Mind-Body Exercises for Pain Management in Older Adults
Yankai Shu1, Liye Zou*1 and Chaoyi Wang2
1College of Sports Science, Jishou University, China
2Jinlin University, China
Submission: April 19, 2017; Published: May 04, 2017
*Corresponding author: Liye Zou, College of Sports Science, Jishou University, China, Tel: 413-241-0705; Email: liyezoul23@gmail.com
How to cite this article: Yankai S, Liye Z, Chaoyi W. Mind-Body Exercises for Pain Management in Older Adults. OAJ Gerontol & Geriatric Med. 2017; 1(3): 555564.
Rationale of Mind-Body Exercise For Pain Management In Older Adults
People who are at the age of 65 or above represents 8.5 percent of the total population of 6.17 billion in the globe in 2015. According to World Health Organization [1], this age group continues to rise at an unprecedented rate and this percentage is expected to reach approximately 17 percent (1.6 billion) of the entire population worldwide by the year 2050. Musculoskeletal pain as one of the most common complaints is reported in this special population, which may be associated with chronic diseases such as osteoarthritis, rheumatoid arthritis, spinal problems, and multiple sclerosis [2,3]. More specifically, the prevalence of musculoskeletal pain is present in 50% of community-dwelling and 80% of nursing-home dwelling older adults, respectively [4,5].
The musculoskeletal pain in the ≥65 years' age group is highly associated with physical function limitations (e.g., reduced mobility, falls, and avoidance of activity), mental illness (e.g., depression, anxiety, social isolation), reduced sleep quality, and cognitive impairment. Such complications have directly contributed to reduced quality of life among older population [6,7]. Therefore, the musculoskeletal pain in this special population has become a critical public health concern.
The primary approach for chronic musculoskeletal pain management in older population typically involves pharmacological treatment (e.g., opioid and nonopioid analgesics). Additionally, non-invasive interventions have been used with modest success for alleviating pain in the older population, including acupuncture, transcutaneous electrical nerve stimulation, physiotherapy, physical therapy, and balneotherapy [8,9]. A review study by Labianca et al. [10] indicated that adverse effects (e.g., dry mouth, constipation, nausea or vomiting, pruritus, somnolence or cognitive impairment, tolerance or dependence and urinary retention) were present at people who were treated pharmacologically with these opioid and nonopioid agents. In addition, these expensive pharmacological and noninvasive treatments are unaffordable in the majority of families, especially for those in the developing countries, resulting in financial burdens [11,12]. Therefore, a relatively more cost-effective and safer approach is needed for pain management in older population.
The existing evidence indicated that participating in regular exercises or physical activities is beneficial for pain relief and enhancing functional capability in an older population with chronic musculoskeletal pain [6,8,13]. A systematic review published in the Annals of Internal Medicine suggests that people with chronic musculoskeletal pain for more than three months are recommended to participate in exercises such as motor control exercise, Taichi, and Yoga [14]. Of the exercise-based interventions, mind-body exercises have recently become more popular for pain management. When compared to conventional exercises focusing on strengthening the physical body, mind- body exercises (e.g., Pilates, Taichi, Baduanjin Qigong, and Yoga) do not only emphasize physical body movement, but also require practitioners to integrate with mental focus, breathing technique, self-awareness, musculoskeletal stretching and relaxation [15-17]. The feature of a combination of body and mind may contribute to better pain management in older adults.
Mechanisms of Mind-Body Exercises for Pain Management
A possible explanation regarding pain relief from practicing mind-body exercises in older adults may be associated with the gate control theory. According to Melzack and Wall [18], the gate control theory suggests that the passage of the uncomfortable impulses (pain) can be degraded or eliminated by any simultaneously emerging input in the A Beta nerve fiber. The painful information is typically transmitted from the peripheral receptors to the central nerve system through the dorsal horn containing C nerve fiber and A Beta nerve fiber:
I. if a person touched a sharp or hot object, pain is perceived when more C nerve fibers or only C nerve fibers are stimulated, because C fiber stimulation inactivates the inhibitory neurons so that projection neuron is not inhibited from sending pain signals to the brain;
II. the degree of pain sensation has become weaker when more A Beta nerve fibers are stimulated, because the A Beta nerve fiber stimulation activates the inhibitory neuron preventing projection neuron from sending pain signals to the brain. The Gate Control Theory is presented in Figure 1.
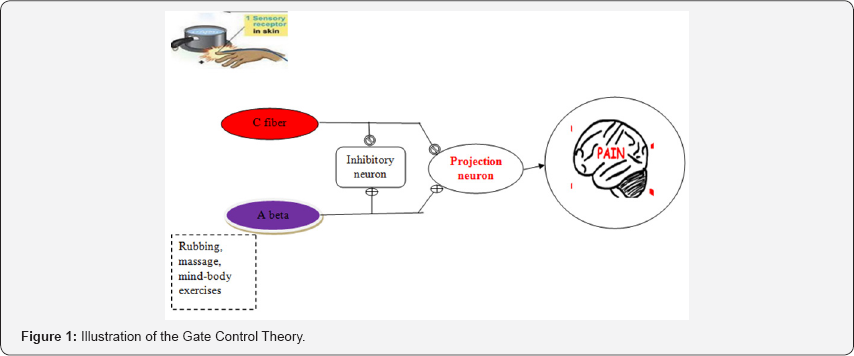
In generally, if we touched a hot stove, the discomfort or pain perception occurs in peripheral pain receptors, which then relay it to the dorsal horn of the spinal cord via C nerve fibers and subsequently travel upwards to the central nerve system so that the pain is perceived. If we rubbed or massaged the affected area, more A Beta nerve fibers are stimulated, which can weaken the degree of the uncomfortable impulses or pain sensation. Exercise itself is like rubbing or massaging, which has the same function as stimulating A beta nerve fiber [19,20]. Mind-body exercises are low-to moderate intensity exercise modes that can potentially activate the larger afferent nerve fiver, which may be reasonably beneficial for pain relief in older adults.
