Improving the Nutritional Status of a Patient with Pancreatic Cancer (PC)
Yu Chung Chooi1, Thomas V Fungwe2, Avis Graham2, Oyonumo E Ntekim2, Linda Thompson2, Chimene Castor2* and Dwayne Lewis3
1Dietetics Student, Department of Nutritional Sciences, College of Nursing and Allied Health, Howard University, USA
2Department of Nutritional Sciences, College of Nursing and Allied Health, USA
3Department of Radiation Therapy, College of Nursing and Allied Health, Howard University, USA
Submission: March 08, 2016; Published: April 18, 2016
*Corresponding author: Chimene Castor, EdD, CHES, MS. RD, LDN, 516 Bryant Street, NW, Washington DC 20059, USA, Tel: 202-806-5657; Email: chimene.castor@Howard.edu
How to cite this article: Yu Chung , Thomas V F, Avis G, Oyonumo E N, Linda T, et al. Improving the Nutritional Status of a Patient with Pancreatic Cancer (PC). Nutri Food Sci Int J. 2016; 1(1): 555554. DOI: 10.19080/NFSIJ.2016.01.555554
Abbreviations
PC: Pancreatic Cancer; SES: Socio-Economic Status; NCP: Nutrition Care Process; AND: Academy of Nutrition and Dietetics; RD: Registered Dietitian; ERCP: Endoscopic Retrograde Cholangio Pancreatography; EGD: Esophago Gastro Duodenoscopy
Introduction
Incidence & Mortality: Cancer is one of the major leading causes of death in US (US), second only to cardiovascular disease [1,2]. PC (PC) is the most common fatal cancer after lung, colorectal and breast cancer. It is projected to be the second leading cause of cancer death by 2030 [3]. Most PC patients will die within the first year of diagnosis [4]. Overall the mortality rates of most cancers such as lung, prostate, breast, cervix and colon/rectum have been reduced, but the mortality rate for pancreatic rates have been slowly increasing. The overall five-year survival rate of PC is only 7.2% as compared to the overall cancer survival rate of 66.5%. PC, the 12th most common cancer in the US, is the 4th most common cause of cancer-related deaths in both men and women in the US [2]. In 2015, about 48,960 new cases of PC out of the 1,6580,370 new cancer cases are expected to be diagnosed. About 77% of all cancers are diagnosed in people 55 years of age and older. Five hundred and eighty-nine thousand, four hundred and thirty Americans are expected to die from cancer in 2015, of which an estimated 40,560 cases will die from PC. From 2007 to 2011, the death rate for PC increased by 0.3% per year [1]. African Americans have higher rates of PC incidence and mortality than whites or other racial/ethnic groups [2]. PC incidence and mortality rates also are higher in men than in women. Epidemiologic studies reveal several disparities in cancer death rates by race and socio-economic status. In the years 2006-2010, it was reported that African Americans had higher cancer incidence and cancer death rates than whites or other racial/ethnic groups. People with lower socio-economic status (SES) have disproportionately higher cancer death rates than those with higher SES. This might be the result of poor diet, physical inactivity, and tobacco use for people with lower SES [1,2,5,6].
Disease & Etiology: PC is a malignant cancer in which cells form in the tissues of the pancreas. PC is predominantly a disease of the elderly. PC is rare before the age of 40, and the median age at diagnosis is 73 years. A number of risk factors for the disease have been identified apart from hereditary conditions and family history. Cigarette smoking is the most important risk factor for most of the cancer including PC [2]. There is strong evidence convincing that body fatness and abdominal fatness are causes of PC [2,7,8].
