Coronary Artery Disease (CAD): A Case Report
Jessica Zilli Nunes*, Anari Pereira Pieczarka, Diego Melato, Leonardo Soares de Albuquerque Barros, Luiza Alves Daros5, Maria Eduarka Kleis and Elizama de Gregorio
Department of Medicine, University of Alto Vale do Rio do Peixe (UNIARP), Brazil
Submission: October 16, 2020; Published: April 28, 2021
*Corresponding author: Elizama de Gregório, Departament of Medicine, University of Alto Vale do Rio do Peixe (UNIARP), Brazil
How to cite this article: Elizama d G, Anari Pereira P, Diego M, Leonardo S d A B, Luiza A D, et al. Coronary Artery Disease (CAD): A Case Report. OAJ Gerontol & Geriatric Med. 2021; 6(1): 555679. DOI: 10.19080/OAJGGM.2021.06.555679
Abstract
Background: Atherosclerotic disease is the result of several factors, as well as its symptoms, which are commonly associated with somatic pictures. Also, its incidence prevails in the elderly population.
Case presentation: The case presents with an elderly patient referring to thoracic pain, characterized as typical angina and, also, crises that were aggravated by physical efforts. The first tests showed no significant changes and the patient was treated with pain medications and emotional condition. However, after some years the exams showed Coronary Arterial Disease, and the treatment focused on the somatization of the symptoms of the pathology with the depressive picture. However, the effectiveness of the treatment and the disappearance of the symptoms occurred only with the intervention of physical exercises in the routine and improvement of the diet.
Conclusion: The conclusion of the case highlights the need for a global view of the patient and a therapy associated with physical exercise to treat Coronary Arterial Disease.
Keywords: Angina; Pain Thoracic; Coronary Arterial Disease; Frank’s Sign; Drug Interaction; Stents; Aerobic Exercise; Somatization
Abbreviations: SAH: Systemic Arterial Hypertension; CAD: Coronary Arterial Disease; BZDs: Benzodiazepine drug therapy; ASA: Acetylsalicylic Acid; CVA: Cerebral Vascular Accident; ACE: angiotensin conversion enzyme
Introduction
Atherosclerosis or Coronary Arterial Disease is characterized by a chronic inflammatory disease of multifactorial origin that affects the deepest layer of large and medium calibre arteries [1]. This pathological manifestation occurs by the appearance of plaques in response to endothelial aggression [1,2].
Cardiac diseases are commonly associated with anginal pain, which more often than not resolves retrosternal discomfort [3,4]. By this symptomatology, coronary pathological conditions are confused to the clinical state of depression and somatization [5]. In this way, the investigation of the symptomatological peculiarities deliberate effectiveness or failure of the chosen therapy. Currently, with the aging population, the main cause of death has been caused by cardiovascular diseases. In 2015 it was estimated that there were 7.4 million deaths globally, including coronary causes. The WHO still emphasizes the importance of early diagnosis to treat these pathologies.
Case Reports
Female patient, M.Z.N., retired, 71 years old. She has a medical history of Ssystemic Arterial Hypertension (SAH) and somatized angina pain in 2012, retrosternal pain with irradiation for upper limb, accompanied by paresthesia and subsequent coronary angioplasty in 2016, the symptomatic condition and indication of a new catheterization in 2018. At the onset of symptoms, the patient sought medical attention reporting pain in tightness and difficulty breathing during the painful crisis that had been triggered by great efforts. Electrocardiogram, echocardiogram and enzymatic tests were performed; Complementary tests showed normal cardiac rhythm and electrical activity, as well as preserved enzymes. Based on the findings, the diagnostic hypothesis determined an emotional background for the pain, being prescribed drug treatment with Rivotril® and Acetylsalicylic Acid (ASA) for six months. The patient responded well to the treatment, showing improvement in her condition, and progressing to the disappearance of the crises. In September 2016, she sought emergency medical care twice in the event of a painful crisis, being medicated and released. Subsequently, she underwent a medical appointment with a cardiologist whom, on an electrocardiogram, observed non-specific changes in ventricular repolarization and prescribed medication treatment - Amitriptyline, Monocordil®, ASA, Sustrate and Atenolol.