As mentioned previously, mind-body exercises have concentrated on integrating physical training with spiritual practice (e.g., mental focus, breathing technique, self-awareness, musculoskeletal stretching, and relaxation). The spiritual practice may also help with pain management in older population because breathing technique, mental focus, and self-awareness require practitioners to have an empty, meditative mind, instead of focusing on pain itself. For example, when you are competing in a sport, you often ignore pain produced by even severe injury. If we can get the brain think of anything else though the spiritual practice (mental focus, meditative mind, breathing technique), pain is not perceived. The relevant literature supporting the importance of cognitive factor for pain management is associated with these clinical trials investigating the effects of drug versus placebo on alleviating pain in patients with different disease conditions [21]. For example, patients who received placebo demonstrated less pain perception as compared to those in a drug group after the intervention period. From the cognitive perspective, the phenomenon is probably attributed to that patients in the placebo had the same expectation for pain relief as those in the experimental group did.
Practical implication
Mind-body exercises are complementary and alternative medicine that have become more acceptable and should be integrated with western conventional medicine in the mainstream of health care systems. In particular, the therapeutic effects of mind-body exercises for pain management in older population should be taken into account by health professionals (e.g., physical therapists, physicians, and rehabilitation specialists).
References
- Beard J, Officer A, Cassels A (2015) World report on ageing and health. Geneva: World Health Organization. Switzerland.
- Simon LS (2012) Relieving pain in America: A blueprint for transforming prevention, care, education, and research. Journal of Pain & Palliative Care Pharmacotherapy 26(2):197-198.
- Macfarlane GJ, Beasley M, Jones EA, Prescott GJ, Docking R, et al. (2012) The prevalence and management of low back pain across adulthood: results from a population-based cross-sectional study (the MUSICIAN study). Pain 153(1): 27-32.
- Gloth FM (2001) Pain management in older adults: prevention and treatment. Journal of the American Geriatrics Society 49(2): 188-199.
- Ferrel BA, Ferrel BR, Osterweil D (1990) Pain in the nursing home. Journal of the American Geriatrics Society 38(4): 409-414.
- Cavalieri TA (2005) Management of pain in older adults. The Journal of the American Osteopathic Association 105(3_suppl): 12S-17S.
- American Geriatrics Society Panel on Persistent Pain in Older Persons (2009) Pharmacological management of persistent pain in older persons. Journal of the American Geriatrics Society 57: 1331-1346.
- Cavalieri TA (2005) Management of pain in older adults. The Journal of the American Osteopathic Association 105(3_suppl): 12S-17S.
- Chatfield SM, Dharmage SC, Boers A, Martin BJ, Buchanan RR, et al. (2009) Complementary and alternative medicines in ankylosing spondylitis: a cross-sectional study. Clinical rheumatology 28(2): 213217.
- Labianca R, Sarzi-Puttini P, Zuccaro SM, Cherubino P, Vellucci R, et al. (2012) Adverse effects associated with non-opioid and opioid treatment in patients with chronic pain. Clinical drug investigation 32(suppl_1 Chronic): 53-63.
- Maniadakis N, Gray A (2000) The economic burden of back pain in the UK. Pain 84(1): 95-103.
- van Tulder MW, Koes BW, Bouter LM (1995) A cost-of-illness study of back pain in The Netherlands. Pain 62(2): 233-240.
- Ferrell BA, Josephson KR, Pollan AM, Loy S, Ferrell BR (1997) A randomized trial of walking versus physical methods for chronic pain management. Aging Clinical and Experimental Research 9(1-2): 99105.
- Qaseem A, Wilt TJ, McLean RM, Forciea MA (2017) Noninvasive Treatments for Acute, Sub acute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians Noninvasive Treatments for Acute, Sub acute, and Chronic Low Back Pain. Annals of Internal Medicine 166(7): 514-530.
- Zou, L, Wang, C (2017) Traditional Chinese Baduanjin Qigong for Older Adults: A Mini-Review 1(3): 1-2.
- Zou L, SasaKi JE, Wang H, Xiao Z, Fang Q, et al. (2017) A Systematic Review and Meta-Analysis Baduanjin Qigong for Health Benefits: Randomized Controlled Trials. Evidence-Based Complementary and Alternative Medicine.
- Zou L, Wang H, Xiao Z, Fang Q, Zhang M, et al. (2017) Tai chi for health benefits in patients with multiple sclerosis: A systematic review. PloS one 12(2): e0170212.
- Melzack R, Wall PD (1967) Pain mechanisms: a new theory. Survey of Anesthesiology 11(2): 89-90.
- Kanarek RB, Gerstein AV, Wildman RP, Mathes WF, D'Anci KE (1998) Chronic running-wheel activity decreases sensitivity to morphine- induced analgesia in male and female rats. Pharmacology Biochemistry and Behavior 61(1): 19-27.
- Bement MK (2009) Exercise-induced hypoalgesia: an evidence-based review. Mechanisms and management of pain for the physical therapist pp: 143-66.
- Benedetti F (2014) Placebo effects: From the neurobiological paradigm to translational implications. Neuron 84(3): 623-637.






























