Nocturnal Bladder Dysfunction: A Conceptual Framework Underlying Estimate of Cost
Bower WF*1,2,3,4, King S1,2, Holm-Larsen T and Whishaw1,2
1Department of Medicine & Aged Care, The Royal Melbourne Hospital, Australia
2Department of Sub-Acute Care Services, The Royal Melbourne Hospital, Australia
3Faculty of Medicine, Dentistry & Health Sciences, The University of Melbourne, Australia
4Physiotherapy, Department of Allied Health, The Royal Melbourne Hospital, Australia
Submission: March 31, 2022; Published: April 12, 2022
*Corresponding author: Wendy F Bower, The Royal Melbourne Hospital Royal Park Campus, Parkville, Australia
How to cite this article: Bower W, King S, Holm-Larsen T, Whishaw. Nocturnal Bladder Dysfunction: A Conceptual Framework Underlying Estimate of Cost. OAJ Gerontol & Geriatric Med. 2022; 6(4): 555693. DOI: 10.19080/OAJGGM.2022.06.555693
Abstract
Aim: Holistic care of geriatric inpatients involves bladder management at night. The aim of this study was to identify variables that should be included in a concept pool describing the attributable costs of nocturnal bladder dysfunction in the geriatric rehabilitation setting.
Design: A scoping review to map the key contributors to cost of care in older people with nocturnal bladder symptoms during hospitalization was conducted using machine learning.
Method: Individual and institution attributable cost factors implicated in the care for urinary tract symptoms at night during hospitalization, were identified and charted. A concept pool was developed and inter-relationships explored.
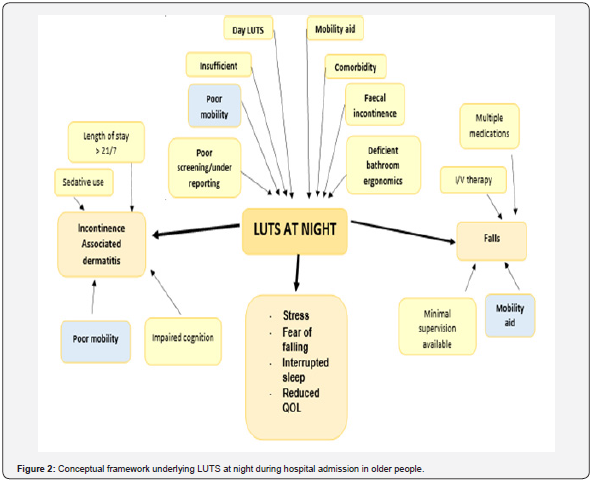
Results: The two major health service consequences observed were incontinence-associated dermatitis and falls incidents. From an individual perspective, four health consequences emerged: stress, a fear of falling during the night, interrupted sleep and reduced quality of life. Limited mobility appeared as a contributor to nocturnal Lower Urinary Tract Symptoms (LUTSn), incontinence-associated dermatitis and falls.
Conclusion: A conceptual framework of characteristics of affected individuals, alongside resource use and healthcare costs associated with bladder dysfunction at night, has been developed. This will provide a structure to evaluate the cost benefit of implementing improved care for older in-patients with LUTSn.
Keywords: Nocturia; Bladder symptoms; Lower Urinary Tract Symptoms; Older people; Fatigue; Hypnotic drugs; Hospitalization; Incontinence-Associated Dermatitis; Urinary incontinence; Sleep disturbance
Introduction
A large proportion of nursing care of older people, particularly at night, involves management of bladder dysfunction. There is a wide variation in care of elder patients with bladder dysfunction, from containment of urine to treatment of causal factors. Despite considerable healthcare resource allocation, the breadth of Lower Urinary Tract Symptoms (LUTS) at night has been poorly described. Bladder function at night is associated with poor quality sleep; more frequent episodes of toileting correlate with greater sleep disturbance, less time in deep sleep and more fatigue during the day [1]. Daytime function is diminished by sleep deprivation. Even in healthy adults daytime somnolence and fatigue are evident after disrupted sleep [2]. Sleepiness during the day compromises recovery from illness, successful rehabilitation, return to function and possible independence.
