Clinical and Bacteriological Profile of Older Patients with Acute Exacerbation of Chronic Obstructive Pulmonary Disease
Anand P Ambali1* and Jayanth S Shanthakumar2
1Department of Medicine and Geriatric Clinic, BLDE (Deemed to be University), Shri B M Patil Medical College Hospital and Research Centre, India
2Department of Medicine and Geriatric Clinic, BLDE (Deemed to be University), Shri B M Patil Medical College Hospital and Research Centre, India
Submission: May 14, 2019; Published: June 18, 2019
*Corresponding author: Anand P Ambali, Professor, Department of Medicine and Geriatric Clinic, BLDE (Deemed to be University), Shri B M Patil Medical College Hospital and Research Centre, Vijayapura, Karnataka, India
How to cite this article: Ambali AP, Jayanth S S. Clinical and Bacteriological Profile of Older Patients with Acute Exacerbation of Chronic Obstructive 002 Pulmonary Disease. OAJ Gerontol & Geriatric Med. 2019; 5(1): 555652. DO 10.19080/OAJGGM.2019.05.555652
Abstract
Background: Acute Exacerbation of Chronic Obstructive Pulmonary Disease (AECOPD) results in substantial worsening of the general condition and decrease in quality of life in older people (>60 Years).
Aim and Objectives: To identify and establish clinical and bacteriological profile and antibiotic sensitivity pattern in sputum culture of older patients with acute exacerbation of chronic obstructive pulmonary disease
Material and Methods: prospective study carried out in 66 older people of AECOPD admitted in medical college hospital
Results: The mean age group of patients was 70.63 years. Male outnumbered female. Pulmonary function test revealed obstructive pattern in 75.7% patients. Streptococcus pneumoniae was the most common organism isolated in 16(24.2%) patients. Majority of the organisms isolated were sensitive to Cefoperazone antibiotic. The overall mortality rate is 1.5%.
Conclusion: Knowledge of bacteria prevalent in our locality would implicate the sensitivity patterns of AECOPD in patients and would facilitate an early introduction of a proper antibiotic, reducing the mortality, morbidity and improving the prognosis and quality of life among the older patients. Holistic approach and Immunization prevent future exacerbations.
Keywords: Older people Chronic Obstructive Pulmonary Disease Bacteriological profile.
Introduction
Chronic obstructive pulmonary disease (COPD) is characterised by the slowly progressive impairment of airflow in lung function and worsening of breathlessness, exercise capacity and impairment of quality of life with time [1,2]. The rate of decline varies from individual to individual. In, a subset of patients, this steady decline is punctuated in the natural course by episodes of increased symptoms, labelled as “acute exacerbations”. Exacerbations are acute worsening of clinical condition in COPD patients. An acute exacerbation of COPD (AECOPD) was defined in the GOLD 2014 update as “an acute event characterized by worsening of the patient’s respiratory symptoms that is beyond normal day-to-day variations and leads to a change in medication” [1].
The high prevalence of COPD has made the disease a leading cause of morbidity and mortality worldwide which induces an economic and social burden [3]. AECOPDs account for the largest proportion of the COPD burden on the healthcare system. According to the National Commission of Macroeconomics and Health (NCMH) estimates, there were 17 million COPD patientsin India in year 2006 and the estimated economic burden of COPD in India is Rupees 350 Billion [4]. Treating COPD and associated comorbidities require institutional resources and there is a need of regular hospitalizations which can be cumbersome for the individuals as well as the health system. The rate of hospitalization can be four times among older people when compared to younger ones. The mean length of hospital stays for COPD ranges from 4.5 to 16 days in normal to intensive care. Moreover, the social structure of India does not provide adequate protection to the older people resulting into less adherence to the treatment.
Among the episodes of AECOPD, more than 75% the of episodes are incited by infections [5]. Environmental pollution has also been implicated in a small proportion of patients up to 10% [6]. Decreased air temperature, increased exposure to sunshine, and decreased humidity were also found to be responsible for triggering exacerbations of COPD. The proof that bacterial infections are the causation factors for AECOPD comes from the isolation of pathogens from the lower respiratory tract secretions obtained by different techniques during episodes of exacerbations.
