Depression and Care Strategies in Elderly People
Rukuye Aylaz*1 and Erman Yyldyz2
1Department of Public Health Nursing, Nursing Faculty, Inonu University, Malatya, Turkey
2Department of Psychiatric Nursing, Nursing Faculty, Inonu University, Malatya, Turkey
Submission: April 04, 2018; Published: April 17, 2018
*Corresponding author: Rukuye Aylaz, Department of Public Health Nursing, Nursing Faculty, Inonu University, Malatya, Turkey, Email: rukiye.aylaz@inonu.edu.tr
How to cite this article: Rukuye A, Erman Y. Depression and Care Strategies in Elderly People. OAJ Gerontol & Geriatric Med. 2018; 4(1): 555628. DOI: 10.19080/OAJGGM.2018.04.555628
Abstract
The increase in the frequency and duration of depression with age is an important psychological problem in the elderly. If depression is not treated in old age, it produces adverse results such as early death, increased risk of suicide, decline in functioning and impairment of general health. Depression is less common in older people than in young people. However the risk of suicide is higher than in young people. In depressed elderly patients whose life expectancy and quality is falling, priority is given to care content; preventing suicide attempts, increasing self-care, and supporting and informing the elderly and family in care and treatment. A depressed elderly has a longer time to respond to treatment than younger people. However, it is worth spending time and effort to improve the quality of life by removing the old person from the mood of the depressed person.
Keywords: Elderly; Depression; Care
Introduction
With the prolongation of the average life span, the proportion of the elderly population in society increases day by day. However, as age progresses, there is an increase in the risk of physical and mental illnesses as opposed to the lifetime [1,2]. The most common psychiatric disorder in the elderly is depression. Increased incidence of depression in elderly individuals is associated with various variables such as physical illnesses, functional deficits, cognitive impairment and loss of consent [3]. In fact, the cause of depression in elderly people is not much different from that seen in young people. These include the following basic parameters: deterioration in brain chemistry (serotonin, adrenaline, reduction in secretion of dopamine), negative thinking (eg, perfectionism, self-doubt, and pessimism), some personality traits and depression due to cerebrovascular disease. Elderly patients with atrophy of the brain according to brain tomography or MR result may also be susceptible to depression [4].
It is estimated that the rate of depression among the elderly in Europe is about 10-15% [5]. Rate of depressive symptoms in individuals over the age of 75 in a comprehensive study conducted in Turkey was determined to be 16% [6]. Factors predisposition to depression in the elderly include; the death of the spouse or relatives of the elderly individual may lead to the formation of depression as it causes feelings of loneliness and isolation in the elderly individual [7,8]. Another reason for predisposition to depression is the poor physical health that can trigger a depressive episode and cause the epidemic to turn into a disease. The limitation of the movement of the person, the increase of dependence on others, the presence of pain are the most important factors. Fear of physical health, autonomy, and loss of individual competence due to negative self-awareness may set the stage for clinical depression. In addition, the presence of dynamics such as diminished social relations, economic weakness and inadequate social support are among the conditions associated with depression [9]. In old age, physical appearance, power, role and position are lost, physical- mental disabilities and diseases are increasingly addictive. Depending on these, depressive disorders can develop with feelings such as sadness, guilt, pessimism, unhappiness [10,11].
Old age causes significant, reversible disorders in high cognitive functions such as short-term memory, learning, voluntary attention, as well as general slowing down of mind processes. Sometimes depression can also be a leading symptom of dementia [12]. Depression in the elderly is associated with decreased quality of life and increased mortality [13,14]. In the future, depression is expected to take second place after heart disease [15]. The depression in elderly individuals is not much different from the type seen in adolescents. On the other hand, complaints such as sleep, appetite, concentration difficulties, slowing of walking, decreased energy and activity, and fatigue are more frequent, while signs of loss of interest (anhedonia), guilt and worthlessness in daily activities are less visible [16]. Nevertheless, it may be useful to consider some areas specific to this age group when evaluating depression in elderly individuals. Memory-related or somatic complaints may be more frequent in this age group. At the same time, comorbidity can be difficult to distinguish from symptoms of appetite, weight loss and fatigue due to physical illness. Cognitive deficits associated with elderly individuals increase the risk of dementia in the long term [17]. Depression in elderly individuals; risk of falling and social isolation may increase suicide risk [16]. It has been reported that more than 90% of elderly patients who die from suicide have depression or mental illness and the mortality rate is 5 times higher in elderly people than in the general population. In elderly male subjects, suicidal death is 4-7 times higher than in elderly women [18]. The development and symptoms of depression as a consequence of neurological disorders that are common in the elderly, such as vascular and Alzheimer's dementia and Parkinson's disease, can often be masked by cognitive deficits [19,20].
