The Role of Models and Formulations in the Management of Behaviors that Challenge in Dementia
Barbara Medea1, Marta Roberts1, Rosie Dunn3 and Ian Andrew James*1
1CNTW NHS Foundation Trust, UK
2University of Hull, UK
Submission: September 16, 2020;; Published: October 07, 2020
*Corresponding author: Ian Andrew James, Campus for Ageing and Vitality, Westgate Road, Newcastle upon Tyne, UK
How to cite this article: Medea B. Roberts M. Dunn R. James I.A. The Role of Models and Formulations in the Management of Behaviors that Challenge in Dementia. OAJ Gerontol & Geriatric Med. 2020; 5(5): 555671. DOI: 10.19080/OAJGGM.2020.05.555671
Abstract
The British Psychological Society’s Briefing Paper for Behaviors that Challenge (BtC) in dementia states that psychological formulation helps in the development of effective and well targeted treatments [1].While not explicitly using the term psychological formulation, the 2018 NICE UK Dementia Guidelines support the use of systematic problem-solving approaches in the management of BtC. The current paper gives an overview of the content of a number of formulation models developed in this area and contrasts two established models. This article looks at two different ways of understanding people’s agitation – one which emphasizes the reasons for their behaviour in terms of the person with dementia [2] and the other called DICE [3]which puts equal emphasis on the roles of both caregivers and the environment in explaining behaviors. We suggest that, while the Newcastle Model tacitly suggests a role for caregivers and the environment in BtC, the explicit emphasis in DICE encourages a more holistic understanding of agitation.
Introduction
National guidelines on Behaviors that Challenge (BtC) in dementia routinely suggest the trialing of psychological treatments prior to the use of psychotropic medication, owing to the problematic side-effects of many of the medications used in dementia [4]. To remind us of the NICE [5] guidance on the topic, here is their statement outlining the guidelines regarding pharmacological and non-pharmacological approaches, known to professionals as the ‘psychology first’ initiative [6]. Before starting non-pharmacological or pharmacological treatment for distress in people living with dementia, conduct a structured assessment to:
a. Explore possible reasons for their distress and check for and address clinical or environmental causes (for example pain, delirium, or inappropriate care).
b. As initial and ongoing management offer psychosocial and environmental interventions to reduce distress in people living with dementia.
c. Only offer antipsychotics for people living with dementia who are either:
At risk of harming themselves or others or experiencing agitation, hallucinations or delusions that are causing them severe distress [7].
Unfortunately, NICE, in common with other guidelines on the same topic [8], do not offer specific guidance on the alternatives to drugs in terms of the theory, rationale and practicalities of implementing non-drug approaches. This lack of clarity is likely to have unintentionally perpetuated the use of medication as the main response to BtC in many clinical settings [9].In order to support care settings to adhere to NICE guidance the alternatives to pharmacological approaches need to be operationalized. Psychological formulation can play a major role in supporting non-pharmacological approaches to BtC [10,11] and in the development of the ‘psychology-first’ initiative. Indeed, when used effectively formulations can provide well targeted interventions across a range of clinical settings, including inpatient and community services.
The original idea for this article was to complete and update the review of BtC formulation undertaken by Holle and colleagues [12] Indeed, when we examined her data set we found that she had missed some key formulations in the original 2016 paper and some of her descriptions required amending. We also wanted to update the systematic review with newer models published after her cut-off point of 2014. Over the course of writing our paper, however, we have recognized that such reviews are challenging, and their quality depends greatly on the sources of the models on which one chooses to base one’s descriptions. In truth to undertake a systematic review correctly one would need to contact each model’s author and ask for primary and updated sources in order to describe the models accurately. Such actions were beyond the scope of the current paper, and we settled for identifying models not included in [12] article both new and old. Hence, we provide a description of each model, but overtly acknowledge that we have taken details about the model from only the source we have cited in this paper. The current paper also seeks to identify trends in the development of the models, noting that many new models have been produced in the recent past. In order to illustrate developmental changes, we contrast an early client-centered model with a newer holistic approach. The model representing client-centered approaches is the Newcastle model [2,13] and it was chosen because it is the most widely used model in the UK. The holistic example is DICE [3] which conceptualizes BtC in terms of the person, the caregiver and environment.