The angina condition progressed negatively, and then she sought the nearest emergency care unit. She was hospitalized for a complaint of retrosternal pain with irradiation to upper limb, accompanied by paresthesia; the day after admission, the patient in bed using morphine, reported no chest pain and no other complaints - stable vital signs. During hospitalization, cardiac catheterization and angioplasty were performed, which revealed mild and moderate lesions in the territories of the proximal and middle-distal artery of the anterior descending artery. Percutaneous intervention with a conventional stent 3.0/15 and 2.25/12 was chosen for proximal and mid-distal segment performed with primary success and adequate final flow. The diagnostic impression of the catheterization expressed severe single-vessel, moderate single-vessel and mild singlevessel atherosclerotic disease; Still, during the procedure there was spasm in the right coronary artery and intracoronary nitrate was administered in the right and left coronary arteries. The intervention used was a femoral technique associated with the Judkins technique. The following day the patient was discharged, with the diagnostic conclusion of Acute Myocardial Infarction; cardiologist return guidelines and drug treatment – ASA 100mg 1 tablet after lunch, simvastatin 40mg 1 tablet in the evening, Brilinta® 90mg 1 12/12 tablet, Monocordil® 20mg 1 tablet 12/12, Bisoprolol 2.5 mg 1 tablet daily, Amitriptyline 1 tablet at night. All medications were prescribed for continuous use, except Brilinta® for 60 days - extended for another 60 days.
After 2 months of angioplasty (December), there was no significant improvement in pain. The Doctor, aiming to investigate the coronary risk stratification, requested the performance of Myocardial Perfusion Scintigraphy. The nuclear medicine exam denies scintigraphic evidence of ischemic and/or cicatricial lesions in the left ventricular myocardium, as well as the GATEDSPECT imaging records showed 67% left ventricular ejection fraction. The cardiologist remained with the same medication management, only further restricting the patient’s daily activities, requesting absolute rest for 30 days and after that period, a slow and gradual return to daily activities.
In the following year, in February 2017, with the persistence of symptoms, the therapeutic approach further restricted the patient’s activities - not allowing sudden movements, holding a weight greater than 1 kg, sweeping, picking up heavy objects from the floor and lifting abruptly, as well as he deliberated her to avoid situations of significant stress or emotional load. The doctor requested Holter’s report which recorded 73 isolated supraventricular extrasystoles, 4 paired and 1 atrial tachycardia with 3 beats. No other tachycardias or pauses longer than 2.5 seconds were detected. The symptom “heart accelerate” was reported seconds after supraventricular extrasystole. The minimum heart rate detected was 49 bpm and the maximum HR was 102 bpm. It is worth mentioning that the symptoms described by “heart accelerate” happened to the events of “lying down”. The findings in the cardiac report did not indicate new behavior, only extended the rest period. Later, in October of the same year, the Electrocardiogram prescribed for follow-up did not show any significant morphological changes; the examination contained a clinical indication of non-cardiac pain - somatization. There was also an indication for an ecodoppler cardiogram, which determined the absence of images suggestive of “shunt”, thrombosis / or intracavitary vegetation. The examination suggests mitral valve reflux and mild tricuspid - allowing to estimate pulmonary artery systolic pressure at 29mmHg (VN <35mmHg).