Bladder symptoms at night (LUTSn) are linked to adverse effects on health, safety and wellbeing and will therefore generate costs to both individuals and health services. An estimate of the direct and indirect costs of waking to void at night in three European countries revealed thousands of hospital admissions annually were attributable to nocturia or to fractures sustained because of night toileting [3]. Nocturia, waking to void during the sleep period, generates a substantial socioeconomic burden; potentially a threefold increase in medical costs and hospitalization days compared to individuals who sleep through the night [4]. The risk remains even after adjustment for age, sex and known diseases or risk factors [4].
The aim of this study was to identify variables that should be included in a concept pool describing the attributable costs of bladder dysfunction at night in the aged care hospital setting. A conceptual framework of characteristics of affected individuals, alongside resource use and healthcare costs associated with bladder dysfunction at night, will provide an overview of the cost benefit of implementing improved care for older in-patients with LUTSn. The specific objective was to identify variables common in hospitalized individuals with nocturnal bladder symptoms and elements of care that contribute to the cost of managing LUTS at night.
Methods
In order to map the key practices and potential contributors to cost of care in older people with nocturnal bladder symptoms during hospitalization the six-stage framework described by Arksey and O’Malley was utilized.
Stage 1: Research question
The research question asked what is known about the care and cost of managing bladder symptoms during the night in hospitalized geriatric patients. A scoping review was conducted to map the underlying key concepts and synthesize evidence related to managing bladder dysfunction at night during a hospital stay [Colquhoun 2014]. The review aimed to identify factors from both an individual and institution perspective implicated in the attributable cost of care for urinary tract symptoms at night during hospitalization.
Domains and variables of interest identified a priori as likely to influence care needs included comorbidities, mobility, continence status and management, general and disease-specific quality of life, patient beliefs about bladder dysfunction at night and healthcare cost parameters. Specific symptoms of interest included nocturia (passing urine more than once per night), urinary urgency at night, urinary incontinence either during or after waking from sleep and voiding dysfunction while passing urine. Factors considered to be on the causal pathway of bladder symptoms at night included difficulties with independent toileting, mobility limitations, fear of falling and self-management of bladder dysfunction. Healthcare parameters related to management of bladder symptoms at night comprised nursing tasks and care burden.
Stage 2: Identifying relevant studies
The literature review software ‘Silvi’ was used to identify studies from multiple databases that described bladder symptoms at night in older people admitted to hospital. The following search strategy was used: (“urinary incontinence/etiology”[MeSH Major Topic] OR “urinary bladder”[All Fields] OR “lower urinary tract symptoms /diagnosis”[MeSH Terms]) AND ((“hospital*”[MeSH Terms] OR “Hospitals”[MeSH Terms]) AND (“Aged”[MeSH Terms] OR “geriatric*”[MeSH Terms]) NOT (“cyst*”[MeSH Terms] NOT “malignan*”[All Fields]) NOT (“radical*”[All Fields] NOT (“cancer*”[All Fields] OR “neoplasms”[MeSH Terms] NOT (“prolapse*”[MeSH Terms] NOT “laparoscop*”[All Fields]) NOT “neurofibrom*”[MeSH Terms] OR “tumor*”[All Fields] OR “tumour”[All Fields] NOT (“prostat*”[All Fields] NOT (“ulcer*”[MeSH Terms] NOT “fistul*”[All Fields]) NOT “fungu*”[All Fields]) NOT (“biops*”[All Fields] OR “pathol*”[MeSH Subheading] NOT (“outpatient*”[All Fields].
The search was restricted to publications over the preceding six years, regardless of study design. This period included the time span of emerging interest in nocturia, the most common bladder symptom at night. At least the abstract was required to be in English. Reference lists from identified publications, along with abstracts from relevant scientific societies, were searched for studies describing older people during hospitalization. Existing knowledge networks in the area of bladder dysfunction at night were utilized.
Stage 3: Study Selection
Studies were initially rejected if they described the wrong cohort, were not related to bladder dysfunction or were duplicates. Studies where participants were palliative, had an indwelling urinary catheter in situ or were receiving dialysis were excluded. Studies describing events that occurred before admission or after hospital discharge were ineligible.