Clinical Features: Nutrition
Diets high in red meats especially in high doses and cooked at high temperatures, are suggested positive association PC [5,7,8]. Alcohol consumption appears to be small fraction of PC risk as the positive association is found in people who consume more units but not all cases [5,7]. From the review by World Cancer Research there did not appear to be sufficient evidence that intake of fruits and dietary folate, or physical activity protect against PC [5]. Epidemiological studies have shown that fruits and vegetable have inverse relationships with PC risk [7]. Today, there are no effective screening test, primary prevention and early diagnosis strategies for PC. Cancer of the pancreas usually develops without early symptoms until the cancer has already spread to other organs at an advanced stage [5]. The early symptoms are vague and non-specific and can be easily missed [9,10]. These include abdominal discomfort, bloating, flatulence, diarrhea, vomiting, constipation, epigastric, and general malaise [9]. The symptoms also depend on the location of the tumor within the pancreas and the stages [10]. Other possible symptoms include jaundice, indigestion, and bloating and oily bowel movements if the cancerous growth blocks the pancreatic duct and digestive enzymes are not released into the intestinal tract [5]. Unintended drastic weight loss and poor appetite are very common in patients with PC [11-13]. Cachexia is defined as unintended weight loss of 10% and loss of muscle & fat tissue [12-15]. PC patients who have lost weight have a poorer prognosis than patients with stable weight [16,17]. A recent study with patients suffering from PC demonstrated that weight stabilization was associated with longer survival [18]. Nutrition is a major focus for patients diagnosed with PC and subsequent treatment. Good nutrition is very important for cancer patients because the treatment alters eating patterns. Improved nutrition status and weight stabilization are very important. The objective of this case study was to investigate how the nutritional care process can be used to improve the nutritional status of a patient with PC.
Methodology
Data were collected from the patient’s medical record and electronic data file followed by interviews of the patient and registered nurse at a university teaching hospital. The data was assessed using the nutrition care process (NCP), which is a systematic approach to provide comprehensive nutritional program for patients. The NCP was established by the Academy of Nutrition and Dietetics (AND). The NCP includes four steps that must be completed by registered dietitian (RD): 1) Nutrition assessment, 2) Nutrition diagnosis; 3) Nutrition intervention, and 4) nutrition monitoring and evaluation.
Case Presentation
The patient is a 63-year old African American male with an invasive, poorly differentiated pancreatic adenocarcinoma diagnosed in June 2014. He has been receiving chemotherapy at the Cancer Center since November 2014, and was admitted to the hospital in early December 2014 due to syncope. He felt weakness in his legs and denied dizziness or lightheadedness. The patient reported that for the last two weeks, he noticed that anything he ate came right back up. At this time the patient denied nausea & vomiting, diarrhea or constipation.
Nutrition Assessment
The past medical history of the patient is adenocarcinoma of the head of the pancreas, invasive poorly differentiated cirrhosis, hepatitis B, and chronic alcoholism. The patient reported he had not drunk since his last admission on September 2014. The patient’s past surgical history included esophago gastro duodenoscopy (EGD) and endoscopic retrograde cholangio pancreatography with stent (ERCP), which were performed in Sept 2014. It used an endoscope to look into the stomach and small intestine where the ducts of the pancreas drain. X-ray dye was injected into the ducts of the pancreas and images taken of the organ, allowing irregularities of the pancreatic ducts to be identified. During the ERCP procedure, tissues were removed for a biopsy. Physical examination indicated the patient was a cachectic male who looked older than his stated age and was in no current distress. His temperature was 97.1 F, and he had a heart rate of 100, and a blood pressure 128/76. Alert oriented X3. He has had an internal jugular Port-a-Cath since October 2014. His skin was intact with no edema. His abdomen was distended, positive fluid thrill but soft with right upper quadrant tenderness to palpation with normal bowel sounds. His extremities showed positive clubbing of fingernails.