In the period from 2016 to 2018, the patient was unable to perform some of her daily activities; she reports that she felt “incapable” and depressed; the continuation of painful crises on small efforts continued to happen, and a new catheterization was performed to investigate late coronary angioplasty. The hemodynamic procedure was the catheterization of the left chambers and a cineangiography study of the aorta and its branches - right femoral technique associated with the Judkins technique. The right coronary presented ostial spasm reversed with nitrate - there is an ostial focal lesion of 30%, medial of 40% and distal of 50%. The left main coronary artery is of good caliber, without obstructive lesions; the anterior descending artery has a patent proximal stent; there is a 20% medial focal lesion and a patent medial stent. There is a diagonal branch of moderate caliber that originates in the region of the stent of the anterior descending artery and presents a 99% ostial focal lesion and TIMI II flow. The circumflex artery presents a 50% ostial focal lesion.
The diagnostic impression delimits reversed ostial spasm with monocordile, adapted patent stents, and severe unilateral and moderate bilateral coronary atherosclerotic disease. The examination was performed with an infusion of isosorbide mononitrate in the left coronary artery and the right coronary artery. As of 2018, drug therapy adopted included Vastarel® 35mg 1 tablet in the morning and 1 tablet in the evening, Monocordil® 20mg 1 tablet in the morning and 1 tablet in the evening, Simvastatin 10mg 1 tablet in the evening, Enalapril® 20mg 1 tablet in the evening, ASS 1 tablet after lunch, Sustrate 5mg sublingual in case of pain. Rest had been replaced by light walks that evolved from 10, 20 to 30 minutes daily - afterwards the time was estimated to be at least 30 minutes or free demand. At the beginning of the walks, she felt pain and difficulty breathing; after 2 months, physical activity had a duration of 40 minutes without painful episodes. Nutritional monitoring was also indicated - removing fatty foods, opting for oil-free preparations, decreasing the consumption of red meat. There was a positive progression of the case; the patient is adapted to the treatment and has remained without crises since then. Currently, she reports BP of 120/80 mmHg and reports mild retrosternal discomfort to excessive efforts, especially in activities that need to handle heavy objects. She also reports having decreased from 54 to 50 kg after starting aerobic exercise. She has not used Sustrate in the past 20 months. On inspection, it was possible to observe a positive Frank sign, in which the anterotragal and diagonal lobular folds of the ear undergo a dermatological alteration, making them more evident; it is important to note that the patient does not wear earrings, which could lead to a false positive. Laboratory tests carried out in March 2020 indicated blood count, LDL, HDL and triglyceride levels within the parameters indicated for the age group.
Discussion
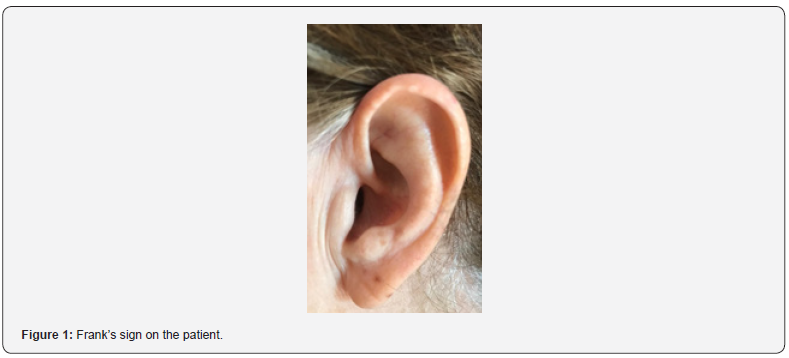
Angina pectoris is characterized as a substernal thoracic pain, which may or may not be irradiated, in order to produce pressure or discomfort [3], in the patient in question, the pain irradiated to MMSS. The expressive retrosternal discomfort evidences a typical angina [4], which increases due to effort and/or emotional stress, as presented by the patient, lasting from 30 to 60 seconds and is attenuated by rest or nitroglycerin [3]. Also, as a symptom, an intermittent sensation of tingling, defined as paresthesia [6]. These symptomatological findings of cardiac pain prove Coronary Arterial Disease (CAD) [7]. And, yet, as a semiological clinical inspection evaluation, a fold was observed in the earlobe that characterizes the positive Frank’s Sign (Figure 1). The earlobe fold (ELC) or Frank’s Sign is a wrinkle that extends from the swallow to the outer edge of the earlobe. Thus, the pathogenic mechanisms that correlate ELC with CAD are explained by an abnormality in collagen metabolism [8].
