Risk of Fall, Cognition and Static Posture in Aging
Fagundes C*, Renner JS, Lopes IO, Barbosa R, Kampff CA, Alcantara VR, Peixoto MCO, Kleemann KL, Cardoso EH, Souza DS and Santos GA
Postgraduate Program in Cultural Diversity and Social Inclusion, Feevale University, Brazil
Submission: August 16, 2022; Published: September 01, 2022
*Corresponding author: Caroline Fagundes, Postgraduate Program in Cultural Diversity and Social Inclusion, Feevale University, Brazil
How to cite this article: Fagundes C, Renner JS, Lopes IO, Barbosa R, Kampff CA, et al. Risk of Fall, Cognition and Static Posture in Aging. OAJ Gerontol & Geriatric Med. 2022; 7(1): 555703. DOI: 10.19080/OAJGGM.2022.07.555703
Abstract
Introduction: The elderly with impaired cognition may have mobility deficits, slowing of movements, behavioral changes and shorter reaction time in the face of imbalances, predisposing them to falls. In addition, with aging, joint flexibility is reduced, resulting in postural deviations and limitation of mobility in elderly, making it difficult to maintain static balance and safe gait.
Objective: To analyze the relationship between the risk of falls, cognitive performance and static posture in aging.
Method: 107 subjects participated in this research, aged between 60 and 89 years, divided into 2 groups: the first formed by 54 individuals who practice water aerobics and the second composed of 53 elderly people participating in a computer program. For data collection, the following instruments were used: Mini Mental State Examination, Fall Efficacy Scale, Berg Balance Scale and Postural Assessment Software (SAPO).
Results: The results showed satisfactory means for the scales used. Furthermore, it was observed that the risk of falls is directly related to the angle of thoracic kyphosis and ankle angle. An indirect relationship between the risk of falls and the self-efficacy of falls and vertical head alignment was also identified (R2: 0.367).
Conclusion: There was a significant relationship between the risk of falls, cognition and static posture in elderly people. Based on the findings of the present study, it is possible to develop measures to prevent falls in the elderly.
Keywords: Cognition; Elderly people; Posture; Falls; Aging; Frailty syndrome; Dementia; Joint flexibility; Fall Effectiveness Scale; Berg Balance Scale
Introduction
Aging is a worldwide phenomenon. According to the United Nations Organization, life expectancy for developed countries in 1950 was 60/70 years, and for developing countries it was 40/50 years. It is estimated that, in 2050, the average age for developed countries will be 70/80 years and 60/70 years for developing countries. These data show that, in 1950, the difference in life expectancy between developed and developing countries was 20 years. One hundred years later, this difference is estimated at 10 years. The increase in the elderly population in the world is associated with a decrease in births and fertility and an increase in life expectancy, due to investment in public policies related to the quality of life of the elderly [1]. Falls in elderly are common and can result in functional incapacity, directly affecting the quality of life of these individuals. One of the causes of decline in old age is cognitive deficit. Elderly people with impaired cognition may have mobility deficits, slow movement, behavioral changes and shorter reaction time to imbalances, predisposing them to falls. In addition, muscle strength, especially in the lower limbs, is also impaired with advancing age, with a decrease in recruitment and activation of motor units [2-3]. Furthermore, another factor of decline in the elderly population is the reduction in joint flexibility, resulting in postural deviations. Thus, the mobility of the elderly becomes limited, interfering with body sway and making it difficult to maintain static balance and safe gait [4-5]. Therefore, this study aimed to analyze the relationship between the risk of fall, cognitive performance and static posture in aging.
Method
This study was approved by the Feevale University Ethics And Research Committee, under the number 3.096.990. The present study was characterized as quantitative, descriptive and transversal. This research was carried out in the city of Dois Irmãos, Rio Grande do Sul, Brazil, in partnership with the Department of Health, Social Assistance and Environment and in the city of Novo Hamburgo, Rio Grande do Sul, Brazil, in partnership with the Directorate of Digital Inclusion of the Municipal Administration Secretariat of Municipality of Novo Hamburgo, Rio Grande do Sul, Brazil. The inclusion criteria were 60 years or older, groups attending hydrogymnastics, in the city of Dois Irmãos, Rio Grande do Sul, Brazil, and informatic program groups for the elderly, in the city of Novo Hamburgo, Rio Grande do Sul, Brazil. The elderly could not being institutionalized or hospitalized. In addition, the subject must have the mental and health conditions to have independence and autonomy to participate in the study, and thus, sign the Consent Form Free and Informed. Exclusion criteria were to present dementia, frailty syndrome, being hospitalized or institutionalized.