Best practice guidelines on BtC
In the last ten years several best practice guidelines regarding the management of BtC have been published [14] Dementia Behaviour Management Advisory Services – [15] International Psychogeriatric Association [16], the following common themes emerge from them. First, all the guidelines discuss the impact that cognitive deficits have on the person’s life, in addition to the physical and social changes involved with both the diagnosis of dementia and age-related decline. For example, the IPA [16,17] highlights the impact of intellectual, sensory and communication difficulties and their links to distress and agitation. More specifically, the ReBOC guidelines from Alzheimer’s Australia, frame the agitation displayed by some people with dementia within a combined biomedical and stress model. From a biomedical perspective the dementia causes damage to different areas of the brain which might directly impact on a person’s behavioural repertoire. At the same time the dementia lowers a person’s ability to deal with daily stresses and increases their susceptibility to environmental stressors. As a consequence of these two processes, BtC should be seen neither as intentional nor deliberate acts of aggression.
Second, there is an agreement that BtC have multiple root causes and it is the professional’s responsibility to observe the behaviour and develop causal hypotheses [18]. ‘Reus and colleagues [8] specify the use of ABC charts to aid hypotheses and detect patterns, and to determine frequency, severity, pattern, and timing of symptoms. Potential causes to consider for BtCs are physical health (e.g., pain, discomfort), the environment (e.g., excessive noise, bright lights), cognitive impairment (e.g., frontal lobe deficits), emotional/mental health history (e.g., depressive symptoms), and social difficulties (e.g., interpersonal problems, loneliness). The authors of the stepped care approach [14] stress the importance of integrating the above information with other relevant individual features such as religious beliefs, spiritual and cultural identity. They also discuss the value of integrating the information prior to hypothesis generation and testing. Third, all the guidelines tend to suggest that the choice of approach depends on the outcome of the assessment. If clear physical causes (pain, constipation, infection) or psychoses are identified, drug management is often appropriate. In most other circumstances, however, non-pharmacological approaches are regarded as first line interventions, apart from situations of high risk where sedating medication may be required immediately [5]. In some cases, a non-pharmacological approach equates to ‘watchful waiting’, meaning the refraining from any intervention [19,14].
Fourth, person-centered approaches [20] are the preferred philosophy. As such BtCs are interpreted as an expression of some form of unmet need, rather than willful or conscious challenges to the caregivers [21,22]. Finally, the guidelines suggest a number of management strategies.
Two of the main lines of intervention are:
a. The removal of potential triggers (i.e., negative caregiver interactions or environmental cues) [15,7]
b. Adding meaningful and personalized activities to allow for the satisfying of specific unmet needs
Importantly, Brechin and colleagues [14] stress the importance of integrating the above information within a conceptual framework, and thus endorse the use of a formulation. The value of formulation is further commended by the BPS’ professional guidelines [11], which states: “Central to the management of behaviors that challenge is both ensuring that the needs of the person with dementia are met and resolving any unmet needs, using individually formulated biopsychosocial approaches to intervention. The formulation aims to actively treat episodes of behaviors that challenge and prevent their frequency or escalation. Clinicians and staff working to minimize behaviors that challenge should be aware of biopsychosocial formulation in which behaviour and associated needs are identified.” [11].
Overview of formulation-led interventions
In 2016, Holle and colleagues systematically reviewed formulation-led interventions for BtCs published between 1995 and 2014 and identified 14. The authors carried out an analysis of the structural and process features of these models and looked at the outcomes of these formulations on people with dementia and their careers. This review showed that all of the formulation approaches in dementia are based on the assumption that BtCs arise from an interaction of biological, psychological and social factors. Moreover, formulation approaches usually have four processes: assessment of the behaviour, analysis of the causes of the behaviour, intervention, and evaluation (What’s the problem? This is what’s going on; This is what we need to do; Has it worked?). However, there seems to be a wide variation in the operationalization of such phases, especially in terms of the analysis of the causes of BtCs and the proposed tools to carry this out. Holle and colleagues could not make any judgements regarding which approaches were the most effective due to the lack of clear definitions of outcomes in some studies, the lack of specific information on the timeline/amount of intervention delivered, and who were the targets of the interventions (i.e. staff or the person with dementia).