Benzodiazepine drug therapy (BZDs) is indicated in generalized anxiety and psychotic conditions [9]. Being recommended in the reported case, Clonazepam, to treat the emotional background identified as the probable cause of the patient’s angina. This class of drugs presents great efficacy and low toxicity, so their interactions with other drugs have few risks [10]. Thus, combined with this drug, Acetylsalicylic Acid (ASA) was prescribed, used as a cardiovascular drug, which acts by inhibiting platelet COX-1, being able to reduce its aggregation [11] by decreasing the production of thromboxane A2. With a lower chance of forming thrombi, ASA consequently reduces the risks of Acute Myocardial Infarction and Cerebral Vascular Accident (CVA) [12]. Therefore, ASA was indicated for preventive consumption [13]. A new therapy was indicated for the patient. Using Amitripitiline, a tricyclic antidepressant, used to inhibit the capture of noraepinephrine [14], in this case it was recommended to treat the emotional condition. In contrast, this drug should be avoided in older adults for stimulating cholinergic effects [14].
The use of Amitripitiline when associated to morphine, made by the patient to relieve pain crises, causes an increase in the absorption of the opioid that aggravates its toxicity and the risk of respiratory depression [15]. To relieve the symptoms of angina, isosorbide mononitrate, a drug that dilates blood vessels, increasing blood flow and decreasing oxygen demand, was indicated [16]. The interaction between mononitrate and tricyclic antidepressants, such as Amitriptyline, causes a lower absorption of isossorbide, since the cholinergic effect of Amitriptyline decreases salivation [17]. Also, this class of antidepressant drugs can potentiate the hypotension caused by isosorbide [17]. Propatilnitrate is a medicine used for the treatment of angina pectoris [18], characterized as a substernal pain, with pressure or discomfort, which can be aggravated by efforts and emotional stress, as exposed in the clinical picture [1]. Atenolol is a beta-blocker used to treat hypertension and angina [19], also recommended to prevent acute myocardial infarction [20], but in the latter it is not very effective. Thus, the use of ASA complements this function [12].
The pharmacological therapy has been replaced. The use of Amitriptyline has been maintained. Sinvastatin was introduced to treat atherosclerotic disease, as it acts as a hypolipemic agent and reduces possible heart diseases [21], with use of 40mg per day, a dose recommended for adults and the elderly [18]. Bisoprolol is a cardiosselective beta-blocker, used to treat hypertension, in this case, replacing Atelonol. Its dose is presented in an adequate manner [22]. However, the use of this drug combined with AAS reduces the action of beta-blockers [23]. Also, the use of Isosorbide Mononitrate with 20mg twice a day was maintained, a dose recommended for this type of treatment [16]. The ticagrelor, with commercial name Brilinta, acts inhibiting platelet formation, yet, associated with AAS reduces the risk of acute coronary syndrome and myocardial infarction [24]. The last change in drug therapy was the one that best fitted the patient. Bisoprolol was replaced as a hypertensive medication by Enalapril Meleate, which acts as an inhibitor of the angiotensin conversion enzyme (ACE). Its daily dose can reach 40mg, in this case 20mg was recommended [25]. Also, Isossorbida, Sinvastatina and AAS were maintained. Trimetazidine was added, being a drug with cardioprotective and cardioischemic properties, which differ from beta-blocking agents, and acts as an antianginous agent [26]. It was recommended sustrate in case of angina pectoris crises.