Various studies on isolation of pathogens associated with AECOPD suggested that the presence of pathogens was clinically and geographically unpredictable.
Old age and comorbidity go hand in hand in misdiagnosing and undertreating COPD in them. There is a disparity between practice guidelines and treatment among the COPD in older patients. The management of older patients with COPD should encompass a multidisciplinary approach. Along with assessment of the lung ventilator performance and functional impairment, nutritional status, mental health and social issues should be evaluated. Knowledge of local bacterial aetiology and antibiotic sensitivity patterns of acute exacerbation of chronic obstructive pulmonary disease facilitates early introduction of proper antibiotics which can reduce the morbidity, mortality and improve the prognosis. The data about the bacteria involved in AECOPD in our area is sparse and very less studied. Hence, the following study was undertaken to study the bacteriological profile and antibiotic sensitivity pattern in sputum culture of older patients with AECOPD.
Materials and methods
This prospective observational cross-sectional study was conducted in Shri B M Patil Medical College Hospital and Research centre, BLDE (DU), Vijayapura. A total of 66 patients aged more than 60 years diagnosed with acute exacerbation of chronic obstructive pulmonary disease over a period of twenty-four months were included in the study. All patients were interviewed as per the prepared proforma and then complete clinical and laboratory examination were conducted.
i. Inclusion Criteria: All the patients above 60 years of age with clinical symptoms like increased cough, expectorations,increased severity of dyspnoea for over 3 months in a year for 2 consecutive years supported by pulmonary function test for the diagnosis suggestive of COPD were included in the study. Even previously diagnosed patients of COPD based on exposure to risk factors, clinical history and examination supported by pulmonary function test were included
ii. Exclusion Criteria:Patients with active pulmonary tuberculosis, lung malignancy, bronchiectasis, patients who were already on antibiotic treatment for exacerbation of COPD and acute severe asthma were excluded from the study. Informed written consent was obtained from all the study group subjects. Ethical clearance of the study was obtained from the institutional ethical committee.
iii. Specimen Collection: Early morning expectorated sputum samples were obtained from the cases that were clinically diagnosed to have AECOPD. The samples were then transported to Microbiology laboratory for gram stain and culture.
iv. Culture Methods: Sputum quality was assessed both macroscopically and microscopically. Sputum samples were subjected to gram staining and were reported according to Bartlett’s grading system and a score of 1 or above was considered as suitable sample [7]. The sputum samples were inoculated onto Mac Conkey’s Agar, chocolate agar and two blood agar plates. On one blood agar streaking with Staphylococci was done to facilitate the growth of Haemophilus influenzae. All the plates were inoculated for 24 hours at 37 degree Celsius for 24 hours in 7-10 % CO2 concentration. Using standard microbiological technique, the organisms were identified [8]. Antimicrobial susceptibility of the isolates was determined by Kirby Bauer disk diffusion method on Muller Hilton agar plates according to Clinical and laboratory Standard Institute Guidelines [9].
Results
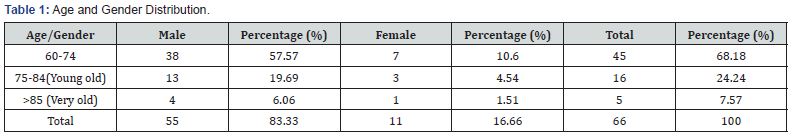
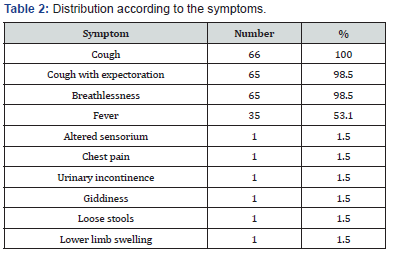
The age group of patients varied from 60 to 91 years with a mean age of 70.63 years. 55(83%) of the patients were males and 11(17%) were females (Table 1). The common symptom at presentation was cough in 100%, while cough with expectoration was seen in 98.5%. Breathlessness was the second most common symptom seen in 98.5%, followed by fever in 53.1% (Table 2). Among the atypical symptoms were chest pain, altered behaviour, hiccups, giddiness, urinary incontinence and reduced appetite. Among the comorbid conditions, Hypertension was noted in 15(23%) Type 2 Diabetes Mellitus seen in 6(9%). Old Pulmonary Tuberculosis was seen in 5(8%) and Ischemic Heart Disease in 3(4.5%) patients. Multiple comorbidities were noted in 6(9%).
