/52 (25.0%) fulfilled the universal criteria of myocardial infarction, while the remaining 75.0% were asymptomatic.
Patient Demographics and Clinical Baseline Characteristics
(Table 1) describes patient demographics and clinical baseline characteristics for patients with and without MINS. The overall sample had a mean age of 71.0 years (standard deviation 10.1) with females accounting for 70.1%. Patients with MINS were older (mean age 73.7 years versus 69.2 years). A higher proportion of patients with MINS had premorbid coronary artery disease (n=32/52 [61.5%] vs n=25/75 [33.3%], P=0.002), congestive heart failure (n=17/52 [32.7%] vs n=10/75 [13.3%], P= 0.011), atrial fibrillation (n=17/52 [32.7%] vs n=11/75 [14.7%], P=0.018), diabetes (n= 29/52 [55.8%] vs n=17/75 [22.7%] P<0.001) and diabetes on insulin treatment (n= 13/52 [25.0%] vs n=7/75 [9.3%] P=0.021).
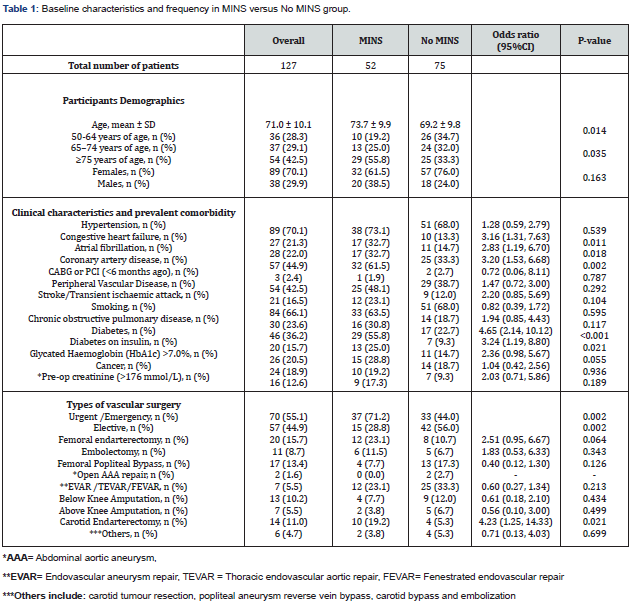
Type of Vascular Surgery
There was a higher proportion of MINS who had emergency or urgent surgery vs elective surgery. (n=37/52 [71.2%] vs n=15/52 [28.8%], P= 0.002). Carotid endarterectomy in particular was significantly associated with a high proportion of MINS (19.2%; OR 4.23, 95% CI 1.25-14.33, P=0.021 (Table 1).
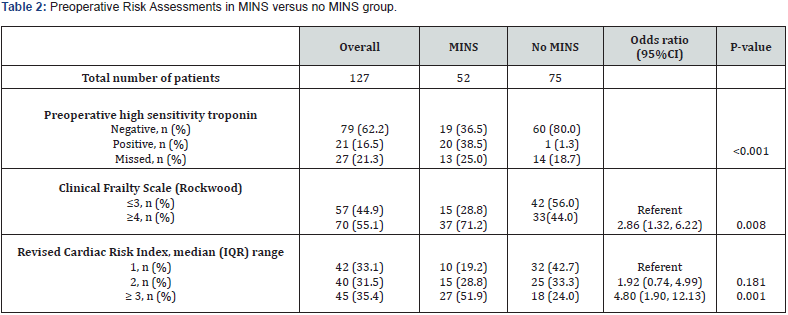
Length of Stay
MINS group had an increased median length of stay (9 days [MINS] vs 6 days [no MINS], P=0.039) (Table 2). MINS was associated with a 40% (β 0.40, 95%CI 0.11, 0.68; P=0.007) and 30% (aβ 0.30, 95%CI 0.01, 0.59; P=0.046) increased LOS in a univariate and multivariate linear regression, respectively.
Secondary Outcomes
Postoperative Complications
At 30-days, a total of 32 adverse outcomes were recorded in 23 patients, with the majority consisting of congestive heart failure and myocardial infarction (Table 3). A higher proportion of patients with MINS had 30-day adverse outcomes (n=18/52 [34.6%] vs n=5/75 [6.7%], P<0.001). This included postoperative congestive heart failure (n=8/52 [15.4%] vs n=1/75 [1.3%], P=0.016) and myocardial infarction (n=13/52 [25.0%] vs 0/75). Of the 13 patients with MINS, 12 had myocardial infarction as inpatients and 1 within one week of discharge.