While Holle’s review was helpful, such a summary of the literature proved challenging. This is because the primary sources of the models are usually difficult to identify, and the key papers used as sources may not provide adequate descriptions of the true nature of the models. An example of this challenge is the overview that Holle provided of the ‘Newcastle approach’. Firstly, this model was misattributed and then the analysis of its content failed to illustrate changes to its development over the 20 years of its existence [23]. As part of the current paper we updated Holle’s list of formulations. (Table 1) presents an overview of the features of five frameworks missing in Holle’s paper, and another five new models published since her review. It is important to note that the features identified are taken from the paper cited alongside the model and, again, may not fully represent any recent adaptations or improvements. While this caveat may limit the value of the analyses, it was felt to be important to provide readers with an idea of the extent and nature of the models available to them (Table 1). As shown in (Table 1), all the models analyze the person’s behaviour and mental health and the majority also take the physical and/or social environment into consideration. Moreover, most of the models explore either the type of dementia or the nature of the cognitive changes the person is going through as well as their physical health. However, fewer than 50% of the frameworks collect details about either premorbid personality or the medications the person is prescribed. Overall, this brief summary echoes findings that the assessment frameworks informing the formulation focus on the person with dementia. This is not surprising as it is in line with the rationale of a ‘personcentered’ approach where collecting relevant information about the person help us better understand the potential causes of the BtC. Once we understand the causes of the BtC, we can then treat those causes that are reversible and establish strategies that meet people’s needs. The implicit method of change operating in these types of frameworks is that by gaining insight into the causes of the BtC, the caregivers are more likely to engage in a range of pharmacological and non-pharmacological strategies that will reduce the triggering of the problematic behaviors.
A typical example of client-focused formulation framework
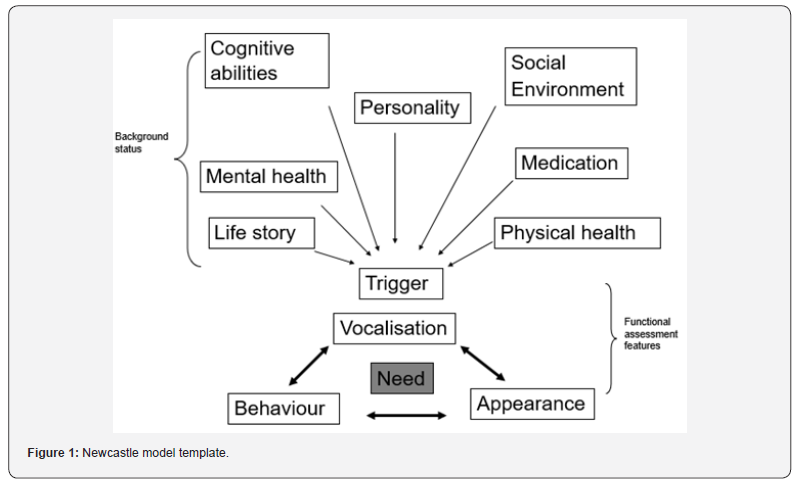
One of the frameworks that exemplifies an approach that chiefly formulates the experiences of the person with dementia is the Newcastle model. There were very few models being used when it was developed in 1999, and it is now the most widely used approach in the UK. It is the grandparent of many of the more recent conceptual models (e.g., FITS, CLEAR, CEASE, etc.; see (Table 1). The Newcastle approach, which has undergone many helpful revisions in recent years, aims to identify potential biological, psychological and social causes of BtC. In order to do this, caregivers are assisted in populating a template of relevant features which, once put together, offers an overview of the patterns and mechanisms underpinning the BtCs (Table 1).The underpinning psychological principle of the Newcastle model is that BtCs are the result of unmet needs. Eight needs are considered as part of this model (freedom from discomfort/pain, emotional security, sense of love and belonging; control; esteem; positive touch; meaningful occupation; fun). Further, the model contains a least four progressive phases:
a. An assessment phase, where relevant information is collected in collaboration with the caregivers. As part of this phase diaries and assessment charts are used to identify the triggers of the BtC. The outcome of the assessment should be an agreed and unified account of the problem.
b. A formulation phase, which consists in scaffolding staff, helping them to populate the formulation map where a diagram will show both background features and the functional assessment of the BtC.
c. Treatment planning and support phase. In this phase a care plan is created based on what emerged from the formulation map.
d. Evaluation of the care plan through the use of questionnaires and observations. (Figure 1) Newcastle model template
As shown in (Figure 1), the Newcastle model contains many of the features outlined in both the best practice guidelines and the models reported in (Table 1). The positives of this model were that it was one of the first biopsychosocial models in the field; it was coproduced with local care home staff and it was used and adopted by non-psychologists very early on. However, the translation from formulation to intervention has often proved challenging clinically. For many staff using the model the focus has become the populating of the boxes within the model, and the process features seemed to have been viewed as being less important. The process features of the model include collaborative assessment; information sharing sessions; scaffolding; coaching of caregivers, etc. The latter’s omissions are a real problem because the process of formulating can help the carers develop an understanding of the person and generate empathy towards their behaviors.