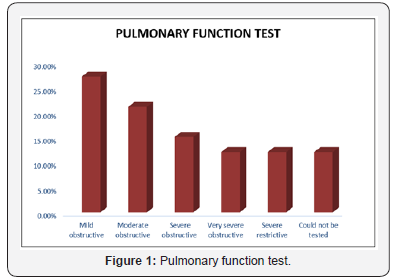
The common finding on Electrocardiogram was P Pulmonale in 62.1% followed by right ventricular hypertrophy. All the patients in the study had features of emphysematous chest on chest radiography. Pulmonary function test was conducted in 58 patients in the study participants. Among them 50(75.7%) patients showed obstructive and 8(12.3%) showed restrictive pattern (Figure 1). On gram staining of the sputum, Gram positive cocci were isolated from 39.3%, Gram negative bacilli in 22.7%, and mixed organisms in 10.6% of the patients (Table 3).

Pulmonary function test (PFT) was done in 58 patients. It could not be done in 8 patients; 4 among them were ventilated initially and later after extubating, the patients refused owing to the seriousness of the illness and 4 were unable to complete the procedure. The PFT revealed mild obstructive pattern in 18(27.7%) patients, moderate obstructive pattern in 21%, severe obstructive in 15.15% and very severe obstructive pattern in 12.12% patients. This was classified according to the GOLD 2017 Classification of severity of airflow limitation. In our study 8(12.12%) patients had severe restrictive pattern (Figure 1).
Bacteriological isolation by sputum culture showed Streptococcus pneumoniae as the most common isolated organism in 24.2%, followed by Klebsiella pneumoniae in 12.1% and Pseudomonas aeruginosa and Staphylococcus aureus each in 9.1% patients. Multiple organisms were isolated from 2 patients, Streptococcus pneumoniae and Acinetobacter species in one patient and Streptococcus pneumoniae and Klebsiella pneumoniaein another patient. No pathogenic bacteria were isolated in 13(19.69%) patients (Table 4).
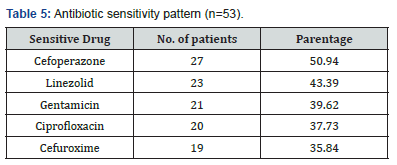
Antibiotic sensitivity revealed organisms sensitive to cefoperazone was 51%, Linezolid in 43%, Gentamicin in 40%, and Ciprofloxacin in 38% of patients (Table 5). Streptococcus pneumoniae, which was the most common isolate, was sensitive to Cefoperazone, Linezolid, Piperacillin and Clindamycin in decreasing frequency. Klebsiella pneumoniae isolates were sensitive to Amikacin, Ciprofloxacin, Gentamicin and Cefuroxime. Pseudomonas aeruginosa isolates were sensitive to Amikacin, Cefoperazone, and Piperacillin. Staphylococcus aureus isolates were sensitive to Cefoperazone, Cefuroxime, Clindamycin and Gentamicin.

One male patient with AECOPD died in hospital with mortality rate of 1.5%.
Discussion
Chronic obstructive pulmonary disease is a chronic noncommunicable disease and its prevalence dramatically increases with age and leads to decreased quality of life in older people. COPD exacerbations are the leading cause of morbidity and mortality and early introduction of empirical antibiotics, can improve outcome and reduce mortality [10].
In this study, the age group of patients varied from 60 to 91 years. Mean age was 70.63 years. Majority of the patients (45) were in the age group of 60-74 years, which constituted 68.2 % of the total patients. It is like the study conducted by Babu D et al. [11] where 74.5% of the patients were between 60-79 years. Increased incidence of AECOPD in males was observed, 55(83%) were males and 11(17%) were females. It was like the study conducted by Shashibhushan B L et al. [12] where 84% of the patients were males and 16% females.