Major Depressive Disorder (MDD) is the most common psychiatric disorder in elderly patients, although the prevalence and severity of the sequelae are high, often the condition is unrecognized, untreated, or inadequately treated [21,22]. One of the reasons for this is the fact that the elderly are unhappy and stagnant is regarded as a normal pattern. Another reason is that the somatic complaints in the elderly depression are in the forefront. Old people generally do not talk about their psychological status. But they can talk about the pain of their heads or joints, their breathing shortening, their chest tightening, their tiredness when they take two steps, and their digestive system complaints. There are some special points to distinguish MDD seen in elderly people from demanstan. For example, depressive patients show temporary cognitive disturbances that respond well to treatment. While cognitive testing individuals with depression make little effort during the examination, dementia patients usually exert more effort. Individuals with depression have a significant amount of insight for intellectual difficulties, whereas insight for individuals with dementia is less. In addition, cortical or neurological symptoms observed in demented patients are not encountered in MDD [23]. Elderly individuals need valid and safe scales as well as detailed psychiatric story in order to be able to detect depression correctly and healthily.
The "Depression Scale for the Elderly" [24] is often used in the world from these scales. Screening tests can help early detection of depression in primary care and other health care settings. A multidisciplinary approach (such as a physician, nurse, psychologist, social worker) has been reported to be useful in the treatment of depression in elderly individuals. Among the general targets in treatment are the reduction or prevention of suicide risk, the increase in functioning and self-care and the prevention of recurrences [17]. According to the results of a high-evidence-based study, the mobilization of depressed patients in this age group provided substantial benefits in improving symptoms [25]. Just as in young people, pharmacotherapy (antidepressants), psychotherapy and electroconvulsive therapy (ECT) are considered to be effective in depressive disorders in elderly individuals [26]. In the care of a depressed elderly patient, priority should be given to prevention of suicide attempts, to meeting the individual needs of the individual and maximizing independent functions, providing interaction with self care, providing support to the patient and his family in care and treatment, and informing the individual and his family about treatment programs and requirements. Conclusion and Recommendations
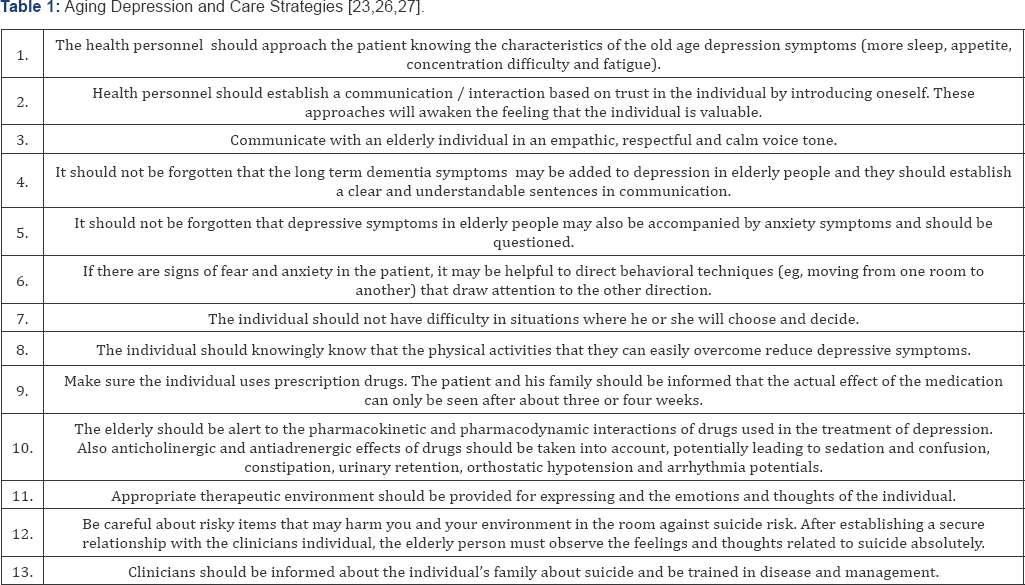
There is a significant role to play in health care staff in the prevention of depression (an increase in the number of people in the risk group, the increase of the social security possibilities of the elderly, the increase of the awareness of the family and the society), treatment and rehabilitation as an important problem in aging which is a period of increased dependency of life quality. In addition, in the majority of depressive patients, the idea is that they should not spend time on their health staff in parallel with the feeling of worthlessness [10,12,17]. For this reason, it is recommended that healthcare personnel participate in activities that will enable them to make good planning and work partitions and to ensure effective communication skills so that patients can devote time to care and treatment. We find it appropriate to give the approaches that can guide clinicians about how to approach depression seen in elderly individuals in Table 1 [27].