To analyze the variables of static posture, balance and cognitive performance, the following instruments were used:
Mini Mental State Examination: This is a cognitive screening test widely used in the evaluation of the elderly and was developed by Folstein, Folstein and McHugh and translated by Bertolucci et al. [7] [6,7]. It consists of several questions typically grouped into seven categories, each one designed to evaluate specific cognitive functions: orientation to time (5 points), orientation to place (5 points), recording of three words (3 points), attention and calculation (5 points), recall of three words (3 points), language (8 points) and visual constructive capacity (1 point). The application is fast, ranging from 5 to 10 minutes. The items are evaluated by a score ranging from 1 to 5 points, reaching a maximum of 30 points. Schooling was pointed out by Bertolucci et al. [7] Juva et al. [8] Almeida and Almeida [9] as a determinant factor for the evaluation presenting differentiated cut-off points according to the number of years of study [7-9]. The cut-off points were based on the Brucki et al. criteria [10]. In clinical practice, the cut-off point 23 or 24 is the most commonly used, presenting high sensitivity and specificity for the detection of cognitive damage and dementia. It also identifies the influence of the social and economic environment in the studies of [7-11]. According to Almeida and Almeida the Mini Mental State Examination scores have significant influence of age [9].
Fall Effectiveness Scale- International: This scale assesses the fear of falling. The original scale was developed by Tinetti, Richman and Powell in 1990 and was called Fall Efficacy Scale. In 2005, Yardley et al. developed the Fall Efficacy Scale - International version, which had 6 more items. In Brazil, the scale was adapted for use in elderly by Camargos et al. [12]. The instrument assesses the concern of elderly regarding the possibility of falling when performing 16 activities, with scores ranging from one (“not worried at all”), to four, (“extremely concerned”), points per action. The total of points is obtained by the sum of these values and varies between 16 and 64 points. The higher score indicates lower self-efficacy index. For the evaluation of the scale, a sum ≥ 23 is associated with sporadic fall and higher than 31 points with a recurrent fall [13-14].
Berg Balance Scale: The Berg Balance Scale is a validated instrument for the functional evaluation of the balance, with 14 tasks with five items each and scores to 0-4 for each task: 0 - is unable to perform the task and 4 - performs the independent task. The total score ranges from 0 - 56 points. The lower score means higher the risk for falls. Score lower than 45 points indicates risk of falling. The Berg Balance Scale, was created in 1992 by Katherine Berg, and has been widely used to assess balance in individuals aged 60 years or over. This scale was translated and adapted to the Portuguese language by Miyamoto et al. [15] in his dissertation of master [15]. The test is simple, easy to apply, and safe for the evaluation of elderly. It only requires a timer and a ruler as equipment and the test execution takes about 15 minutes [16-19].
Postural Assessment Software: Postural Assessment Software is a software that allows the import and calibration of images, the marking of points on the photograph according to the protocol, and the free marking of points to determine linear measurements, angular values, distance measurements and body angles. Postural Assessment Software is a free program that was developed by the University of São Paulo, and its reliability is well documented. To carry out the postural assessment in this software, the following materials and procedures were used: black TNT fabric (2.0 m high by 1.40 m wide) at the bottom of the photograph site in order to facilitate the subsequent analysis in Postural Assessment Software; plumb line fixed to the TNT fabric (two 15mm styrofoam balls) at a distance of 1 meter between them, with the aim of later calibrating the image in the software; black cardboard mat for positioning the individual at the time of photography; digital still camera (Sony Cyber-shot DSC-W690 16.1mp Digital Camera) with tripod; anatomical markers (8 15mm styrofoam balls applied to the subject with double-sided tape); white chalk to outline the subject’s right and left foot on black cardstock.
To ensure the same support base in the photographs in the different views (anterior view, right side view and left side view) a black cardboard mat was used, on which the individual is positioned freely for the first photograph. The verbal command was: “you will stand on this black cardboard in a position that is familiar and comfortable for you, position your feet in the way that is most comfortable for you”. The camera was positioned 3 meters away from the individual and at a height of about half of their height [20-22].