Among habits, smoking alone was predominant in 30.3% of the patients. Multiple habits like smoking, tobacco chewing, and alcohol consumption altogether were seen in 26% patients and smoking and tobacco chewing together in 12.1% patients. In total, 82% of patients in the present study were smokers. Identical observations were made by Syed A et al. [13] where 85% of the patients were smokers and S B Lal et al. [14] where 95% of the patients were smokers. No history of smoking was reported by female patients like the observations in the study by Syed A et al. [13]. All the female patients had sustained exposure to indoor pollution mainly from cooking fumes for almost four decades.
The presenting symptoms were cough in 100%, Cough with expectoration in 98.5% which was like study by S B Lal et al. [14] and Arora N et al. [15]. Breathlessness was second most common symptom in 98.4% like study by Arora N et al. [15] where it was 98.2%. Fever was presenting symptom only in 53.1% which is contradicting to the studies reported by Arora N et al. [15] and Kulkarni G et al. [16]. Gram staining predominantly showed gram positive organisms. This finding was contrary to other studies reported by Sharan H et al. [17], Aleemullah M F et al. [18], and Babu D et al. [11] where gram negative bacteria were isolated predominantly.
In our study, predominantly isolated organism was Streptococcus pneumoniae, followed by Klebsiella pneumoniae, Pseudomonas aeruginosa and Staphylococcus aureus. The observations were like the studies conducted by Arora N et al. [15], Shashibhushan B L et al. [12], Patel A K [10], and Syed A et al. [13] where Streptococcus pneumoniae was the most common bacteria isolated. Contrary to this, the studies conducted by Babu D et al. [11], Sharan H et al. [17], and Narayanagowda D Set al. [19] found out Klebsiella pneumoniae to be the most common bacteria causing exacerbations. No pathogenic bacteria were isolated in 13 (19.7%) patients in our study. This was less when compared to the studies done by Narayanagowda D S et al. [19] where 63% yielded no bacteria, and by Babu D et al. [11] where 57% yielded no bacteria.
Streptococcus pneumoniae, which was the most common isolate, was sensitive to Cefoperazone, Linezolid, Piperacillin and Clindamycin in decreasing frequency like the study conducted by Kulkarni G et al. [16]. Klebsiella pneumoniae isolates were sensitive to Amikacin, ciprofloxacin, Gentamicin and cefuroxime. In the study done by Narayanagowda D S et al. [19] Klebsiella pneumoniae was sensitive to Ampicillin, Ciprofloxacin andNetilmicin. A study by S B Lal et al. [14] study demonstrated sensitivity to a combination of Levofloxacin and Gentamicin.
Staphylococcus aureus isolates were sensitive to Cefoperazone, Cefuroxime, Clindamycin and Gentamicin. The study by Narayanagowda D S et al. [19] found Staphylococcus aureus to be sensitive to Amoxyclavulinate, Penicillin, Erythromycin, Gentamicin, Amikacin, Netilmicin and Co-trimoxazole.
Conclusion
Chronic obstructive pulmonary disease is a chronic noncommunicable disease and its prevalence dramatically increases with age and leads to decreased quality of life in older people. Exacerbations of COPD in older people result in substantial worsening of the general condition of them and depression in quality of life. Older patients with exacerbations can present with both typical and atypical complaints. None of the patients had received pneumococcal or influenza vaccine in past. Older People with AECOPD may not perform pulmonary function test fully owing to the decreased physical capacity and cognitive impairment. Bacterial infection is the most common triggering factor for exacerbations of COPD in older people. Streptococcus pneumoniae was the most common bacteria isolated in our study. Most of the organisms isolated in our study were sensitive to Cefoperazone. Knowledge of the bacteria with their sensitivity pattern resulting in exacerbations in the local geographical area would help in immediate and prompt management of them. Adequate awareness regarding the immunization among the older people with COPD, their caregivers and the treating doctor would prevent many exacerbations and hence improves quality of life. The management of elderly patient with COPD should encompass a multidisciplinary and holistic approach. They require special attention because of high susceptibility to infections, polypharmacy, multiple comorbidities, disabilities, dependency, financial and social issues.
References
- Strategy G (2014) The FOR, Of P, Obstructive C, Disease P. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. Glob Initiat Chronic Obstr Lung Dis, USA.