To be effective, a formulation of BtC must serve the following functions:
a. Provide explanations for the behaviors that are both clear and acceptable to the staff and caregivers. The formulation needs to be parsimonious and make sense to the caregivers. Hence, complex patterns of behaviour need to be presented in simple ways.
b. Help to explain the behaviors in a way that encourages empathy and a motivation within the caregivers to change their own approaches in order to bring about changes in the person with dementia.
c. The information must present ‘recognizable’ solutions to the BtC. The formulation must lead intuitively to the production of a care plan, which converts the ideas developed within the formulation into realistic actions. A good formulation will present information in such a way that the caregivers will be able to immediately identify feasible ways of altering their behaviors to deal with the BtCs.
In order to meet the above functions, the formulation has to be co-produced with the staff and caregivers. In fact, it is recognized that some level of input from those intending to implement the formulation-led care plans is essential to bring about change. As highlighted in the previous paragraph, the majority of the content of the formulation of BtC focuses on details of the person with dementia. This is because all of the recent frameworks come from a ‘person-centered’ tradition which emphasizes the notion of ‘personhood’. A valuable expansion of this approach is provided by Kales and colleagues who have produced a framework called DICE. The DICE framework is described by the authors as “compatible with the ‘person centered’ approach commonly used in Europe” (p.13); however, in our view, this model adds some extra value to its compatibility by extending its focus to the context and systems around the person with dementia. Hence, this is worth exploring further.
A broader contextual formulation approach
The DICE framework was developed in 2014 by a group of experienced US psychiatrists and clinicians following a series of consensus meetings aimed at devising a protocol for the management of BtC. It is specifically designed for people living in their own homes. The DICE (Describe, Investigate, Create, Evaluate) framework suggests that there are three areas which need to be the focus of assessment and intervention: the person, the career, and the environment. In the Describe phase, a description of the behaviour and the context in which it manifests is elicited. This is important to clarify potential triggers to the behaviour. In the Investigate phase, the possible causes of the behaviors are explored. The causes are divided in patient factors (e.g., infection which has led to delirium), care giving factors (e.g., communication issues) and environmental contributions (e.g., overstimulating or under stimulating). In the Create phase, a treatment plan is devised in collaboration with the caregivers, the person with dementia and the team around them. Again, the key interventions will relate to the patient, caregiver and environment. Interventions can be pharmacological or non-pharmacological. In the Evaluate phase, the intervention is evaluated for its effectiveness and depending on the outcome the recommendations can be changed.
In our view, there are aspects of this model that make it an important addition to other formulation frameworks. For example, although some clinicians may suggest that the roles of ‘carers’ and ‘environmental’ features are addressed in other ‘person-centered’ models, like the Newcastle model, there is far greater emphasis on the psychology of the caregiver in DICE. As much attention is placed on the abilities of the carers to deal with the situation as on the person with dementia. In part, the focus on the caregiver may be due to DICE having been solely designed for ‘own-home’ scenarios. A further attractive feature of DICE is that it presents a flow diagram demonstrating the causal and maintaining factors for the person’s agitation that clearly indicates where the intervention should focus in terms of the person with dementia, caregiver and environment [3]. In fact, the management plan is clearly mapped onto this flow diagram making it not only easy to use but also providing a clear rationale for what is assessed and treated. As such, DICE provides very specific guidance regarding what to assess and treat using a checklist approach (e.g., rule out acute medical problems; educate staff about BtC and the ‘broken brain’; teach staff to use tailored activities prior to person getting agitated).
Overall, the DICE flow diagram identifies key components for the BtC and their relationships, a mechanism of change, and builds assessment and management strategies around these structures. In terms of future BtC guidelines, this is the sort of level of content at which we must operate. At the same time, there are some aspects of this model that appear problematic. Firstly, while the checklist approach is helpful, it tends to reduce the amount of integration between the various aspects of the model. If the approach does not integrate aspects of the information collected in the first phase of the formulation, clinicians are unable to generate a meaningful explanation for the behaviour. This is also problematic because developing rationales by weaving the various information together is the key method in generating hypotheses and testing them [24]. Of note, DICE does not refer to the term formulation in its articles or textbook. Another issue associated with DICE is that the approach is trademarked which means that it cannot be adapted without permission of the authors, and the materials and tools used in services in the other countries would need to be markedly changed to comply with the DICE framework. The lack of adaptation is an important problem because DICE was developed exclusively for own-home settings and would require changing for use in 24hour care settings.