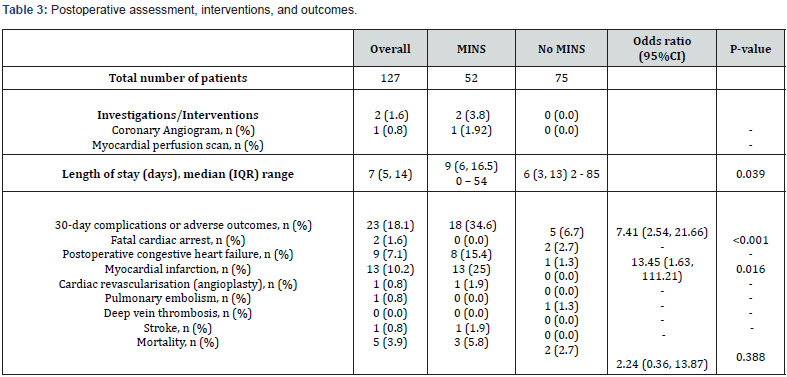
In patients with MINS diagnosed with myocardial infarction, two patients had coronary angiography. One patient had angioplasty. The second patient did not require revascularization because only mild coronary artery disease was found with less than 30% of coronary artery stenosis. One patient in the MINS group had a myocardial perfusion scan which did not show reversible perfusion defect and therefore did not require further cardiac intervention. No recorded deep vein thrombosis but one patient without MINS developed pulmonary embolism. One patient had fatal hemorrhagic stroke in the MINS group (Table 2). Overall, 30-day mortality was 5.8% (3/52) in the MINS group and 2.7% (2/75) in those without MINS (P=0.388). Three patients in the MINS group died; 2 from congestive heart failure and 1 from haemorrhagic stroke. Two patients without MINS died from fatal cardiac arrest.
Clinical Frailty Scales and Revised Cardiac Index Score
Using the Rockwood CFS, overall, 55% (n=70/127) of participants were scored as being in the vulnerable to severely frail categories (CFS 4-7) (Table 2). A higher proportion of MINS in those scoring CFS ≥ 4 (71.2% vs 44%, OR 2.86 (95% CI 1.32- 6.22), P=0.008]. (Table 2) shows that 35.4% of the participants had an RCRI score of ≥ 3. There was a higher proportion of MINS in the RCRI score of ≥ 3 [51.9% vs 24%, OR 4.80 (95%CI 1.90-12.13; p= 0.001].
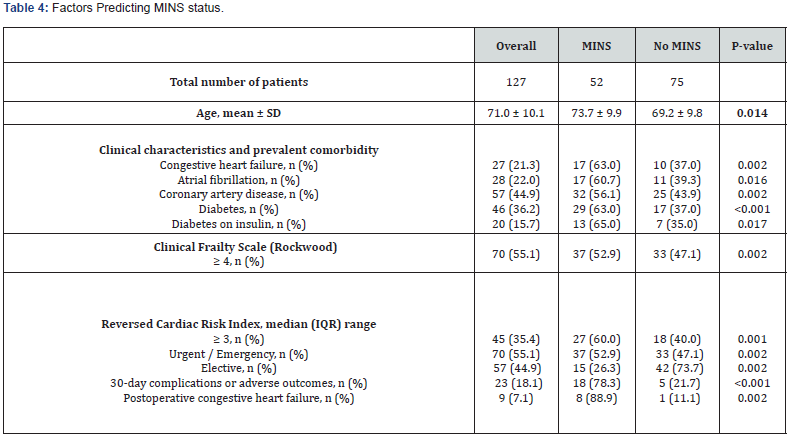
Factors Predicting MINS Status
(Table 4) summarises the predictors of MINS. It includes older age, congestive heart failure, atrial fibrillation, coronary artery disease, diabetes, diabetes on insulin treatment, urgent/ emergency surgery, patients with CFS score ≥ 4 and RCRI score ≥ 3. In turn, MINS predicts 30-day complications or adverse outcomes, and postoperative congestive heart failure.
Discussion
This single-centre study demonstrated a high prevalence of MINS (40.9%). Of concern, the majority (75%) were asymptomatic. Furthermore, we found a five-fold increase of 30-day adverse complications (primarily cardiac in nature) and increased length of stay in patients with MINS. However, overall mortality rates were low without a statistically significant difference compared to those without MINS. Our results far exceeded previous MINS estimates of 8% to 19% [1,2]. We believe this was due to the utilisation of high sensitivity troponin, with a high specificity compared to a standard cardiac troponin test used in other studies. In addition, the selected cohort of patients were frail; and were at high perioperative risk. This is supported by the fact that > 50% of patients had a CFS score ≥ 4 and more than 30% of the patients had a RCRI score ≥ 3 (high postoperative predicted cardiac risk). We also found a higher premorbid level of congestive heart failure, atrial fibrillation, coronary artery disease and diabetes comorbidities in those with MINS.