- British thoracic society. British guideline on the management of asthma Key To Evidence Statements And Grades Of Recommendations (2014). Scottish Intercoll Guidel Netw.
- Adeloye D, Chua S, Lee C, Basquill C, Papana A, et al. (2015) Global and regional estimates of COPD prevalence: Systematic review and meta–analysis. J Glob Health 5(2)
- Murthy KJR,Sastry JG (2005) Economic burden of chronic obstructive pulmonary disease: NCMH Background Papers Burden of Disease in India.
- Jindal SK, Aggarwal A N, Chaudhry K, Chhabra SK, D Souza G a, et al. (2005) A multicentric study on epidemiology of chronic obstructive pulmonary disease and its relationship with tobacco smoking and environmental tobacco smoke exposure. Indian J Chest Dis Allied Sci 48(1): 23-29.
- Murray CJ, Lopez AD (1996) Evidence-based health policy-lessons from the global burden of disease study. Science 274(5288): 740-3.
- Mokkapati A, Yalamanchili M (2013) Correlation of sputum gram’s stain and culture in lower respiratory tract infections. IOSR Journal of Dental and Medical Sciences 8(1): 6-9.
- Collee JG, Miles RS, Watt B (2006) Tests for the identification of bacteria. In: Collee JG, Marmion BP, Fraser AG, Simmons A (Eds) Tests for the identification of bacteria 14thedn Churchill Livingstone London pp. 131-49.
- (2011) Performance standards for antimicrobial susceptibility testing; Twenty first informational supplement. In: Performance standards for antimicrobial susceptibility testing; Twenty first informational supplement 29th edn Clinical and Laboratory Standards.
- Patel AK (2015) Sputum Bacteriology and Antibiotic Sensitivity Pattern of Patients Having Acute Exacerbation of COPD in India? A Preliminary Study. J Pulm Respir Med 5(01): 1–4.
- Babu D, Abraham L, C BR, Majeed HP, Cr SB,et al. (2017) Sputum Bacteriology in Patients having Acute Exacerbation of Chronic Obstructive Pulmonary Disease in a Tertiary Care Hospital. Int J Med Res Heal Scienes 6(9): 1–5.
- Shashibhushan BL, Nagaraja C, Arun BJ, Nagaraj N (2016) Bacteriological profile and antibiotic sensitivity pattern in sputum culture of chronic obstructive pulmonary disease patients. International Journal of Advances in medicine 3(3): 671–674.
- Syed A, Saleem SM, Shafiq S, Khursheed S (2017) Hospital based cross sectional study on bacteriological isolates of acute exacerbation of chronic obstructive pulmonary disease patients. Int J Curr Adv Res 6(7): 4680–4683.
- Lal SB, Kumar KR, Sudeena D (2017) Profile of bacterial culture and sensitivity from the sputum of chronic obstructive pulmonary patients with acute exacerbations. Asian Pac J Health Sci 4(1): 173–82.
- Arora N, Daga MK, Mahajan R, Prakash SK, Gupta N (2001) Microbial pattern of acute infective exacerbation of chronic obstructive airway disease in a hospital based study. Indian J Chest Dis Allied Sci 43(3): 157–162.
- Kulkarni G, Chaudhary D, Bhoyar A, Dugad S, Telkhade A (2017) Bacteriological Profile in Sputum and their Antibiogram among the Patients of Acute Exacerbation of COPD. MVP Journal of Medical Sciences 4(2): 113–117.
- Sharan H (2015) Aerobic Bacteriological Study of Acute Exacerbations of Chronic Obstructive Pulmonary Disease. J Clin Diagn Res 9(8): 10-12.
- Aleemullah MF, Krishnamurthy V, Harish M, Akeel CA (2016) Bacteriological Profile of Patients with AECOPD- Hospital Based Study. Int.J.Curr.Microbiol.App.Sci 5(4): 84–90.
- Narayanagowda DS, Golia S, Jaiswal J, Manasa SS (2015) A bacteriological study of acute exacerbation of chronic obstructive pulmonary disease over a period of one year 3(11): 3141–6.
- Strategy G (2014) The FOR, Of P, Obstructive C, Disease P. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. Glob Initiat Chronic Obstr Lung Dis, USA.