Formulation-approaches moving forward
This paper has discussed two established approaches to the management of BtCs. On balance, there appears to be some advantages to adopting a holistic approach as it seems to capture and manage the complex dynamics underpinning BtC, and it may be particularly helpful for more severe BtC. DICE is a good representation of a holistic approach and it is likely to have an impact within the UK, and elsewhere, once it has become better established. Unfortunately, because of its failure to incorporate a process for integrating information and the inflexibility resulting from being trademarked, there remain considerable obstacles regarding its use. As such we would like to see the development of other holistic models. We are not the only clinicians to have such ideas, a team in Switzerland have already produced an alternative to DICE called DATE (Describe, Analyse, Treat, Evaluate – [25]. DATE has not been well articulated thus far but shares many aspects with DICE. In terms of our own work in the UK an early version of a holistic model has been produced and is currently being tested on our inpatient wards [26-27]. An article outlining the model is available from the corresponding author (IJ).
Conclusion
Twenty years ago, there were a small number of formulations for the management of BtC. At the present time there are over twenty published frameworks. In this article, we have updated Holle’s recent systematic review providing details of some of the new (and omitted) models from the original survey. In order to illustrate developmental changes in the use of formulation approaches, we have presented and contrasted an early clientcentered model, the Newcastle model [2], with a newer holistic approach, the DICE [3]. Although the DICE framework does not refer to itself as a formulation, its structure is a good example of an integrated management approach in the treatment of BtC. We suggest that the use of holistic formulation approaches, such as DICE, can help better capture the complex dynamics underpinning BtC. Recommendations have been given around important elements that formulations should cover both to be effective and to contribute to positive changes in the management of BtC in dementia.
Acknowledgment
The authors thank Kristina Gray for her intellectual assistance in preparing this article for publication.
References
- James I, Moniz-Cook E (2018) Behaviors that Challenge in Dementia. A Briefing Paper for British Psychological Society: Leicester.
- James IA (1999) Cognitive conceptualization of distress in dementia. Clinical Psychology Forum, 133, 21-25.
- Kales HC, Gitlin LN, Lyketsos CG (2015) Assessment and management of behavioral and psychological symptoms of dementia. BMJ 2: pp. 350.
- Buckley JS, Salpeter SR (2015) A risk-benefit assessment of dementia medications: systematic review of the evidence. Drugs & Aging, 32(6): 453-467.
- National Institute for Health and Care Excellence (2018) Dementia - assessment, management and support for people living with dementia and their carers (NICE guideline NG97).
- James IA (2019) Formulations in Behaviors that Challenge. FPOP National Conference. Southport
- Pink J, O’Brien J, Robinson L, Longson D (2018) Dementia: assessment, management and support: summary of updated NICE guidance. BMJ 361.
- Reus VI, Fochtmann LJ, Eyler AE, et al. (2016) The American Psychiatric Association practice guideline on the use of antipsychotics to treat agitation or psychosis in patients with dementia. American Journal of Psychiatry, 173(5): 543-546.
- Wood-Mitchell A, James IA, Waterworth A, Swann A, Ballard C (2008) Factors influencing the prescribing of medications by old age psychiatrists for behavioural and psychological symptoms of dementia: a qualitative study. Age and Ageing, 37(5): 547-552.
- James IA (2015) The use of CBT in dementia care: a rationale for Communication and Interaction Therapy (CAIT) and therapeutic lies. The Cognitive Behaviour Therapist.
- Moniz-Cook E, James IA (2018) Evidence Briefing: Behaviour that challenges in dementia. British Psychological Society. BPS Publishing.
- Holle D, Halek M, Holle B, Pinkert C (2017) Individualized formulation-led interventions for analyzing and managing challenging behavior of people with dementia–an integrative review. Aging & mental health, 21(12): 1229-1247.
- James IA (2011) Understanding Behaviour in Dementia that Challenges: A guide to assessment and treatment. Jessica Kingsley: London.
- Brechin D, Murphy G, James I, Codner J (2013) Alternatives to Antipsychotic Medication: Psychological Approaches in Managing Psychological and Behavioural Distress in People with Dementia. British Psychological Society Publications.
- Dementia Behaviour Management Advisory Services. (2012) ReBOC: Reducing Behaviours of Concern. Australian Alzheimer Society Publications.
- International Psychogeriatric Association (2012) The IPA Complete Guides to Behavioral and Psychological Symptoms of Dementia-Specialists Guide. Draper B, Henry B, Sanford FI, editors. Milwaukee, WI: International Psychogeriatric Association.