References
- Gitlin LN (2018) Valuation of Life as outcome and mediator of a depression intervention for older African Americans: the Get Busy Get Better Trial. International Journal of Geriatric Psychiatry 33(1): e31-e39.
- Gitlin LN (2012) A community-integrated home based depression intervention for older African Americans: descripton of the Beat the Blues randomized trial and intervention costs. BMC Geriatrics 12(1): 4.
- Lange JW (2012) The nurse's role in promoting optimal health of older adults: thriving in the wisdom years. Philadelphia: FA Davis pp. 339370.
- Wang S, DG Blazer (2015) Depression and Cognition in the Elderly Annual Review of Clinical Psychology 11(1): 331-360.
- Castro-Costa E (2007) Prevalence of depressive symptoms and syndromes in later life in ten European countries. The SHARE study 191(5): 393-401.
- Kulaksizoglu IB (2004) Unrecognized depression in community- dwelling elderly persons in Istanbul. International Psychogeriatrics 17(2): 303-312.
- Taylor WD (2014) Depression in the Elderly. New England Journal of Medicine 371(13): 1228-1236.
- Şahin D (2012) Yajlilik, depresyon ve hemŞirelik. Psikiyatri Hemjireligǧ Dergisi 3(1): 38-41.
- Sivertsen H (2015) Depression and Quality of Life in Older Persons: A Review. Dementia and Geriatric Cognitive Disorders 40(5-6): 311-339.
- Holtfreter K, D Reisig, JJ Turanovic (2017) Depression and infrequent participation in social activities among older adults: the moderating role of high-quality familial ties. Aging & Mental Health 21(4): 379388.
- Chu H (2014) The Impact of Group Music Therapy on Depression and Cognition in Elderly Persons With Dementia: A Randomized Controlled Study. Biological Research For Nursing 16(2): 209-217.
- Steffens D (2017) Late-life depression and the prodromes of dementia. JAMA Psychiatry 74(7): 673-674.
- Gallo JJ (2005) Depression, Cardiovascular Disease, Diabetes, and Two- Year Mortality Among Older, Primary-Care Patients. The American Journal of Geriatric Psychiatry 13(9): 748-755.
- Gurland B (1992) The impact of depression on quality of life of the elderly. Clinics in geriatric medicine 8(2): 377-386.
- Chapman DP, GS Perry (2008) Depression as a major component of public health for older adults. Prev Chronic Dis 5(1): A22.
- Wright PP, CW Thorpe (2016) Triple Threat Among the Elderly: Depression, Suicide Risk, and Handguns. Journal of Emergency Nursing 42(1): 14-18.
- Duman B, TE Kizil Özel (2016) Yajlilikta Depresyon ve Tedavisi. Turkiye Klinikleri J Psychiatry 9(4): 1-8.
- (2016) Centers for Disease Control and Prevention, National suicide statistics at a glance.
- Thielscher C, S Thielscher, K Kostev (2013) The risk of developing depression when suffering from neurological diseases. GMS German Medical Science 11: Doc02.
- Winter Y (2011) Depression in elderly patients with Alzheimer dementia or vascular dementia and its influence on their quality of life. Journal of Neurosciences in Rural Practice 2(1): 27-32.
- Tham A (2016) Efficacy and tolerability of antidepressants in people aged 65 years or older with major depressive disorder-A systematic review and a meta-analysis. Journal of Affective Disorders 205: 1-12.
- Richardson TM (2012) Depression and Its Correlates Among Older Adults Accessing Aging Services. The American Journal of Geriatric Psychiatry 20(4): 346-354.
- Balcio lu 1, 5 Turan (2015) Olgu Dosyalari Psikiyatri. Istanbul: Nobel Tip Kitapevleri.
- Saǧduyu A (1997) Yaşlilar ifin depresyon Ölçeǧi Hamilton depresyon Ölçeǧi ile karjilajtirmali guvenilirlik ve geÇerlilik falijmasi. Turk Psikiyatri Dergisi 8(1): 3-8.
- Bridle C (2012) Effect of exercise on depression severity in older people: systematic review and meta-analysis of randomised controlled trials. The British Journal of Psychiatry 201(3): 180-185.
- Baldwin R, R Wild (2004) Management of depression in later life. Advances in Psychiatric Treatment 10(2): 131-139.
- Çam o, E Engin (2014) Ruh Saǧliǧi ve Hastaliklari Hemjireliǧi Bakim Sanati.






