To assist in the drug therapy, the implantation of cardiac Stent in the patient was performed, acting to restore blood flow [27,28]. In order to characterize the stenosis, a percentage analysis is performed, analyzing the diameter of the compromised vessel in comparison to the portion immediately beside preserved, usually the proximal segment [27,28]. The coronary lesion is considered significant when it exceeds 50% of the diameter, in the related case the obstruction exceeded 70%, being this percentage necessary for the Angioplasty intervention [27,28]. After the procedure, the ideal would be that the vessel returns to the previous state the pathological condition, however, as in the case, what happens is the permanence of a certain degree of impairment of the flow [27]. For this reason, the therapeutic conduct chosen was the implantation of a stent, considering the patient individually, with a certain and specific condition, taking into account the risk-benefit ratio of the procedure [27,28]. In recent years several guiding guidelines have been established; the universally diffused guideline is divided into Recommendation Class and Level of Evidence [27].
The guideline does not overlap, however, with the individual responsibility of health professionals to make appropriate decisions, so the final diagnosis or therapy established should be the responsibility of the medical professional, as well as the patient; it should be a joint action - explain the guideline that considers the level of evidence and success, associated with the medical practice of the responsible professional [27]. The adoption of the recommended treatment for the patient, due to the reduction of stenosis via stent, aimed mainly to avoid the symptomatologic picture and avoid Acute Myocardial Infarction, since the use of drugs was not efficient [27,28]. Also, the percutaneous intervention by stent implantation, compared to the clinical drug treatment, in a randomized study, proved to be potentially effective in the clinical improvement of Angina, with the majority being classified as unstable Angina or Myocardial Infarction [28].
In addition, in order to enhance the treatment, the patient was prescribed the regular practice of aerobic exercises. Aerobic exercise is defined as activity that uses several muscle and may be maintained rhythmic mode and continuously, some examples include dancing, cycling, running, swimming and walking [29]. These activities may improves the aerobic capacity that is considered as the capacity of the cardiorespiratory system into supply oxygen to body and the capacity of muscles to utilized this oxygen [30]. A robust evidence body has demonstrated the benefits of physical exercise in several parameters such as lipoprotein profile [31,32]”type”:”article-journal”,”volume”:”334”},”uris”: [“http://www.mendeley.com/documents/?uuid=005db60b- 1 f f 9 - 4 1 8 f - 9 d 9 7 - e 4 1 e 1 c 0 b 7 d d 7 ” ] } , { “ i d ” : ” I T E M - 2 ”,” i t e m D a t a ” : { “ D O I ” : ” 1 0 . 1 0 5 6 / N E J M o a 0 2 0 1 9 4 ”, ”ISSN”:”00284793”,”PMID”:”12421890”,”abstract”:”Background: Increased physical activity is related to reduced risk of cardiovascular disease, possibly because it leads to improvement in the lipoprotein profile. However, the amount of exercise training required for optimal benefit is unknown. In a prospective, randomized study, we investigated the effects of the amount and intensity of exercise on lipoproteins. Methods: A total of 111 sedentary, overweight men and women with mild-to-moderate dyslipidemia were randomly assigned to participate for six months in a control group or for approximately eight months in one of three exercise groups: high-amount-high-intensity exercise, the caloric equivalent of jogging 20 mi (32.0 km, increased insulin sensitivity [33], improved cognition function [34], decreased psychosocial stressors and determent of depression [35,36]. Moreover, in a prospect study involving 73.743 women 50 to 79 years of age demonstrated that walking and also vigorous exercise are associated with reductions in the incidence of cardiovascular events among [37]as compared with vigorous exercise, in the prevention of cardiovascular disease remains controversial. Data for women who are members of minority racial or ethnic groups are particularly sparse. Methods: We prospectively examined the total physical-activity score, walking, vigorous exercise, and hours spent sitting as predictors of the incidence of coronary events and total cardiovascular events among 73,743 postmenopausal women 50 to 79 years of age in the Women’s Health Initiative Observational Study. At base line, participants were free of diagnosed cardiovascular disease and cancer, and all participants completed detailed questionnaires about physical activity. We documented 345 newly diagnosed cases of coronary heart disease and 1551 total cardiovascular events. Results: An increasing physical-activity score had a strong, graded, inverse association with the risk of both coronary events and total cardiovascular events. There were similar findings among white women and black women. Women in increasing quintiles of energy expenditure measured in metabolic equivalents (the MET score. The European Society of Cardiology has recommend that people with chronic stable angina should do moderate-to-vigorous intensity aerobic exercise at least 30 min per session 3 times a week [38]. These dates demonstrate an effective intervention non-medicament able of decreased incidence of cardiovascular events in people with angina stable [38].