The anatomical markers were located through the palpatory surface anatomy, in the subject’s orthostatic position. The points selected follow the Postural Assessment Software protocol. This protocol was suggested by the initial program development project team and their choice was based on clinical relevance, scientific basis, methodological feasibility and applicability. This protocol is used as a standard for postural assessment that generates values for the posture database. To assess thoracic kyphosis, an anatomical marker was added to the protocol, applied under the spinous process of the twelfth thoracic vertebra (T12) [20].
At the time of the photography, the subject’s image was framed together with the plumb line. Then, with a white chalk, the outline of the individual’s right and left foot was drawn on black cardboard. After taking the photo in a particular view, the cardboard was rotated through 90 degrees and the subject was instructed to position himself on top of the cardboard with his feet on the drawing made with chalk. With the photographs ready, it was already possible to transfer them to the computer and start the evaluation at Postural Assessment Software. After installing the program, the images were imported and calibrated in the software. This procedure adjusted the vertical direction of the image and the transformation of distances in the image in pixels to real object distances (measured in meters), as shown in the postural assessment report issued by Postural Assessment Software [20].
Results
Participated in this research 107 elderly people between 60 and 89 years old, divided into 2 groups: hydrogymnastics and informatics.
The (Table 1) shows the mean age, sex and education of the groups surveyed. Individuals who practiced hydrogymnastics showed the highest mean age, 72.96 years. It is observed that the majority of the sample was composed of women, corresponding to 78.5% of the total participants in this study. Regarding education, most had incomplete primary education, equivalent to 58.9% of the total, followed by complete secondary education (13%).

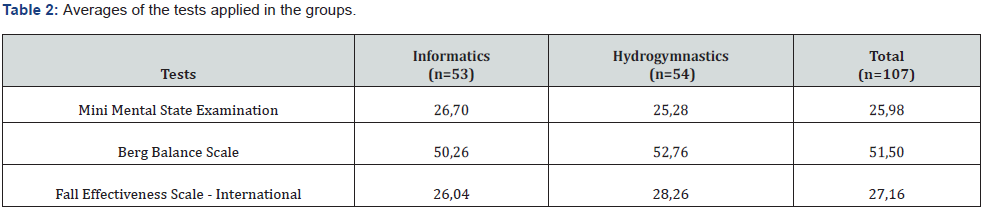
The (Table 2) reveals that the elderly of this study had preserved cognition and, according to the Berg Balance Scale, a low risk of falling. However, data obtained from the Fall Effectiveness Scale - International indicated a risk of sporadic falls.
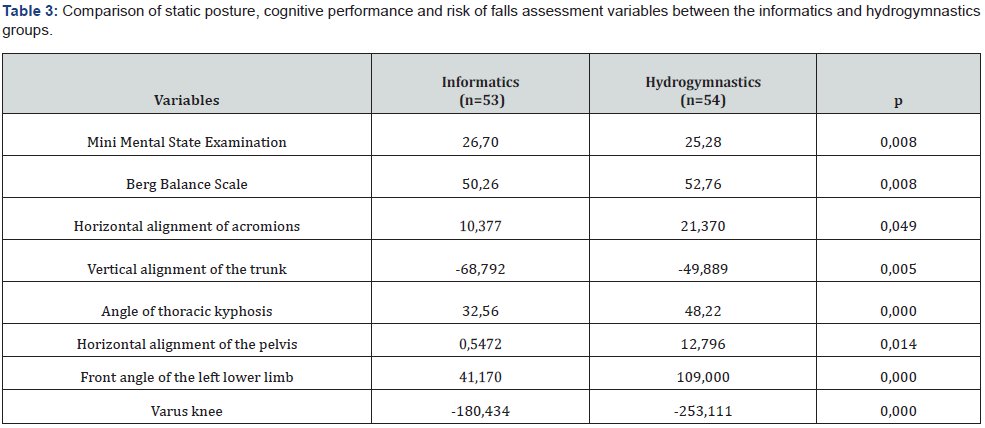
The (Table 3) shows the variables that had a significant relationship between the groups. Thus, it can be observed that the elderly in this study had good cognitive performance, low risk of falling and static postural changes within normal limits, suggesting that there is a relationship between risk of falling with cognitive performance and static posture in aging.