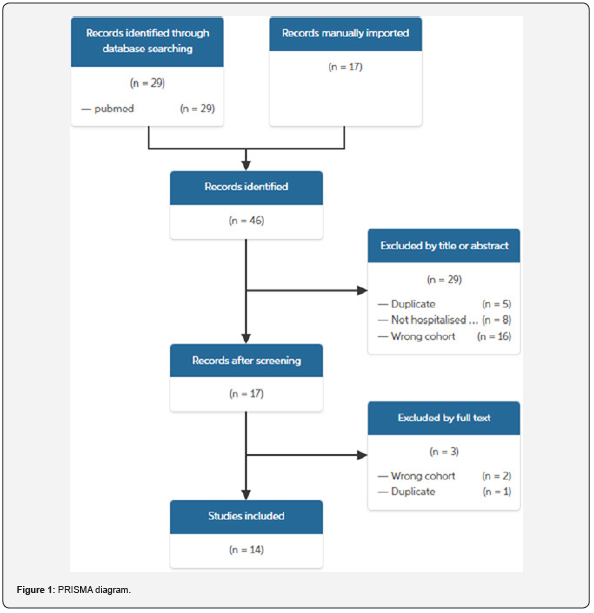
A single reviewer applied the inclusion and exclusion criteria to all the citations identified. An automated PRISMA table of the studies included and the reasons for rejection was generated. The program (Silvi) imported full papers into the selection component of the review process, extending review of abstract for relevance to include an overview of the full paper. Where the relevance was unclear the full paper was obtained.
Stage 4: Charting the data
To support synthesizing and interpreting of findings, key items of information were charted, for example, variables reported as having a significant association with bladder symptoms at night and economic factors. During the study selection process topics of interest were tagged within Slivi. Machine learning then extracted the charted data from the portable document format of the full papers.
Stage 5: Collating, summarizing and reporting
Demographic information from studies included was tabulated. The program (Silvi) then automated a summary table of findings with headings as per the topics tagged during charting. This overview provided the basis for identifying relevant contributors to care of bladder symptoms during the night. Commentary about factors identified in included studies as being associated with night care of bladder dysfunction was prepared. Formal quality assessment of studies was not made nor evidence was not weighted against other studies.
Charted findings were added to a concept pool to inform a theoretical framework about the care and cost of managing bladder symptoms at night in elderly individuals during hospitalization. A societal perspective was used to describe and depict the relationship between relevant factors.
Results
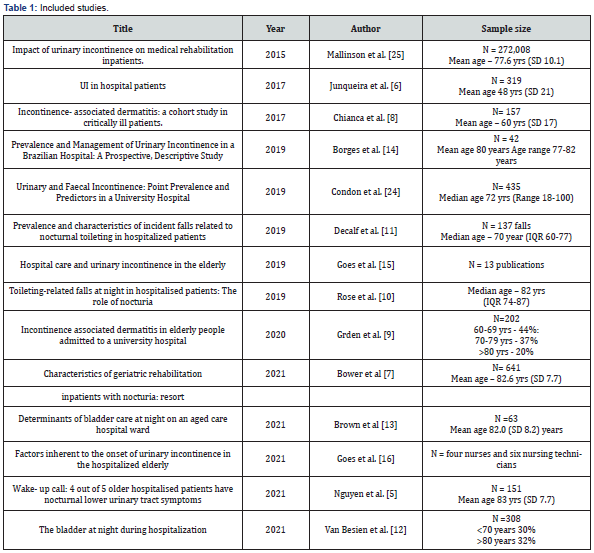
Study selection: As per the PRISMA diagram (Figure 1) 46 hits were found and 14 eligible studies dating from 2015 to 2021 were selected for full text review. (Table 1) shows that eight studies described any urinary incontinence whilst six limited the report to nocturnal bladder symptoms. Twelve of the studies included reported primary data from participants, while one study was a review and another described qualitative data from care staff. In all but one study participants had a mean age over 60 years.
Charting and summary of data: Any bladder symptom at night was reported in 80% of older people during hospitalization [5]. UI while asleep was described in 32-37% [6,5], nocturia more than once per night in 57.4% - 76% [7,5], nocturnal urinary urgency and nocturnal incontinence were recorded in 54% and 51% of an older hospitalized patient cohort. Patients with UI during the day had a mean of 2.86 LUTSn [5].