- British thoracic society. British guideline on the management of asthma Key To Evidence Statements And Grades Of Recommendations (2014). Scottish Intercoll Guidel Netw.
- Adeloye D, Chua S, Lee C, Basquill C, Papana A, et al. (2015) Global and regional estimates of COPD prevalence: Systematic review and meta–analysis. J Glob Health 5(2)
- Murthy KJR,Sastry JG (2005) Economic burden of chronic obstructive pulmonary disease: NCMH Background Papers Burden of Disease in India.
- Jindal SK, Aggarwal A N, Chaudhry K, Chhabra SK, D Souza G a, et al. (2005) A multicentric study on epidemiology of chronic obstructive pulmonary disease and its relationship with tobacco smoking and environmental tobacco smoke exposure. Indian J Chest Dis Allied Sci 48(1): 23-29.
- Murray CJ, Lopez AD (1996) Evidence-based health policy-lessons from the global burden of disease study. Science 274(5288): 740-3.
- Mokkapati A, Yalamanchili M (2013) Correlation of sputum gram’s stain and culture in lower respiratory tract infections. IOSR Journal of Dental and Medical Sciences 8(1): 6-9.
- Collee JG, Miles RS, Watt B (2006) Tests for the identification of bacteria. In: Collee JG, Marmion BP, Fraser AG, Simmons A (Eds) Tests for the identification of bacteria 14thedn Churchill Livingstone London pp. 131-49.
- (2011) Performance standards for antimicrobial susceptibility testing; Twenty first informational supplement. In: Performance standards for antimicrobial susceptibility testing; Twenty first informational supplement 29th edn Clinical and Laboratory Standards.
- Patel AK (2015) Sputum Bacteriology and Antibiotic Sensitivity Pattern of Patients Having Acute Exacerbation of COPD in India? A Preliminary Study. J Pulm Respir Med 5(01): 1–4.
- Babu D, Abraham L, C BR, Majeed HP, Cr SB,et al. (2017) Sputum Bacteriology in Patients having Acute Exacerbation of Chronic Obstructive Pulmonary Disease in a Tertiary Care Hospital. Int J Med Res Heal Scienes 6(9): 1–5.
- Shashibhushan BL, Nagaraja C, Arun BJ, Nagaraj N (2016) Bacteriological profile and antibiotic sensitivity pattern in sputum culture of chronic obstructive pulmonary disease patients. International Journal of Advances in medicine 3(3): 671–674.
- Syed A, Saleem SM, Shafiq S, Khursheed S (2017) Hospital based cross sectional study on bacteriological isolates of acute exacerbation of chronic obstructive pulmonary disease patients. Int J Curr Adv Res 6(7): 4680–4683.
- Lal SB, Kumar KR, Sudeena D (2017) Profile of bacterial culture and sensitivity from the sputum of chronic obstructive pulmonary patients with acute exacerbations. Asian Pac J Health Sci 4(1): 173–82.
- Arora N, Daga MK, Mahajan R, Prakash SK, Gupta N (2001) Microbial pattern of acute infective exacerbation of chronic obstructive airway disease in a hospital based study. Indian J Chest Dis Allied Sci 43(3): 157–162.
- Kulkarni G, Chaudhary D, Bhoyar A, Dugad S, Telkhade A (2017) Bacteriological Profile in Sputum and their Antibiogram among the Patients of Acute Exacerbation of COPD. MVP Journal of Medical Sciences 4(2): 113–117.
- Sharan H (2015) Aerobic Bacteriological Study of Acute Exacerbations of Chronic Obstructive Pulmonary Disease. J Clin Diagn Res 9(8): 10-12.
- Aleemullah MF, Krishnamurthy V, Harish M, Akeel CA (2016) Bacteriological Profile of Patients with AECOPD- Hospital Based Study. Int.J.Curr.Microbiol.App.Sci 5(4): 84–90.
- Narayanagowda DS, Golia S, Jaiswal J, Manasa SS (2015) A bacteriological study of acute exacerbation of chronic obstructive pulmonary disease over a period of one year 3(11): 3141–6.






