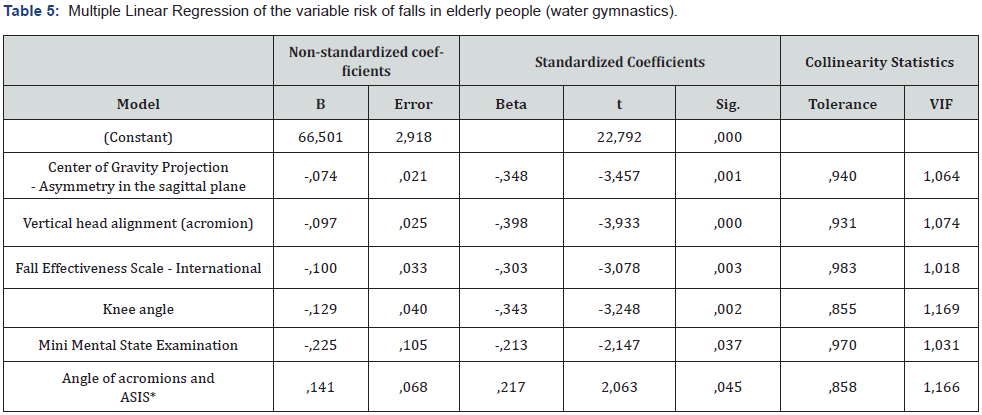
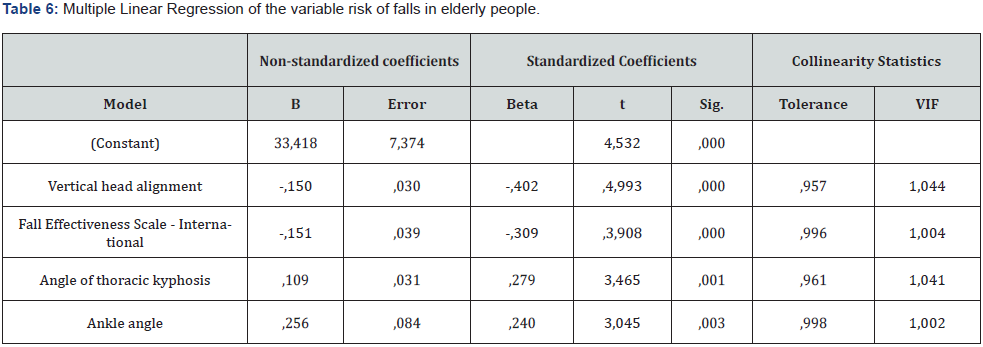
Linear regression analysis was performed using the stepwise method, with a significant level ≥ 0.05 using the Berg Balance Scale instrument as the dependent variable, which assesses the risk of falls. It is present below three tables with the analysis models. The (Table 4) shows the analysis with the group of elderly from Novo Hamburgo who regularly participate in a informatic program for elderly. In (Table 5) it is possible to see the same analysis carried out with the Dois Irmãos group that regularly performs water aerobics activities and finally in (Table 6) it is showed the same analysis carried out with the two groups together.
In the analysis presented in (Table 4), the relationship (sign and intensity) between the variable risk of falls assessed by the Berg Balance Scale instrument (dependent, explained) was verified, directly related to the variable cognitive performance assessed by the Mini Mental State Examination and the horizontal line between the acromions (independent, explanatory). An indirect relationship of the risk of falls with the self-efficacy of falls was also identified, as assessed by the Fall Effectiveness Scale - International instrument, vertical line of the head (lateral view, distance between the ear lobe and the acromion) and hip angle (lateral view, angle between the acromion, trochanter of the femur and lateral malleolus). In this model, an R square (R2) of 0.575 was obtained. This coefficient of determination is a measure of the efficiency of the regression equation. It indicates that 57.5% of fall risk variations can be explained by variations in fall risk selfefficacy, cognitive performance and postural assessment results. In this group, it is clear that preventing the risk of falls is associated with better cognitive performance and a better perception of selfefficacy in falls, as well as better vertical alignment of the head and horizontal alignment of the acromion and a smaller hip angle.

*ASIS: Anterior Superior Iliac Spine
In the (Table 5) also verified the relationship between the variable risk of falls, but now with the group of elderly in the municipality of Dois Irmãos, Rio Grande do Sul, Brazil, who regularly perform hydrogymnastic activities. It was identified in the model that the risk of falls is directly related to the variable angle between the two acromions and the two anterior-superior iliac spines. An indirect relationship of the risk of falls with selfefficacy of falls, cognitive performance, vertical head alignment (lateral view, distance between ear lobe and acromion) and knee angle (lateral view, angle between the femoral trochanter, knee joint line and lateral malleolus).