Multiple variables associated with LUTSn in older people during hospitalization were identified. Incontinence-Associated Dermatitis (IAD) occurred in 23.5% of patients over 70 years, rising to 44% of patients who stayed in hospital beyond three weeks [8,9]. Predictors of IAD included restricted mobility, impaired cognition, use of sedatives / hypnotic drugs and length of hospital stay. Two authors reported that between 15-28% of all falls incidents on the ward were related to toileting at night, half of these occurring at the bedside and most related to the early stage of mobilizing [10,11]. Although up to 50% of older low functioning patients admitted a fear of falling at night, less than one third called the night nurse for assistance to void [12]. Nocturnal falls were associated with use of multiple prescription medication (median of 9), intravenous therapy and dependence for mobility or use of a mobility aid [11].
Nocturia during hospitalization was predicted by daytime urinary frequency ± UI, nocturnal urinary urgency, faecal incontinence, comorbidity, health status and all sub-domains on the EQ-5D bar pain i.e. includes mobility limitations [7,12]. Postvoid UI was more common in men reporting multiple nocturia episodes per night as compared to men who slept all night [13].
Women required more bladder care during the night than men. In one study up to nine nursing care units per night were attributable to LUTSn with a mean of 2.33 bladder care moments [13]. Overall, 36% of care occasions related to providing assistance to reach the toilet, while 20% of night visits related to UI management [7]. Care provided for individuals with LUTSn was significantly associated with UI, limited mobility in the bed and requirement for assistance to ambulate but not with patient age [13]. Containment product use at night was common, with one study reporting a 6.7 times risk of UI when wearing such garments [6,14]. Care at night was noted to be affected by both quantity and quality of human resources, deficient bathroom ergonomics and indiscriminate use of geriatric diapers [15-16].
Personal cost variables identified included interrupted sleep, stress related to slowness of staff to respond to all buzzers and fear of falling [15]. One study considered that the needs of elderly patients with bladder dysfunction were not recognized due to a deficit in screening, risk identification and under reporting by ward staff [15]. The invisibility of UI by ward staff when planning care action, was noted as a common roadblock and attributed to education provided external to the hospital [16].
Generation of the concept pool: The two major health service consequences observed were incontinence-associated dermatitis and falls incidents. From an individual perspective four health consequences were identified: stress, a fear of falling during the night, interrupted sleep and reduced quality of life. Potential relationship between variables identified as being associated with LUTS at night have been summarized in (Figure 2). Eight factors were identified as being on the causal pathway of nocturnal bladder symptoms. Limited mobility appeared as a contributor to LUTSn, incontinence–associated dermatitis and falls.
Discussion
Overall there are few reports detailing bladder dysfunction at night in older people admitted to hospital. This is despite the finding that most of the individual nocturnal lower urinary tract symptoms exist in at least 50% of participants studied. Furthermore, multiple bladder symptoms at night appear to co-exist during hospitalization. From a conceptual framework perspective the issue of nocturnal LUTs is sufficiently prevalent to warrant attention.
This study has identified variables that potentially impact cost during hospitalization in older people with bladder dysfunction at night. On a patient-level the practice of restricting independent mobilization to minimize falls potentially escalates fear of toileting and may transition urinary urgency to incontinence. Sleep disturbance might be expected from multiple care occasions during the night, particularly if this includes changing bedding, clothes and body-worn products. Intangible costs would also be associated with sleep disruption and the resultant daytime fatigue in patients woken during the night. Potential costs accrued to the health service include multiple nursing care moments, continence products, bedding and clothing changes, skin care products, falls injury management and extended length of hospital stay.
Two items extracted during this scoping review of urinary incontinence in older people during hospitalization suggest that the impact of bladder dysfunction is under-appreciated. Firstly, the comment that “urinary incontinence was invisible to staff” and the second that there is “no screening or risk identification of individuals with urinary incontinence” during ward admission. Although staff can provide up to nine occasions of bladder care during the night, incontinence was considered to be “consistently under reported by staff”. The disruption to sleep associated with this style of continence management is readily appreciated. The paradigm shift in community continence care to appreciating that incontinence is a potentially treatable set of symptoms rather than an inevitable age-related dysfunction, was not evident in ward-based care.