According to the patient’s initial symptoms and no imaging findings, the first suspicion was somatic disease. Summatization can be characterized as a defense against suffering, since it can be a way to mask depression [5]. It is composed of somatic symptoms, which include physical symptoms: chest pain and fatigue, reported by the patient, and dizziness that cause discomfort, being considered by traditional medicine as a process of physiological disease [39]. Somatic symptoms are often more associated with the individual’s brain and emotional functions [39]. In a study performed by Harris et al. (2008), it was observed that somatic patients present greater functional incapacity and more impairment compared to non-summing patients [40]. Moreover, patients with somatic problems spend more days in bed, have a greater impairment of function, as reported in the case, higher rates of unemployment and need more medical certificates [40]. Somatic symptoms are more common in patients with a negative perception of their health, besides depression and anxiety disorder [41]. The somatization is difficult to diagnose, since the medical practice, according to Descartes, is focused on the biological situation of the patient, excluding the psychological and social issue, a fact that leaves doctors unprepared to deal with patients who somatize [42]. Moreover, referrals and exacerbated exams are requested to analyze the health of the patient with somatic problems, causing higher costs to the health system and putting the patient in possible situations of risk [42].
Given the above case, we conclude the need to have a global view on the patient, since the complementary tests did not elucidate the disease diagnosed. Accordingly, Frank’s sign, if observed at clinical inspection, could have been indicative of early diagnosis. The drug therapy best adapted was the combination of Bisoprolol, Enalapril Meleate, Isosorbide, Sinvastatin, Trizemetazidine and ASA, associated with Sustrate in case of pain. In addition, regular aerobic exercise has proved crucial in controlling the symptomatologic picture. This conjuncture highlights the importance of new studies on Coronary Arterial Disease and its correlations, since the demographic and epidemiological conjuncture illustrates the growing population aging.[43-45].
Acknowledgement
We thank the patient M.Z.N. for the availability of the case and for all the details and exams granted.
Conflict of Interest
There are no conflicts of interest between the authors of the article.
References
- Faludi André Arpad, Izar Maria Cristina de Oliveira, Saraiva José Francisco Kerr, Chacra Ana Paula Marte, Bianco Henrique Tria et al. (2017) Atualização da Diretriz Brasileira de Dislipidemias e Prevenção da Aterosclerose. Arq Bras Cardiol 109(2 Suppl 1): 1-76.
- Afiune Neto, Abrahão, Mansur, Antonio de Pádua, Avakian, Solange Desirée et al. (2006) Monocitose é um marcador de risco independente para a doença arterial coronariana. Arquivos Brasileiros de Cardiologia 86(3): 240-244.
- Kloner RA, Chaitman B (2017) Angina and Its Management. J Cardiovasc Pharmacol Ther 22(3): 199–209.
- Chequer, Graziela (2015) Segunda opinião formativa: que aspectos devem ser considerados na avaliação da dor torácica crônica? Apoio ao Diagnóstico.
- Ned H Kalin MD (1991) Somatization and psychiatric disorder in the NIMH Epidemiologic Catchment Area study. Official Am J Psychiatry 148(11): 1494-1500
- Dehbashi Sara, Jin Peter, Edelschick, Donald, Shin Susan (2020) Clinical Reasoning: A 53-year-old woman with lower extremity paresthesias. Neurology 94(24): 1105-1108.