- International Psychogeriatric Association (2016) The IPA Complete Guides to Behavioral and Psychological Symptoms of Dementia-Specialists Guide. International Psychogeriatric Association.
- NHS Protect (2013) Meeting needs and reducing distress: guidance on the prevention and management of clinically related challenging behaviour in NHS settings. NHS Protect.
- University of Exeter (2018) Optimizing treatment and care for people with behavioural and psychological symptoms of dementia.
- Kitwood T (1997) The experience of dementia. Aging & Mental Health 1(1): 13-22.
- Algase DL, Beck C, Kolanowski A, Whall A, Berent S (1996) Need-driven dementia-compromised behavior: An alternative view of disruptive behavior. American Journal of Alzheimer's disease 11(6): 10-19.
- Cohen Mansfield J (2000) Theoretical frameworks for behavioral problems in dementia. Alzheimer's Care Today 1(4): 8-21.
- Marshall J, James IA, Carter LJ (2020) Meeting the Needs of People living in Care Homes during the Covid-19 Pandemic: UK perspective. Tees, Esk and Wear Valley NHS Foundation Trust.
- Reichelt K, Moody L, Wells J, James IA (2019) Formulating and formulations in dementia care: Reviewing our perspectives. Psychology of Older People: The FPOP Bulletin. 148: 17-25.
- Tible OP, Riese F, Savaskan E, von Gunten A (2017) Best practice in the management of behavioural and psychological symptoms of dementia. Ther Adv Neurol Disord 10(8): 297-309.
- Cohen Mansfield J, Libin, Marx (2007) Nonpharmacological treatment of agitation: a controlled trial of systematic individualized intervention. J Gerontol A Biol Sci Med Sci 62(8): 908-916.
- Dexter-Smith S (2010) Integrating psychological formulations into older people’s services. PSIGE Newsletter. BPS 112: 3-7.
- Duffy F (2016). ‘Look at all of me’ - a CLEAR model for dementia care. Journal of Dementia Care 24(3):27-30.
- Edgar F (2017) Mnemonic techniques: how to CEASE stress and distress. Journal of Dementia Care. 25(5): 32-34.
- Gitlin L, Winter L, Burke B, et al. (2009) Tailored activities to manage neuropsychiatric behaviors in persons with dementia and reduce caregiver burden: a randomized pilot study. Am J Geriatr Psychiatry 16(3): 229-239.
- James IA (2011) Understanding Behaviour in Dementia that Challenges: A guide to assessment and treatment. Jessica Kingsley: London.
- James IA, Birtles H (2020) Twenty-one years of creativity and development: The evolving Newcastle model. Psychology of Older People. The FPOP Bulletin.4(12): 1093-1098.
- James IA, Jackman L (2017) Understanding Behaviour in Dementia that Challenges: a guide to assessment and treatment. 2nd edition Jessica Kingsley Publishers. 41(5): 699.
- James IA, Mahesh M, Duffy F et al. (in press) UK clinicians’ views on the use of formulations for the management of BPSD: A multidisciplinary survey. Ageing and Mental Health.
- James IA, Reichelt K (2019) Understanding people’s needs: the 8-needs framework for the treatment of behaviours that challenge. Psychology of Older People: The FPOP Bulletin 147: 24-30.
- Kolanowski A, Litaker M, Buettner L et al. (2011) A randomized clinical trial of theory-based activities for the behavioral symptoms of dementia in nursing home residents. J Am Geriatr Soc 59(6): 1032-1041.
- Lichtwarck B, Selbaek G, Kirkevold O et al. (2018) Targeted interdisciplinary model for evaluation and treatment of neuropsychiatric symptoms: A cluster randomized controlled trial. The American Journal of Geriatric Psychiatry 26(1): 25-38.
- Sells D, Howarth A (2018) Caregiver appraisal model understanding and treating behaviour that challenge. Journal of Dementia Care 26(5): 22-27.
- Teri L, Huda T, Gibbons L et al. (2005) STAR: A dementia-specific training program for staff in assisted living residences. The Gerontologist. 45(5): 686-693.
- Tees, Esk, Wear, Valleys (2017) Case 5 John. In Chapter 11: Case studies. In I. James & L. Jackman, Understanding Behaviour in Dementia that Challenges (2nd Ed) (Marshall, 2017). (page 192).






