Falling was one of the two major identified adverse effects of LUTS at night. Patients in aged care wards are often managed from a falls prevention model rather than with an expectation of independence with toileting. The study identified that selftoileting at night is limited by fear of falling. Fear of falling independently predicts limitations in mobility, while previous falls are themselves cause of limited mobility [17]. Fear of falling is also predicted by poor perception of physical ability and use of a walking aid [18]. Mobility issues contribute to LUTs at night in several ways. Since urinary urgency is prevalent in older people and presents as a sudden pressing need to void, immediate assistance is required to prevent incontinence. A lower staff to patient ratio at night means that toileting assistance is often delayed. Increased nocturnal diuresis generates early bladder filling after falling sleep. Individuals are disrupted during their main period of deep sleep; awaking at this time has been associated with deficits in attention, memory and cognition [2]. Additionally, mobilizing with a full bladder precipitates shorter step length and altered balance shift, both changes known to increase risk of falling [19].
This study highlighted that there is an interplay between low functional skills in bed and at the bedside and reduced independence with toileting during the night. Ward-based rehabilitation focuses primarily on skills to safely ambulate, a criterion for hospital discharge. There may be a need to increase attention from allied health staff to rehabilitating basic bed movement and chair to standing skills as well as components of self-toileting. For example, the combination of using a gait aid while experiencing urgency, manipulating the bathroom door and removing clothes at the toilet without jeopardising balance requires strategies and actual supported practice.
Incontinence-associated dermatitis emerged as a key consequence of bladder dysfunction at night. The prevalence of moisture-associated skin damage during sub-acute hospitalization is at least 22%, but increases markedly in the presence of faecal incontinence [20,21]. Nursing care helps to supplement the skin’s barrier function in reducing the irritation from the chemicals contained in both urine and faeces on the lipid layer in the outer epidermis. Regular change of containment products at night, followed by cleaning and protection of the skin avoids skin breakdown. Since changes to skin can occur after any prolonged contact with urine / faeces preventative care is a priority [22-24].
Nocturia is often considered ‘normal part of aging’ and thus not interesting in a hospital setting. Therefore, it is difficult to establish all the variables behind the attributable cost in a hospital setting. This study should be supported by a prospective observational study following older hospitalized patients to validated the concept pool. There is currently low expectation that LUTS in older inpatients can be improved during hospitalization. Recognition and evaluation of LUTS during the day, followed by diagnostic testing to identify pathophysiology is not routine during hospitalization. However, health services are becoming aware of the need to implement better care for older patients with bladder dysfunction. Implementation of a new model of care for older hospitalized individuals who have coexisting nocturnal urinary tract symptoms is needed. One of the key drivers to sustaining change will be demonstration of cost effectiveness [25].
Conclusion
This study has identified a concept pool from which to develop a cost model to measure the cost benefit of improving continence care at night in older people admitted to hospital.
References
- Hafner M, Pollard J, Troxel WM, Yerushalmi E, Fays C, et al. (2019) How frequent night-time bathroom visits can negatively impact sleep, well-being and productivity: Examining the associations between nocturia, well-being and economic outcomes in a working-age population. Rand Corporation.
- Goel N (2017) Neurobehavioral effects and biomarkers of sleep loss in healthy adults. Current neurology and neuroscience reports 17(11): 89.
- Weidlich D, Andersson FL, Oelke M, Drake MJ, Jonasson AF, et al. (2017) Annual direct and indirect costs attributable to nocturia in Germany, Sweden, and the UK. The European Journal of Health Economics 18(6): 761-771.
- Nakagawa H, Ikeda Y, Kaiho Y, Matsushita M, Hozawa A (2009) Impact of nocturia on medical care use and its costs in an elderly population: 30 month prospective observation of national health insurance beneficiaries in Japan. Neurourology and Urodynamics 28(7): 930-931.
- Nguyen HX, Penukonda S, Stephen S, Whishaw DM, Bower WF (2021) Wake‐up call: 4 out of 5 older hospitalised patients have nocturnal lower urinary tract symptoms. Australasian Journal on Ageing 40(4): 457-460.