- Parry M, Bjørnnes AK, Victor JC, Ayala AP , Lenton, E, et al. (2018) Self-Management Interventions for Women With Cardiac Pain: A Systematic Review and Meta-analysis. Can J Cardiol 34(4): 458–467.
- Del Brutto Oscar H, Costa Aldo F, Mera Robertino (2018) Intracranial Atherosclerosis And The Earlobe Crease (Frank’s Sign). A Population Study Rev Ecuat Neurol 27(3): 20-24.
- Larine, Lourival (2008) Fármacos e Medicamentos. Editora Artmed Porto Alegre Brasil (1ª Edição) 395 pá
- Singh I, Oosthuizen F (2019) A retrospective review on benzodiazepine use: A case study from a chronic dispensary unit. S Afr Med J 109(2):127-132.
- Katzung, Bertram G, Masters, Susan B, Trevor, Anthony J (2014) Farmacologia Básica e Clí Editora Artmed Porto Alegre Brasil (12ª Edição) 1228 páginas.
- Cucchiara BL, Messé SR (2019) Antiplatelet therapy for secondary prevention of stroke. Up To Date.
- Valentini G, Huscher D, Riccardi A, Fasano S, Irace R et al. (2019) Vasodilators and low-dose acetylsalicylic acid are associated with a lower incidence of distinct primary myocardial disease manifestations in systemic sclerosis: results of the DeSScipher inception cohort study. Ann Rheum Dis 78(11): 1576–1582.
- Snyder MJ, Gibbs L M, Lindsay TJ (2016) Treating Painful Diabetic Peripheral Neuropathy: An Update. Am fam physician 94(3): 227–234.
- Melgaço, Tainah Brasil et al. (2011) Polifarmácia e ocorrências de possíveis interações medicamentosas. Revista Paraense de Medicina 2(1) 25-85.
- Balasubramanian S, Chowdhury YS (2020) Isosorbide. Stat Pearls Publishing.
- Marcolin, Marco Antonio, Cantarelli, Maria da Graça, Garcia Junior et al. (2004) Interações farmacológicas entre medicações clínicas e psiquiá Rev psiquiatr clín 3(2) 70-81.
- Rosito, Guido Aranha, Kuchenbecker, Ricardo, Berwanger, et al. (2007) Terapêutica Cardiovascular: Das evidências para a prática clí Editora Artmed Porto Alegre Brasil (1ª Edição) 527 páginas.
- Rehman B, Sanchez DP, Shah S (2020) Atenolol. StatPearls Publishing.
- Wiysonge CS, Bradley HA, Volmink J, Mayosi BM, Opie LH (2017) Beta‐blockers for hypertension. Cochrane Database of Systematic Reviews 1: CD002003.
- Al Rasheed NM, Hasan IH, Al Amin MA, Al Ajmi HN, Mohamad RA (2017) Simvastatin Ameliorates Diabetic Cardiomyopathy by Attenuating Oxidative Stress and Inflammation in Rats. Oxidative medicine and cellular longevity 2017: 1092015.
- Bisoprolol (2017) LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. National Institute of Diabetes and Digestive and Kidney Diseases.
- De Mesquita, Josiane Costa, Fábio Vinícius Ferreira SilvaGeovana Rodrigues de OliveiraJanaína Vidal Bezerra et al. (2020) Análise e identificação das principais interações medicamentosas predominantes em unidade de terapia intensiva de um hospital privado. Revista Eletrônica Acervo Saúde 45: e994-e994.
- Wang D, Yang XH, Zhang JD, Li RB, Jia M, Cui XR (2018) Compared efficacy of clopidogrel and ticagrelor in treating acute coronary syndrome: a meta-analysis. BMC cardiovascular disorders 18(1): 217.
- Enalapril (2018) LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. National Institute of Diabetes and Digestive and Kidney Diseases.
- Ciapponi A, Pizarro R, Harrison J (2017) WITHDRAWN: Trimetazidine for stable angina. The Cochrane database of systematic reviews 3(3): CD003614.