In our cohort, we found a higher proportion of patients with MINS had emergency or urgent surgery. These patients are likely to be unwell or septic. A systemic inflammatory response causes endotoxin release, which decreases cardiac ejection fraction and results in myocardial injury [3]. We also found carotid endarterectomy was associated with MINS. However, this was the largest operative subgroup and may suggest that other subgroups were underpowered. Although the exact mechanism of this relationship remains uncertain, one postulated theory is that high Tissue Factor (TF) activity in the atherosclerotic carotid plaque during surgery may lead to myocardial injury [15]. We demonstrated that MINS group had an increased length of stay (9 days vs 6 days, p=0.002). This could be due to a higher proportion of patients with MINS having cardiovascular complications (i.e., congestive heart failure and myocardial infarction), leading to prolonged hospitalization. Consequently, this would further impact on healthcare costs.
Adverse Outcomes in Patients with MINS
A higher proportion of patients with MINS had 30-day adverse outcomes (34.6% vs 6.7%). This was driven primarily by cardiac complications, in particular myocardial infarction, and post-operative congestive heart failure. This is confounded by the fact that myocardial infarction is a subgroup of MINS, such that separating the true effect difference would be difficult. In addition, myocardial infarction may also mediate the increased postoperative congestive heart failure. However, it is reasonable to assume that those with asymptomatic myocardial injury (making up 75% of MINS in this study) are more likely to progress to myocardial infarction and either trigger or worsen heart failure, such that patients with MINS still require close clinical monitoring. Further larger studies are needed to characterise this three-way relationship (i.e., exclude myocardial infarction in the subgroup of MINS and repeat the analysis in those patients with and without MINS). Also, patients with MINS who have a history of heart failure were more likely at risk of developing postoperative congestive heart failure complications. The proposed mechanisms were due to increased transmural pressure, endothelial dysfunction, circulating neurohormones, anaemia or hypotension [3]./
We found an overall mortality rate of 3.9% in our study, which is low in comparison to the VISION study [2]. There was a significant increase in mortality rate in VISION (9.8% (MINS) vs 1.1(no MINS), OR 10.07 [95% CI 7.84-12.94], p < 0.001) [2]. This may either reflect our small sample size or differences in standard of care. Patients in our institution are co-managed between geriatrician and vascular surgeons to optimize patients perioperatively, based on the well-established ortho-geriatric model of care which has been shown to improve mortality and clinical outcomes [16-20].
Frailty Scores and Cardiac Risk Stratification
We observed that patients in the MINS group were generally vulnerable or frail (CFS ≥4). This may imply that elderly patients, with co-existent multiple complex comorbidities and lower cardiac reserve, were more vulnerable to intraoperatively stressors. The increase in oxygen demand intraoperatively may cause troponin leak and myocardial injury [21]. This emphasizes the importance of close and early perioperative assessment and medical optimization in those deemed pre-morbidly vulnerable or frail, to improve outcomes. Our study showed an association between MINS and a high RCRI score of ≥ 3 (indicating high perioperative cardiac risk and complications). However, the RCRI tool demonstrates poor risk stratification in vascular surgery [22]. The majority of vascular patients have an underlying diffuse atherosclerotic disease which may not reflect on the scoring chart [22]. Consequently, high sensitivity troponin may be an alternative to the RCRI tool to predict perioperative cardiac risk and complications.
Considerations for Management
In current practice, there are no set universal guidelines for managing patients with MINS. The only large clinical trial in patients with MINS (Management of Myocardial Injury After Noncardiac Surgery [MANAGE] trial) studied administration of oral Dabigatran 110mg twice daily in a total of 1754 patients [23]. In this study, the Dabigatran arm showed a lower primary outcome of composite adverse events compared to placebo (11% vs 15%, hazard ratio 0.72 [95% CI 0.55-0.09], p=0.0115) [23]. However, at least 46% of participants discontinued the study drug in this trial and the drug has not yet been licenced for this indication [23]. Our study provides further practical considerations in the management of patients with MINS. Early review by a geriatrician would again be invaluable for such patients, especially in those deemed vulnerable or frail, to provide the need for medical optimisation with medical therapy and earlier referral to cardiology.
Strengths
A single investigator assessed all patient records ensuring consistency. This was verified by a senior clinician as required. This study utilised high sensitivity cardiac troponin, which has a high specificity compared to a standard cardiac troponin test. Additionally, we included the measurement of preoperative troponin levels to set as the baseline, which is important in patients with end-stage renal failure with chronically elevated troponin or patients with elevated troponin due to other reasons such as sepsis. We also included a few additional outcomes compared to the other studies (i.e., association between MINS with frailty scores and RCRI). Furthermore, all patients enrolled in this study completed the 30-day follow up.