- Junqueira JB, Santos VL (2018) Urinary incontinence in hospital patients: prevalence and associated factors . Revista latino-americana de enfermagem 25.
- Bower W, Lau L, Reijnierse E, Maier A (2021) Characteristics of geriatric rehabilitation inpatients with nocturia: resort. Neurourology and Urodynamics 40: S125-S126.
- Chianca TC, Gonçales PC, Salgado PO, Machado BD, Amorim GL, et al. (2017) Incontinence-associated dermatitis: a cohort study in critically ill patients. Revista gaucha de enfermagem 37: e68075.
- Grden CR, Martins AR, Cabral LP, Reche PM, Arcaro G, et al. (2020) Incontinence associated dermatitis in elderly people admitted to a university hospital. Revista Brasileira de Enfermagem 73(suppl 3): e20190374.
- Rose G, Decalf V, Everaert K, Bower WF (2020) Toileting‐related falls at night in hospitalised patients: The role of nocturia. Australasian journal on ageing 39(1): e70-76.
- Decalf V, Bower W, Rose G, Petrovic M, Pieters R, et al. (2021) Prevalence and characteristics of incident falls related to nocturnal toileting in hospitalized patients. Acta Clinica Belgica 76(2): 85-90.
- Van Besien W, Shire S, Decalf V, Ervin CE, King S (2021) The Bladder at Night during Hospitalization: Towards optimal care for elderly patients with nocturia. International journal of clinical practice 15: e14876.
- Brown A, Ferguson L, Whishaw DM, Bower WF (2021) Determinants of bladder care at night on an aged care hospital ward. Neurourology and Urodynamics 40: S124- S125.
- Borges EL, Moraes JT, JA OS, Ghiotto IP, Spinola IS, et al. (2019) Prevalence and Management of Urinary Incontinence in a Brazilian Hospital: A Prospective, Descriptive Study. Wound management & prevention 65(12): 12-20.
- Góes RP, Pedreira LC, David RA, Silva CF, Torres CA, et al. (2019) Hospital care and urinary incontinence in the elderly. Revista brasileira de enfermagem 72(suppl 2): 284-293.
- Góes RP, Pedreira LC, Fonseca ED, Coifman AH, Amaral JB, et al. (2021) Factors inherent to the onset of urinary incontinence in the hospitalized elderly patients analyzed in the light of the Donabedian’s triad. Revista da Escola de Enfermagem da USP 55: e03773.
- Liu M, Hou T, Li Y (2021) Fear of falling is as important as multiple previous falls in terms of limiting daily activities: a longitudinal study. BMC Geriatr 21(1): 350.
- Vellas BJ, Wayne SJ, Romero LJ, Baumgartner RN, Garry PJ (1997) Fear of falling and restriction of mobility in elderly fallers. Age and ageing 26(3): 189-193.
- Paquin M, Duclos C, Dubreucq U, Lapierre N, Rousseau J (2018) Impact of a strong desire to void on gait in continent and incontinent community-dwelling older women who have experienced fall in the last year. Neurourology and Urodynamics 37: S322-S324.
- Beeckman D, Woodward S, Gray M (2011) Incontinence-associated dermatitis: step-by-step prevention and treatment. British journal of community nursing 16(8): 382-389.
- Bliss D, Johnson S, Savik K (2000) Faecal incontinence in hospitalized patients who are acutely ill. Nurs Res 49(2): 101-108.
- Arksey H, O'Malley L (2005) Scoping studies: towards a methodological framework. International Journal of Social Research Methodology 8(1): 19-32.
- Birhanie G, Melese H, Solomon G (2021) Fear of falling and associated factors among older people living in Bahir Dar City, Amhara, Ethiopia- a cross-sectional study. BMC Geriatr 21(1): 586.
- Condon M, Mannion E, Molloy DW, O’Caoimh R (2019) Urinary and faecal incontinence: point prevalence and predictors in a university hospital. International journal of environmental research and public health 16(2): 194.
- Mallinson T, Fitzgerald CM, Neville CE, Almagor O, Manheim L, et al. (2017) Impact of urinary incontinence on medical rehabilitation inpatients. Neurourology and urodynamics 36(1): 176-183.






