- The Task Force on myocardial revascularization of the European Society of Cardiology (ESC) and European Association for Cardio-Thoracic Surgery (EACTS) (2019) ESC (40): 87–165.
- Fausto Feres, Ricardo A Costa, Dimytri Siqueira, J Ribamar Costa Jr, Daniel Chamié et al. (2017) Diretriz da sociedade brasileira de cardiologia e da sociedade brasileira de hemodinâmica e cardiologia intervencionista sobre intervenção coronária percutânea. Arq Bras Cardiol 109 (1): 1-81.
- A Wahid, N Manek, M Nichols, P Kelly, C Foster et al. (2016) Quantifying the Association Between Physical Activity and Cardiovascular Disease and Diabetes: A Systematic Review and Meta-Analysis. J Am Heart Assoc 5 (9):
- LC Dalleck, JS Tischendorf (2012) Guidelines for Exercise Testing and Prescription (ACSM) In: Encycl Lifestyle Med Heal, SAGE Publications Inc, 2455 Teller Road Thousand Oaks California 91320 United States of America.
- PT Williams (1996) High-density lipoprotein cholesterol and other risk factors for coronary heart disease in female runners. N Engl J Med 334 (20): 1298–1303.
- WE Kraus, JA Houmard, BD Duscha, KJ Knetzger, MB Wharton JS et al. (2002) Effects of the amount and intensity of exercise on plasma lipoproteins. N Engl J Med 347: 1482-1492.
- M Rosenthal, WL Haskell, R Solomon, A Widstrom, GM Reaven (1983) Demonstration of a relationship between level of physical training and insulin-stimulated glucose utilization in normal humans. Diabetes 32 (5): 408-411.
- WW Spirduso (1980) Physical Fitness, Aging and Psychomotor Speed: A Review. J Gerontol 35: 850–865.
- DD Lobstein, BJ Mosbacher, AH Ismail (1983) Depression as a powerful discriminator between physically active and sedentary middle-aged men. J Psychosom Res 27 (1): 69-76.
- DJ Crews, DM Landers (1987) A meta-analytic review of aerobic fitness and reactivity to psychosocial stressors, Med Sci Sports Exerc 19 (5): 114-120.
- JE Manson, P Greenland, AZ LaCroix, ML Stefanick, CP Mouton et al. (2002) Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med 347: 716-725.
- Montalescot G, Sechtem U, Achenbach S, Andreotti F, Arden C, et al. (2013) ESC guidelines on the management of stable coronary artery disease. Eur Heart J 34: 2949‐
- Feng Zheng, Yinglong Duan, Jingle Li, Lin Lai, Zhuqing Zhong, et al. (2019) Somatic symptoms and their association with anxiety and depression in Chinese patients with cardiac neuroses. Medical Research J 47(10) : 4920-4928.
- Ashley M Harris, E John Orav, David W Bates, Arthur J Barsky (2008) Somatization Increases Disability Independent of Comorbidity. J Gen Intern Med 24(2): 155–161.
- O Gureje , GE Simon, TB Ustun, DP Goldberg (1997) Somatization in cross-cultural perspective: a World Health Organization study in primary care. Am J Psychiatry 154(7): 989-995.
- Celina DS Lazzaro, Lazslo A Ávila (2004) Somatization in general medical practice.
- EM Ohman (2016) Chronic Stable Angina. N Engl J Med 374: 1167-1176.
- R Ferrari, PG Camici, F Crea, N Danchin, K Fox et al. (2018) Expert consensus document: A “diamond” approach to personalized treatment of angina. Nat Rev Cardiol 15 (2): 120-132.
- L Jespersen, A Hvelplund, SZ Abildstrom, F Pedersen, S Galatius et al. (2012) Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur Heart J 33: 734-744.






























