The Etiologies behind the Scenes in Elderly Infection
Chih-Chun Huang1,2,3 and Yu-Jang Su1,3,4,5,*
1Department of Emergency Medicine, Mackay Memorial Hospital, Taiwan
2Graduate Institute of Injury Prevention and Control, Taipei Medical University, Taiwan
3Department of Medicine, Mackay Medical College, Taiwan
4Department of Oral Hygiene, College of Oral Medicine, Taipei Medical University, Taiwan
5Yuanpei University of Medical Technology, Taiwan
Submission: February 02, 2018; Published: February 06, 2018
*Corresponding author: Yu-Jang Su, Department of Emergency Medicine, Mackay, Memorial Hospital, Taipei 10449, Taiwan, Tel: 886-2-25433535, Fax: 886-2-27621403; Email: yjsu.5885@mmh.org.tw
How to cite this article: Huang CC, Su YJ. The Etiologies behind the Scenes in Elderly Infection. OAJ Gerontol & Geriatric Med. 2018; 3(2): 555609. DOI: 10.19080/OAJGGM.2017.03.555609
Keywords
Keywords: Necrotizing Fasciitis; Thigh; Cecum; Carcinoma
Abbreviations: ED: Emergency Department; WBC: White Blood Cell; CRP: C-Reactive Protein; CT: Computed tomography; AST: Aspartate Amino Transferase; BWL: Body Weight Loss; FOLFIRI: Folinic acid, Fluorouracil, and Irinotecan; ECOG: Eastern Cooperative Oncology Group
Introduction
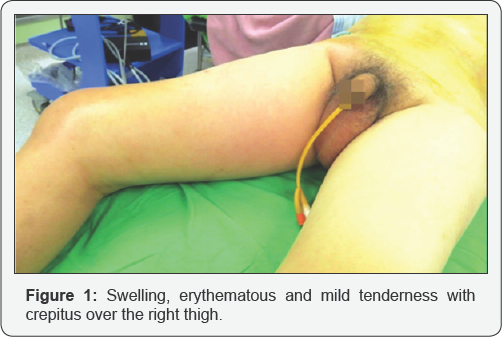
Fever with lethargy, even altered mental status is commonly seen in daily practice, especially in infected elderly. Recently we saw a 63 years old man who complaints of right thigh redness and tenderness for two days. But the etiology behind the scenes is perforated cecal tumor. Prudent workup of infectious source is mandatory to prevent from misdiagnosis. We also briefly review the literatures of necrotizing fasciitis of thigh secondary to perforated colon cancer. This old man went to our emergency department (ED) and said he also felt right back pain and difficulty in standing for one week. There was no symptom of fever, abdominal pain, nausea and vomiting, recent weight neither loss nor bowel habit change. His vital signs showed body temperature of 36°C, respiratory rate of 20 breaths per minute, pulse rate of 93 beats per minute and blood pressure of 92/54 mm Hg. Physical examination revealed swelling, erythematous and mild tenderness with crepitus over the right thigh (Figure 1).
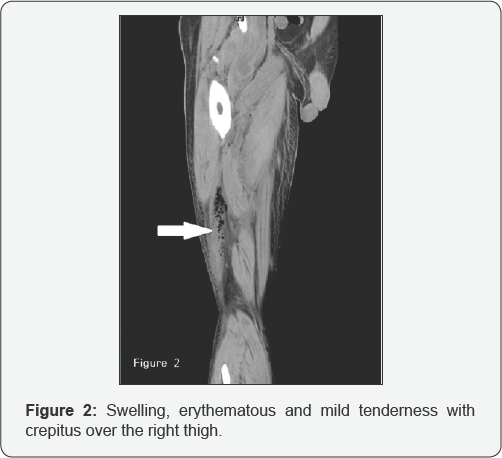
Abdomen was palpated soft with tenderness over the right lower quadrant of abdomen. Laboratory data revealed white blood cell (WBC) count of 8,400/μL, band of 8%, neutrophil of 82%, hemoglobin of 12.4g/dL, platelet count of 36,000/μL, aspartate aminotransferase (AST) of 79 U/L and C-reactive protein (CRP) of 32.25mg/dL. Computed tomography (CT) of right thigh showed scattered, abnormal air accumulation in the subcutaneous layer and muscle layer of right thigh (Figure 2). Further, abdominal contrast-enhanced CT scan showed right colon tumor with abscess formation involving right retro peritoneum and psoas muscle (Figure 3). We applied empiric antibiotic therapy with teicoplanin 200mg and meropenem 500 mg intravenously every 12 hours and fluid resuscitation. Patient received emergent laparotomy and debridement. A 5 cm x 4 cm ulcerative tumor found at cecum and perforated to retroperitoneal space.

