Glycemic Outcomes Resulted from Collaborative Care in a Primary Care Practice
Nazli Parast1,2*, Heather Williams1,2, Christelle P Cleroux3 and Tina Leech1,2
1 Community Diabetes Education Program of Ottawa (CDEPO), Canada
2 Centretown Community Health Centre, Canada
3 Carlington Community Health Centre, Canada
Submission: May 30, 2018; Published: June 06, 2018
*Corresponding author:Nazli Parast, Community Diabetes Education Program of Ottawa (CDEPO), Canada.
How to cite this article: Nazli P, Heather W, Christelle P C,Tina L.Glycemic Outcomes Resulted from Collaborative Care in a Primary Care Practice. OAJ Gerontol & Geriatric Med. 2018; 4(3): 555640. DOI: 10.19080/OAJGGM.2018.04.555640
Background
Collaboration between the client, diabetes educator and primary care provider (PCP) is an integral part of diabetes management. Around 80% of people living with diabetes have their diabetes managed in a primary care setting [1]. This is a study based on the work of 2 Diabetes Educators from the Community Diabetes Education Program of Ottawa (CDEPO) providing client care alongside PCPs in a Community Health Centre primary care setting one day per week. Anti hyperglycemic agent adjustment recommendations are made to PCPs when glycemic targets are not being met.
Purpose
To assess and improve clients’ glycemia in a collaborative practice between PCPs of CCHC and CDEPO.
Methods
Retrospective analysis of referrals from the Community Health Centre to CDEPO. Outcomes were measured using blood glucose and HbA1C values. A period of 6 months was analyzed: April 1- September 30, 2016.
Results
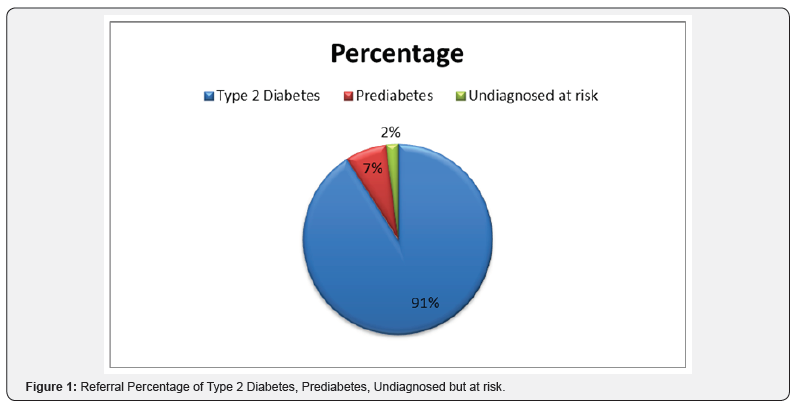
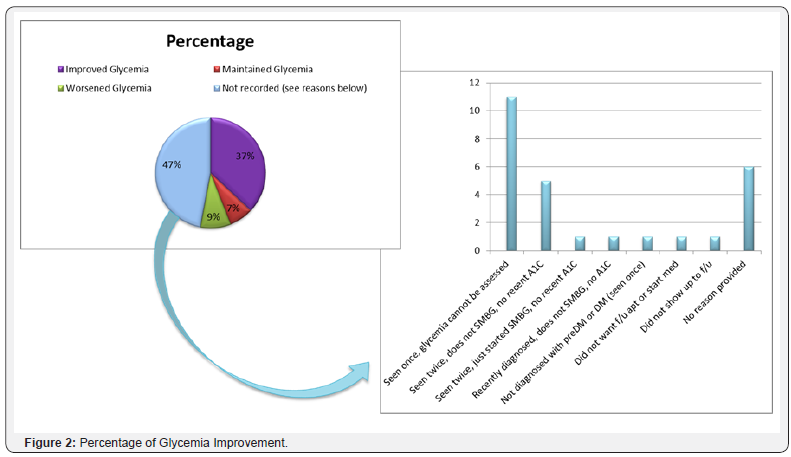
Fifty-seven clients were referred to the Diabetes Educators; 91% had type 2 diabetes 7% had pre-diabetes; 2% were high risk but not diagnosed (Figure1). Among the 91% with diabetes, 37% showed improved glycemia, 47% could not be properly assessed and 7% maintained their glycemic control. Glycemia declined in 9%, mainly due to other comorbidities (Figure 2). Out of the 47% whose glycemia could not be assessed, the main cause was lack of follow-up. These results identified the need for emphasis on client follow-up.
Discussion
Over a 1/3 of the clients demonstrated positive glycemia management results. However, a higher percentage of clients did not provide the necessary information for glycemia to be assessed (Self-management behaviours; i.e. blood work or SMBG not being completed). A possible rationale is the lack of trust between the clients and healthcare providers. Therefore, one of the most important areas that should continue to be addressed by the Diabetes Educators during these visits is the development of trust in order to help promote client’s participation in their care. This may take a longer time for some clients which is possibly the reason for the lack of glycemia assessment during this time period. Of importance to note, the majority of the population being seen by the Diabetes Educators at Carlington CHC are above 60 years old and have some degree of mental health issues such as schizophrenia, bipolar disorder, major depressive disorder, etc; while, some of these clients suffer from multiple mental health issues. Research signifies the importance of building trust and understanding trust in individuals living with mental health issues [2].
Conclusion
Diabetes Educators need to continue to build trusting relationships over-time with clients in order to promote diabetes self-management behaviours and therefore, improve glycemia outcomes. Seeing clients in the primary care setting allows for better collaboration between the primary health care providers (diabetes educators and PCP) which are the foundation for building trust with clients.
Next Step
Diabetes Educators will continue to focus on building trusting relationships through regular follow-ups with clients. Further study needs to be done by performing a longer term assessment of the impact of glycemia in the same population.






