In this model, an R square (R2) of 0.553 was obtained. This coefficient of determination is a measure of the efficiency of the regression equation. It indicates that 55.3% of the variations in the risk of falls can be explained by variations in the self-efficacy of risk of falls, by cognitive performance and by the results of the postural assessment. In this group, it is clear that preventing the risk of falls is associated with a decrease in cognitive performance and an increase in the perception of self-efficacy, as well as a better vertical alignment of the head and an increase in the angle between the two acromions and the two anterior superior iliac spines and a lower knee angle.
In the (Table 6) also verified the relationship between the variable risk of falls, but now with the two groups, hydrogymnastics and informatic. It was identified in the model that the risk of falls is directly related to the variable thoracic kyphosis angle and ankle angle (lateral view, angle formed between the knee joint line and the ankle with the horizontal line). An indirect relationship of the risk of falls with the self-efficacy of falls and vertical head alignment (side view, distance between the ear lobe and the acromion) was also identified. In this model, an R square (R2) of 0.367 was obtained. This coefficient of determination is a measure of the efficiency of the regression equation. It indicates that 36.7% of the variations in the risk of falls can be explained by variations in the self-efficacy of fall risk and by the results of the postural assessment. In this evaluation, observed that the elderly maintain a successful aging profile due to both physical and cognitive activities and social involvement and it is clear that preventing the risk of falls is associated with an increase in the perception of selfefficacy of falls, as well as a better vertical alignment of the head and increased angle of thoracic kyphosis and ankle angle.
Discussion
Cognitive deficit increases the risk of falls in the elderly. Studies show that 65.5% of falls in individuals aged 60 years and over are associated with a decline in cognition. In a research conducted with non-institutionalized elderly people with Alzheimer’s disease and cognitively preserved elderly, it was observed that those with Alzheimer’s disease had 36% probability of falling, while for the other subjects, the chance of falling was 11%. Similar results were found by Cruz et al. [3], in which of the 412 elderly non-institutionalized, 42% of them had impaired cognition and a history of falls. Similar findings were found by Valcarenghi et al. [23] in their study carried out with 25 institutionalized elderly. Of these, 20 showed cognitive impairment and only 10 elderly people reported a history of falls. The results found in the study by Ferraresi et al. [24] corroborate with the anterior studies. In this research made with 172 non-institutionalized elderly, which 117 were women and 55 were men, the average of the Mini Mental State Examination was 26.4 for women and 27 for men. These data show that there is no decline in cognition in this sample. In that same study, the Berg Balance Scale was also applied, with an average of 51.5 for both sexes, suggesting that there is no risk of falls in this population. These findings suggest that there is a relationship between cognition and falls, that is, the lower the cognitive impairment, the lower the risk of falls [3-4, 23].
Falls in elderly with cognitive impairment can be explained by declines in specific cognitive domains, such as executive function, attention and memory. Motor and sensory systems are linked by higher-order neurological processes related to cognition, which are called for motor planning, dual-task attention, and responses to environmental circumstances [3]. Furthermore, according to Borges et al. [13], 51.9% of the elderly report fear of falling, reducing the self-efficacy in relation to falls. Low selfefficacy makes the individual focus on the goals that the person assign, making the person to avoid situations that they consider threatening. Thus, the elderly person limits the development of skills, resulting in a basis for building fear, in addition to being more susceptible to sedentary lifestyles and social isolation.
There is no consensus on the etiology of fear of falling in the elderly, however, it is known that physical, behavioral, environmental and functional factors are involved. Previously, it was claimed that the fear of falling was related to the history of falls, however, studies show that the fear of falling is present even in individuals who have never fallen, as shown in the study by Cruz, Duque et al. [14], in which, of the 314 elderly participants in the study, 207 (65.9%) did not report falls and of these, 196 (94.7%) were afraid of falling.
In a research carried out with 49 elderly women, the mean of the Fall Effectiveness Scale - International was 33.51, indicating a recurrent fall. Contrary results were found by Silva et al. [25], in which the mean Fall Effectiveness Scale - International was 25.9, indicating a sporadic fall. Other interesting data from this research is that individuals aged 60 years or more had an average of 27.1 on the Mini Mental State Examination and 53.7 on Berg Balance Scale. These findings indicate that these elderly people showed good cognitive performance and low risk of falls, however, these individuals did not present satisfactory self-efficacy for falls, which is in agreement with the results found in this study [13].