Patient’s Medications
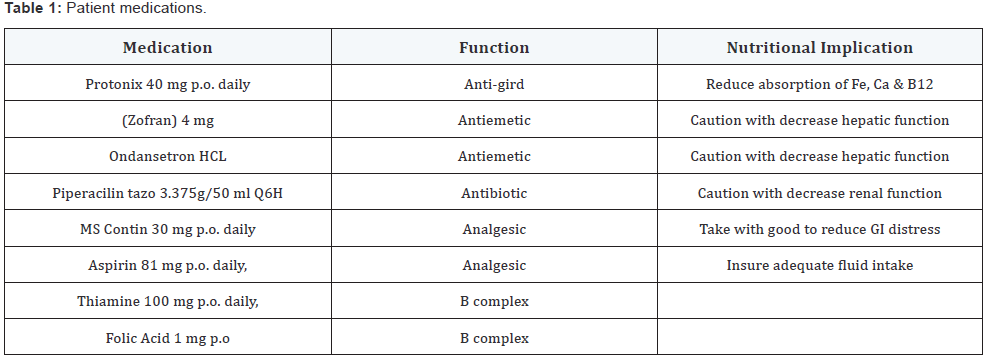
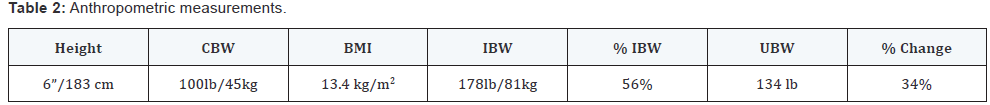
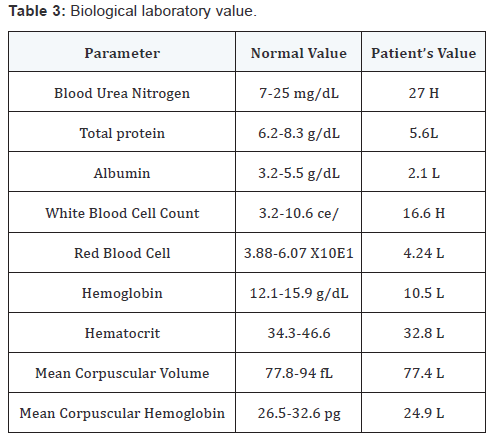
The medications being taken by the patient are shown in Table 1. The patient was unemployed, smoked two cigarettes a day, and had an extensive history of chronic alcoholism, but no drug use. He lives in an apartment with his sister who takes care of him. The patient reported a weight loss of 20-30 lb in the past 3 months. His current weight was 100 lb (BMI=13.4 kg/ m2). See Table 2 for a display comparison for patient’s weight. Patient abnormal biochemical data as per Table 3 and all other value were within normal level and were not reported. The patient has reportedly not been able to have a good oral intake for the last two weeks. He has been vomiting, also with diarrhea for the last two weeks. At this time, the patient denied nausea & vomiting, diarrhea or constipation. The patient exhibited no chewing and swallowing problems. The study found that the patient had a poor appetite with meals, consuming 25% of lunch and dinner that is inadequate to meet nutritional needs. Studies have reported that PC and its treatment can place extra demands on the body, greatly increasing nutrient and caloric needs. The patient’s energy intake requirement was 2050 kcal/day using the Mifflin St Jeor predictive equation for calculating nutritional needs. In addition, a stress-factor was added to increase meet the need of the catabolic states of cancer, hence there is a greater caloric needs. The patient’s protein needs is 81gm that was 1.8 gm/kg of body weight. The fluid intake was 1,700-2,050 ml (1ml/kg of body weight). The patient was encouraged to keep hydrated as he at risk of loss of fluid due to diarrhea.
Nutrition Diagnosis
Unintended weight loss, loss of lean body mass, poor dietary intake, and weakness are very common in a patient with PC. Moreover, the treatment of cancer involves chemotherapy, which is known to produce various acute and chronic symptoms such as loss of appetite, poor eating habits and digestion, and fatigue. Patients also experienced side effects such as nausea, vomiting, changes in taste or smell, loss of appetite, and bowel changes [11-13,19] . During the nutritional assessment in using the nutrition care process (NCP), there were two nutritional problems identified for the patient; however, two were selected as priorities - predicted suboptimal nutrient intake and unintended weight loss. Predicted suboptimal nutrient intake and unintended weight loss related to PC and effects of chemotherapy as evidenced by weight loss of 34%, BMI=13.4 kg/m2, patient reported poor appetite; and oral intake of 25%.
Nutrition Intervention:
- Provide small frequent meals with increased calories and protein
- Provide small sips of fluids to prevent dehydration
- Provide meals at least 30 minutes before the administration of medications. It is critical that patient receive nutritional education addressing timing of meals as well as the need for increased fluids to prevent dehydration.
Nutritional Recommendation: The overall goal was to improve nutritional status and stabilize weight loss. There are several nutritional recommendations to manage the loss of appetite, nausea and diarrhea and other sustaining injuries related to the diagnosis of cancer.