Right hemicolectomy with side-to-side anastomosis, debridement and fasciotomy over right thigh were performed. Blood culture showed the presence of Bacteroides fragilis. Antibiotic was shifted to cefpirome 1gm every 12 hours and metronidazole 500mg every 8 hours. Abscess culture grew Bacteroides fragilis and Morganella morganii. After three weeks of admission, ventilator-associated pneumonia happened to him and sputum culture revealed Acinetobacter baumannii complex infection. We administrated tigecycline 50 mg every 12 hours for him. Pathological report of the specimen proved adenocarcinoma with one lymph node metastasis, classified as T4N1M0. After surgical intervention and drainage, he recovered from septic shock and was discharged 40 days later. Two months later, the followed chest computed tomography (CT) showed a 1cm nodular lesion with pleural dimpling at right middle lung.
Video-assisted thoracic surgery and wedge resection was performed and pathological report concluded a metastatic adenocarcinoma. Until now, post-operative 4month later, patient received adjuvant chemotherapy with FOLFIRI (Folinic acid, Fluorouracil, and Irinotecan). His ECOG (Eastern Cooperative Oncology Group) performance status is grade 0. Necrotizing fasciitis is a rare but life-threatening infectious disease needing early surgical and broad-spectrum antibiotic intervention. The etiology of necrotizing fasciitis in this case is unusual and rarely happened. Patient was healthy before and he had the symptoms with low grade fever, back pain and difficulty in standing for one week.
He denied of neither abdominal pain, bloody stool passage, body weight loss (BWL) nor bowel habit change. It is difficult to diagnose cecal tumor in the early stage, but devastating necrotizing fasciitis invaded rapidly to gluteal and thigh. Most of necrotizing fasciitis are associated with perforated colorectal cancer limited within peritoneum as Fournier's gangrene. In the English literatures review, there are only 13 reported cases of necrotizing fasciitis in thigh resulting from perforated colorectal malignancy (Table 1) [1-13]. Of them, mean age was 63.3±10.2 years old with male predominant (M:F = 5:1). The most common site of perforated colorectal cancer leading to necrotizing fasciitis is rectum (61.5%; 8/13), followed by sigmoid colon (23%; 3/13), descending colon (7.7%; 1/13) and cecum (7.7%, 1/13). Necrotizing fasciitis involving in right thigh (53.8%) is more commonly seen than left thigh (38.5%), and both thighs is 7.7%. The two-year survival rate is about 53.8%, and 46.2% of cases died 6 months later.
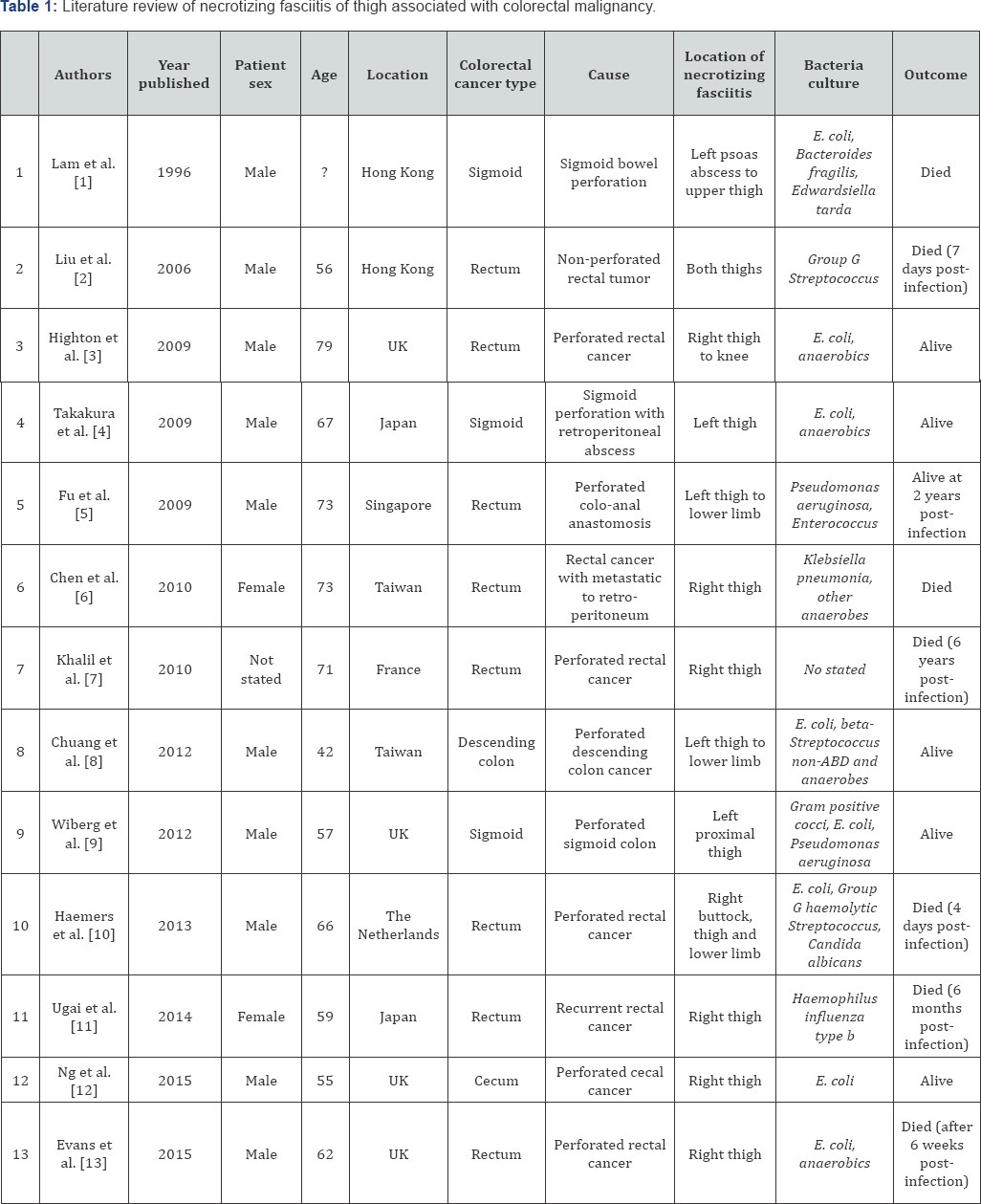
Note: List of necrotizing fasciitis secondary to perforated colon cancer cases. The most common site is rectum (8 cases), followed by sigmoid colon (3 cases), descending colon (1 case) and cecum (1 case).