Over the years, there is a reduction in the elasticity of the tissues that cover the joints, resulting in limited movement and postural deviations. The most commonly affected joints are the spine, hips and knees, and it can be the main cause of discomfort, pain and functional disability in the elderly population [5, 26]. Among the most common postural changes there is a hyperkyphosis toracic. The angle of thoracic kyphosis can vary between 20° and 40° in the general population, however, in the elderly, angles of up to 56° are considered normal. Increased thoracic curvature in individuals aged 60 years or more is also associated with osteoporosis, since this pathology modifies the shape and composition of bones, especially the vertebrae. The muscles, on the other hand, are affected by sarcopenia, resulting in a decrease in the capacity to generate strength and flexibility.
In addition, the elderly may present increased body fat and abdominal and waist circumferences, causing the body to reorganize to ensure orthostatic balance. In fact, thoracic hyperkyphosis can also reduce chest expansion, resulting in respiratory deficit. In the study by Tavares et al. [27], 82.5% of the elderly had shoulder protrusion. This fact may result from the increased thoracic kyphosis resulting in the retraction of the pectoralis major and minor, serratus anterior and intercostal muscles. The increase in thoracic curvature, as well as the cervical anteriorization, point to weakness of the spinal extensor muscles and shortening of the anterior musculature in this region, causing the center of gravity to move forward, thus modifying the imposed direction of body weight on the vertebrae and intervertebral discs, facilitating loss of balance and favoring the elderly to fall [4-5, 26, 28].
Conclusion
At the end of this study, it was concluded that the evaluated subjects have a low risk of falling, satisfactory cognitive performance and postural changes within normal limits. However, the elderly interviewed showed reduced self-efficacy for falls. Among the variables studied, a significant relationship was observed between cognition, risk of falling and static posture. Thus, the angle of thoracic kyphosis, frontal angle of the left lower limb and knee varus stood out, with the highest level of significance (P=0.000). In the linear regression of the two groups, a significant relationship was observed between the risk of falls variables with the self-efficacy of falls, the vertical head alignment, the thoracic kyphosis angle and the ankle angle. That is, a better perception of self-efficacy and vertical head alignment indicates lower the risk of falls. The higher angle of the thoracic kyphosis and the angle of the ankle, the higher is the risk of falls. Stands out that cognition is present in the groups, when studied separately, but when analyzed together this variable does not appear. Different from the self-efficacy that is present in all analyses. Therefore, it is suggested that cognition is not as relevant as self-efficacy for the risk of falls in the evaluated groups. Therefore, based on the findings of the present study, it is possible to develop prevention of falls in the elderly.
References
- United Nations Organization (2013) World Population Ageing. New York, USA
- Hernandez SSS, Coelho FGM, Gobbi S, Stella F (2010) Efeitos de um programa de atividade física nas funções cognitivas equilíbrio e risco de quedas em idosos com demência de Alzheimer. Braz J Phys Ther 14(1): 68-74.
- Cruz DT, Cruz FM, Ribeiro AL, Veiga CL, Leite ICG (2015) Associação entre capacidade cognitiva e ocorrência de quedas em idosos. Cad saúde colet 23(4): 286-393.
- Burke TN, França FJR, Meneses SRFDE, Cardoso VI, Pereira RMR, et al. (2010) Postural control among elderly women with and without osteoporosis: is there a difference? Sao Paulo Med J 128(4): 219-224.
- Gasparotto LPR, Reis CCI, Ramos LR, Santos JFQ (2012) Autoavaliação da postura por idosos com e sem hipercifose torácica. Ciência & Saúde Coletiva 17(3): 717-722.
- Folstein MF, Folstein SE, Mchugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3): 189-198.
- Bertolucci PH, Brucki SM, Camppacci SR, Juliano Y (1994) The mini-mental state examination in a general population: impact of educational status. Arq Neuropsiquiatr. 52(1): 1-7.
- Juva K, Mäkelä M, Erkinjuntii T, Sulkaya R, Ylikoski R, et al. (1997) Functional assessment scales in detecting dementia. Age Ageing 26(5): 393-400.
- Almeida OP, Almeida SA (1999) Short versions of the geriatric depression scale: a study of their validity for the diagnosis of major depressive episode according to ICD-10 and DSM-IV. Int J Geriatr Psychiatry 14(10): 858-865.