Nutrition Monitoring and Evaluation: The patient was under Level 1 follow-up, which was due after five days. However, the patient was discharged after three days. Therefore, no further intervention could be done. There are limitations to this paper as there is no nutrition follow-up to measure the outcome of the intervention. The patient was discharged from the hospital.
Conclusion
PC patients often have a poor prognosis and with poor nutritional status. The prognosis for a PC patient is poor with a 5-year observed survival rate of 6.7% [8]. Resection remains the only way of providing a potential cure. Unfortunately, 80% of patients will have distant metastases at the time of diagnosis [7,20]. Nutritional status influences the prognosis and quality of life of PC patients especially with significant unintended weight loss and poor appetite. Therefore, the nutrition care process plays a critical role in assisting to improve or at least prevent or delay the further decline of the patient’s nutritional status. Such an approach may ameliorate the function and quality of life of PC patients. Future research is needed to determine the impact of the nutrition care process in patients with PC.
References
- American Cancer Society. Cancer facts & figures 2015.
- National Cancer Institute (2014) A Snapshot of Pancreatic Cancer.
- Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, et al. (2014) Projecting cancer incidence and deaths to 2030: The unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res 74(11): 2913-2921.
- American cancer society. Cancer Facts & Figures 2013. Special Section: Pancreatic Cancer, pp. 25-35.
- World Cancer Research Fund & American Institute for Cancer Research, Food, Nutrition, Physical Activity, and the Prevention of Cancer: Global Prospective, 2012.
- National Cancer Institute, Pancreatic Cancer Treatment–Patient Version.
- Pericleous M, Rossi RE, Mandair D, Whyand T, Caplin ME (2014) Nutrition & Pancreatic Cancer. Anticancer Res 34(1): 9-21.
- National Cancer Institute Surveillance, Epidemiology and End Results Program (2011) SEER Stat Fact Sheets: Pancreas Cancer.
- Funel N, Del Chiaro M, Cahen DL, Laukkarinen J (2015) Pancreatic cancer. Gastroenterol Res Pract 2015: 809036.
- Hidalgo M (2010) Pancreatic Cancer. N Engl J Med 362(17):1605-1617.
- Bachmann J, Ketterer K, Marsch C, Fechtner K, Krakowski-Roosen H et al. (2009) Pancreatic Cancer related cachexia: influence on metabolism and correlation to weight loss and pulmonary function. BMC Cancer 9: 255.
- Bachmann J, Heiligensetzer M, Krakowski-Roosen H, Buchler MW, Friess H, et al. (2008) Cachexia worsens prognosis in patients with resectable Pancreatic Cancer. J Gastroinst Surg 12(7): 1193-1201.
- Ferrucci LM, Bell D, Thornton J, Black G, McCorkle R, et al. (2011) Nutritional status of patients with locally advanced pancreatic cancer: a pilot study. Support Care Cancer 19(11): 1729-1734.
- Kim SY, Wie GA, Lee WJ, Park SJ, Woo SM (2013) Changes in Dietary Intake, Body Weight, Nutritional Status & Metabolic Rate in a Pancreatic Cancer Patient. Clin Nutr Res 2(2): 154-158.
- Wigmore SJ, Plester CE, Richardson RA, Fearon KC (1997) Changes in nutritional status associated with unresectable Pancreatic Cancer, Br J Cancer 75(1): 106-109.
- Ockenga J, Pirlich M, Gastell S, Lochs H (2002) Tumour anorexiatumour cachexia in case of gastrointestinal tumours: standards and visions. Z Gastroenterol 40(11): 929-936.
- Deans C, Wigmore SJ (2005) Systemic inflammation, cachexia and prognosis in patients with cancer. Curr Opin Clin Nutr Metab Care 8(3): 265-269.
- Davidson W, Ash S, Capra S, Bauer J (2004) Weight stabilisation is associated with improved survival duration and quality of life in unresectable Pancreatic Cancer. Clin Nutr 23(2): 239-247.
- Pancreatic Cancer Guide, American Cancer Society.
- Freitas D, Fernandes Gdos S, Hoff PM, Cunha JE (2009) Medical Management of pancreatic adenocarcinoma. Pancreatology 9(3): 223- 232.