Limitations
The study sample size was small. It was a single centre study compared to the VISION study, which involved eight countries in five continents [2]. In this study, troponin levels was added to a routine postoperative Day 1 until Day 3 blood tests, and additional MINS may have been missed beyond this period which could underestimate the prevalence of MINS. However, the current evidence suggests low specificity in detecting myocardial infarction beyond this time frame [24].
Conclusions
We demonstrated a high prevalence of MINS in vulnerable, frail, and older patients undergoing major vascular surgery, with the majority being asymptomatic. Patients with MINS had a significantly higher risk of adverse outcomes at 30 days, principally cardiac complications, as well as longer length of stay in hospital, although mortality was not significantly increased. We also found that frailty assessment and cardiac risk stratification tools predicted MINS. The study supports the recommendation that routine troponin monitoring should be performed post major vascular surgery and that geriatrician co-management of such patient’s peri-operatively. May play an important part in achieving optimal outcomes.
Appendix 1:
Baseline characteristics of vascular patients who underwent major vascular surgery.
1. Age- patient aged 50 years or older.
2. Sex - Female or male
3. Diabetes - documented history of diabetes or patient on diabetic medications on admission.
4. Cardiovascular disease - documented history of hypertension, coronary artery disease, cerebrovascular disease (include stroke / TIA), peripheral vascular disease or congestive heart failure.
5. Hypertension - documented history of hypertension or patient on antihypertensive treatment on admission 6. History of congestive heart failure - documented history of congestive heart failure or previous radiographic findings with congestive heart failure (such as alveolar oedema, Kerley B lines, cardiomegaly, dilated upper lobe vessels or pleural effusion)
7. History of coronary artery disease - history of angina, previous myocardial infarction or acute coronary syndrome; previous echocardiographic findings of abnormal segmental cardiac wall motion or evidence of segmental fixed defect on myocardial perfusion scan; positive stress echocardiographic or radionuclide exercise demonstrating cardiac ischemia; evidence of atherosclerotic stenosis ≥50% of coronary artery on coronary angiographic or CT coronary angiographic or evidence of pathological Q waves on two contiguous electrocardiogram leads.
8. History of coronary artery bypass graft (CABG) or percutaneous coronary intervention (PCI)- documented history of CABG or PCI on admission
9. Glycated haemoglobin > 7% - documented history of glycated haemoglobin of greater than 7% in the last 6 months on admission.
10. History of peripheral vascular disease -documented history of intermittent claudication, previous history of vascular surgery for atherosclerotic disease, ankle-brachial index of ≤0.90 (regardless at rest or exercise), doppler or angiographic study with ≥70% stenosis in a noncardiac artery.
11. History of stroke - documented history of previous stroke, or neuroimaging (such as CT head or MRI brain) evidence of stroke.
12. History of TIA - documented history of previous TIA on admission (transient neurological symptoms secondary to brain, spinal cord, or retinal ischemia without acute infarction)
13. Chronic obstructive pulmonary disease (COPD) - documented history of COPD, emphysema or bronchitis or patient reported history of daily production of sputum for at least 3 months in 2 consecutive years.
14. History of smoking - documented history of tobacco smoking
15. Current atrial fibrillation -documented history of atrial fibrillation on admission
16. Preoperative creatinine > 176mmol/L- According to the Revised Cardiac Risk Index (RCRI) criteria.
17. Active cancer - documented history of diagnosis of cancer, or previously had surgery for cancer; or previously had received treatment for cancer (such as chemotherapy, radiation, or surgery). This excludes patients who had non-melanoma skin cancers.
18. Urgent surgery- surgery that occurred between 24 to 72 hours after the diagnosis of an acute surgical condition.
19. Emergency surgery - surgery that occurred <24 hours after the diagnosis of an acute surgical condition.
Appendix 2:
Clinical Frailty Scale [12]
Appendix 3:
References
- Biccard BM, Scott DJA, Chan MTV, Archbold A, Wang CY, et al. (2018) Myocardial Injury After Noncardiac Surgery (MINS) in Vascular Surgical Patients: A Prospective Observational Cohort Study. Ann Surg 268(2): 357-363.
- Botto F, Alonso-Coello P, Chan MT, Villar JC, Xavier D, et al. (2014) Myocardial injury after noncardiac surgery: a large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30-day outcomes. Anesthesiology 120(3): 564-578.
- Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, et al. (2018) Fourth Universal Definition of Myocardial Infarction (2018). Circulation 138(20): e618-e651.
- Sousa J, Rocha-Neves J, Oliveira-Pinto J, Mansilha A (2021) Myocardial injury after non-cardiac surgery (MINS) in EVAR patients: a retrospective single-centered study. J Cardiovasc Surg (Torino) 62(2): 130-135.
- Duceppe E, Parlow J, MacDonald P, Lyons K, McMullen M, et al. (2017) Canadian Cardiovascular Society Guidelines on Perioperative Cardiac Risk Assessment and Management for Patients Who Undergo Noncardiac Surgery. Can J Cardiol 33(1): 17-32.
- Kristensen SD, Knuuti J, Saraste A, Anker S, Bøtker HE, et al. (2014) 2014 ESC/ESA Guidelines on non-cardiac surgery: cardiovascular assessment and management: The Joint Task Force on non-cardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). Eur Heart J 35(35): 2383-2431.
- Fleisher LA, Fleischmann KE, Auerbach AD, Barnason SA, Beckman JA, et al. (2014) 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol 64(22): e77-e137.
- Rocha V, Marmelo F, Leite-Moreira A, Moreira-Goncalves D (2017) Clinical Utility of Frailty Scales for the Prediction of Postoperative Complications: Systematic Review and Meta-Analysis. Rev Port Cir Cardiotorac Vasc 24(3-4): 132.
- Dhesi JK, Lees NP, Partridge JS (2019) Frailty in the perioperative setting. Clin Med (Lond) 19(6): 485-489.
- (2020) Troponin I (Abbott Architect).
- Giannitsis E, Kurz K, Hallermayer K, Jarausch J, Jaffe AS, et al. (2010) Analytical Validation of a High-Sensitivity Cardiac Troponin T Assay. Clinical Chemistry 56(2): 254-261.
- Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, et al. (2005) A global clinical measure of fitness and frailty in elderly people. Cmaj 173(5): 489-495.
- McIsaac DI, MacDonald DB, Aucoin SD (2020) Frailty for Perioperative Clinicians: A Narrative Review. Anesth Analg 130(6): 1450-1460.
- Lee TH, Marcantonio ER, Mangione CM, Thomas EJ, Polanczyk CA, et al. (1999) Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation 100(10): 1043-1049.
- Feng H, Wang TL, Cai B (2014) Ischemic stroke predicts myocardial injury after carotid endarterectomy for symptomatic severe carotid artery stenosis. Clin Appl Thromb Hemost 20(4): 422-426.
- Goldacre MJ, Roberts SE, Yeates D (2002) Mortality after admission to hospital with fractured neck of femur: database study. Bmj 325(7369): 868-869.
- Chong C, Christou J, Fitzpatrick K, Wee R, Lim WK (2008) Description of an orthopedic-geriatric model of care in Australia with 3 years data. Geriatr Gerontol Int 8(2): 86-92.
- Shaw M, Pelecanos AM, Mudge AM (2020) Evaluation of Internal Medicine Physician or Multidisciplinary Team Comanagement of Surgical Patients and Clinical Outcomes: A Systematic Review and Meta-analysis. JAMA Netw Open 3(5): e204088.
- Martinez-Reig M, Ahmad L, Duque G (2012) The orthogeriatrics model of care: systematic review of predictors of institutionalization and mortality in post-hip fracture patients and evidence for interventions. J Am Med Dir Assoc 13(9): 770-777.
- (2022) Department of Rehab and Aged Care.
- Finn M, Green P (2015) The Influence of Frailty on Outcomes in Cardiovascular Disease. Rev Esp Cardiol (Engl Ed) 68(8): 653-656.
- Ford MK, Beattie WS, Wijeysundera DN (2010) Systematic review: prediction of perioperative cardiac complications and mortality by the revised cardiac risk index. Ann Intern Med 152(1): 26-35.
- Devereaux PJ, Duceppe E, Guyatt G, Tandon V, Rodseth R, et al. (2018) Dabigatran in patients with myocardial injury after non-cardiac surgery (MANAGE): an international, randomised, placebo-controlled trial. Lancet 391(10137): 2325-2334.
- Zhelev Z, Ohtake H, Iwata M, Terasawa T, Rogers M, Peters JL, et al (2019) Diagnostic accuracy of contemporary and high-sensitivity cardiac troponin assays used in serial testing, versus single-sample testing as a comparator, to triage patients suspected of acute non-ST-segment elevation myocardial infarction: a systematic review protocol. BMJ Open 9(3): e026012.






