Our patient is the second case worldwide of necrotizing fasciitis in thigh resulting from perforated cecum. Interestingly, sigmoid colon cancer tends to be associated with left thigh necrotizing fasciitis (100%, 3/3). In contrast, rectum cancer easily affected to right thigh necrotizing fasciitis (75%, 6/8). The most commonly seen pathogen is Escherichia coli (75%; 8/12); followed by Pseudomonas aeruginosa, Enterococcus, Bacteroides fragilis and anaerobics. The overall mortality rate was estimated to be 25% [14]. Other risk factors including old age, diabetes mellitus, hypoalbuminemia, alcohol, site of infection, delayed surgical intervention increased mortality rate [14]. In conclusion, necrotizing fasciitis of the thigh is rarely found secondary to perforated colon cancer. Delayed diagnosis and intervention of wound increase morbidity and mortality. Emergency physicians should keep in mind of the possible unusual causes and etiologies of necrotizing fasciitis, especially in infected elderly.
References
- Lam TP, Maffulli N, Chen EH (1996) Carcinomatous perforation of the sigmoid colon presenting as a thigh mass. Bull Hosp J Dis 55(2): 83-85.
- Liu SY, Ng SS, Lee JF (2006) Multi-limb necrotizing fasciitis in a patient with rectal cancer. World J Gastroenterol 12(32): 5256-5258.
- Highton L, Clover J, Critchley P (2009) Necrotising fasciitis of the thigh secondary to a perforated rectal cancer. J Plast Reconstr Aesthet Surg 62(2): e17-e19.
- Takakura Y, Ikeda S, Yoshimitsu M (2009) Retroperitoneal abscess complicated with necrotizing fasciitis of the thigh in a patient with sigmoid colon cancer. World J Surg Oncol 7: 74.
- Fu WP, Quqh HM, Eu KW (2009) Traumatic rectal perforation presenting as necrotizing fasciitis of the lower limb. Singapore Med J 50(8): e207-e273.
- Chen JH, Chang PY, Ho CL (2010) Retroperitoneal metastatic adenocarcinoma complicated with necrotizing fasciitis of the thigh in a patient with advanced rectal colon cancer. Case Rep Oncol 3(2): 304309.
- Khalil H, Tsilividis B, Schwarz L (2010) Necrotizing fasciitis of the thigh should raise suspicion of a rectal cancer. J Visc Surg 147(3): e187-e189.
- Chuang MY, Liu CK, Huang TY (2012) Case report necrotizing fasciitis of the lower limb secondary to perforated colon cancer. J Cancer Res Pract 28(1): 41-46.
- Wiberg E, Carapeti A, Greig (2012) Necrotising fasciitis of the thigh secondary to colonic perforation: The femoral canal as a route for infective spread. J Plast, Reconstr Aesthet Surg 65(12): 1731-1733.
- Haemers K, Peters R, Braak S (2013) Necrotising fasciitis of the thigh. BMJ Case Rep bcr2013009331.
- Tomotaka U, Masataro N, Takahiro M, Goh O, Makito Y (2014) Necrotizing fasciitis caused by Haemophilus Influenzae Type B in a patient with rectal cancer treated with combined bevacizumab and chemotherapy: a case report. BMC Infectious Diseases 14: 198.
- Nigel YBN, Mark T, Suzanne ET (2015) Psoas abscess and severe fasciitis due to a caecal carcinoma BMJ Case Rep.
- William DGE, Conchubhair W, Eshan A (2015) Necrotising fasciitis secondary to perforated rectal adenocarcinoma presenting as a thigh swelling. BMJ Case Rep.
- Kalaivani V, Bharati VH, Indumathi VA (2013) Necrotising soft tissue infection-risk factors for mortality. J Clin Diagn Res 7(8): 1662-1665.






