- Brucki SMD, Nitrini R, Caramelli P, Bertolucci PHF, Okamoto IH (2003) Sugestões para o uso do mini exame do estado mental no Brasil. Arq Neuropsiquiatr 61(3B): 777-781.
- Kukull WA (1998) Problems in measuring and interpreting cognitive decline. J Am Geriatr Soc. 46(12): 1578-1579.
- Camargos FFO, Dias RC, Dias JMD, Freire MTF (2010) Adaptação transcultural e avaliação das propriedades psicométricas da Falls Efficacy Scale - International em idosos brasileiros (FES-I- BRASIL). Rev Bras Fisioter, São Carlos 14(3): 237-243.
- Borges VS, Silva NS, Malta AC, Xavier NC, Bernardes LES (2017) Quedas força muscular e habilidades funcionais em idosas na comunidade. Fisioter mov 30(2): 357-366.
- Cruz DT, Duque RO, Leite ICG (2017) Prevalência do medo de cair em uma população de idosos da comunidade. Rev Bras Geriatr Gerontol 20(3): 309-318.
- Miyamoto ST, Lombardi J, Berg KO, Ramos LR, Natour J (2004) Brazilian version of the Berg balance scale. Braz J Med Biol Res 37(9): 1411-1421.
- Berg K, Maki B, Williams J, PJ Holliday, SL Wood-Dauphinee (1992) Clinical and laboratory measures of postural balance in an elderly population. Arch Phys Med Rehabil 73(11): 1073-1080.
- Hayes KW, Johnson ME (2003) Berg balance scale American Rheumatology (Oxford). 4: 28-30.
- Christofolett G, Oliani MM, Gobbi LTB, Gobbi S, Stella F (2006) Risco de quedas em idosos com doença de Parkinson e demência de Alzheimer: um estudo transversal. Rev Bras Fisioter 10(4): 429-433.
- Gazzola JM, Perracini MR, Ganança MM, Ganança FF (2006) Fatores associados ao equilíbrio funcional em idosos com disfunção vestibular crô Rev Bras Otorrinolaringol 72(5): 683-690.
- Duarte M, Ferreira EA, Maldonado EP, Freitas AZ (2005) Documentação sobre o POSTURAL ASSESSMENT SOFTWARE - Software para avaliação postural.
- Naves JM, Soares C, Svezzia VDEA, Cussolim FD, Mendonça AC (2017) Correlação entre alinhamento pélvico e fibroedema geloide. Fisioter Pesqui 24(1): 40-45.
- Preto LSR, Santos ARR, Rodrigues VMCP, Quitério NFDON, Pimentel MH, et al. (2015) Análise por Fotogrametria da Postura e Fatores de Risco Associados em Crianças e Adolescentes Escolarizados Referência 4(7): 31-40.
- Valcarenghi RV, Santos, SSC, Barlem ELD, Pelzer MT, Gomes GC, Lange C (2011) Alterações na funcionalidade/cognição e depressão em idosos institucionalizados que sofreram quedas. Acta Paul Enferm 24(6): 828-833.
- Ferraresi JR, Prata MG, Scheicher ME (2015) Avaliação do equilíbrio e do nível de independência funcional de idosos da comunidade Rev Bras geriatr gerontol 18(3): 499-506.
- Silva CRBP, Guerra RO, Fonsêca AMSDA, Gomes AC, Maciel ACC (2015) Mobilidade equilíbrio e desempenho muscular segundo a autoeficácia para quedas em idosas. Fisioter mov 28 (2): 231-240.
- Bandeira FM, Delfino FC, Carvalho GA, Valduga R (2010) Comparação entre a cifose torácica de idosos sedentários e praticantes de atividade física pelo método flexicurva. Rev Bras Cineantropom Desempenho Hum 12(5): 381-386.
- Tavares GMS, Rocha TR, Santo CCE, Piazza L, Sperandio FF, et al. (2013) Características posturais de idosos praticantes de atividade fí Fisioter Pesqui 18(4): 341-345.
- Porto F, Espinosa G, Vivian RC, Itaborahy AS, Montenegro RA, et al. (2012) O exercício físico influencia a postura corporal de idosas? Motriz: rev educ fis 18(3): 487-494.






























