Abstract
Bladder tumor staging and treatment is traditionally performed by transurethral resection (TURBT) with a bipolar resectoscope. Prior studies have shown that en-bloc resection of bladder tumor may offer improved hemostasis and tissue sampling.
Objectives: To compare high-power pulse modulation holmium laser en-bloc resection of bladder tumor (HoL-ERBT) outcomes to traditional bipolar TURBT.
Design and Methods: We performed retrospective review of patients who underwent HoL-ERBT using high-power pulse modulation from Jan 2020 to Aug 2023. We identified similar patients who had undergone bipolar TURBT by propensity score matching based on age, sex, BMI, and tumor size. Preoperative, intraoperative, and postoperative characteristics were compared between the two groups.
Results: We identified 14 HoL-ERBT and 14 TURBT patients for a total of 28 patients. There were no differences between the groups with regards to age, BMI, or sex. Number of tumors, tumor type, total tumor size, and tumor site did not differ significantly between the two groups. HoL-ERBT patients were more likely to have primary rather than recurrent tumors (86 vs 50%, p=0.043). Median operative time was longer in the HoL-ERBT group (70.5 vs 55.5 min, p=0.104). HoL-ERBT patients had similar rates of detrusor sampling, postoperative catheterization, foley duration and length of stay.
Conclusions: Our study demonstrates the safety and efficacy of high-power pulse modulation HoL-ERBT for bladder tumors compared to traditional bipolar TURBT. Future studies will determine if the greatest benefit is in more complex patients such as those who are chronically anticoagulated or with bleeding disorders.
Keywords:Bladder tumor; Holmium laser; Transurethral resection of bladder tumor; Moses 2.0; Urothelial carcinoma
Abbreviations: HoL-ERBT: holmium laser en-bloc resection of bladder tumor; HoLRBT: Holmium laser resection of bladder tumor; TURBT: Transurethral resection of bladder tumor; BMI: Body-mass index; CPT: Current Procedural Terminology; NMIBC: Non-muscle-invasive bladder cancer; MIBC: Muscle-invasive bladder cancer; HoLEP: Holmium laser enucleation of prostate; ASA: American Society of Anethesiologists; CBI: Continuous bladder irrigation; LGTa: Low grade Ta; HGTa: High grade Ta; HGT1 = High grade T1; HGT2: High grade T2
Introduction
Bladder cancer is a malignancy that is associated with significant morbidity and mortality. There are an estimated 82,000 new cases and 17,000 deaths in the U.S. in 2023 alone [1]. At presentation, roughly 75% of patients have non-muscle-invasive bladder cancer (NMIBC) while 25% have muscle-invasive (MIBC) or metastatic disease [2]. Determination of tumor grade as well as differentiating between non-muscle-invasive or muscle-invasive disease is critical in correctly risk stratifying and determining appropriate management options for patients. For decades, the gold standard for obtaining a tissue diagnosis for a bladder mass is transurethral resection of the bladder tumor (TURBT) with conventional bipolar resectoscope [3]. Laser technology has vastly improved and has been adapted widely in the field of urology, particularly in the management of nephrolithiasis and benign prostatic hyperplasia, where the utilization of lasers has become a primary mode of treatment. Some of the benefits to using lasers include the possibility of improved hemostasis, operative efficiency, and safety compared to conventional methods.4 Since its introduction in 1992, one of the most common contemporary lasers used is the holmium (Ho:YAG) laser, which provides rapid tissue vaporization and hemostasis [4]. Holmium laser resection of bladder tumors (HoLRBT) was described in 1998 by Das, et al as a safe and effective technique to manage bladder tumors without sacrificing diagnosis or staging [5]. In 2001, Saito described his technique for obtaining adequate pathologic specimens via enbloc transurethral resection using a holmium laser (HoL-ERBT) [6]. The majority of the studies in the literature on HoLRBT have been performed with a standard non-pulse-modulated holmium laser. Urologic lasers are typically immersed in a fluid environment and deliver energy by the creation of a cavitation bubble at the tip of the laser through which the laser pulse may travel to its target, known as the Moses Effect. In 2017, Moses™ technology (Lumenis®, now Boston Scientific) was developed to provide higher energy delivery efficiency through the cavitation bubble by pulse-modulating the laser [7]. More recently, the second-generation Moses 2.0 platform improved on the original Moses technology to allow even higher energy delivery. Studies have shown that high-power pulse modulation laser technology is associated with improved hemostasis and efficiency in prostatic enucleation [8,9]. To our knowledge, there are no comparative studies investigating the use of this technology for the treatment of bladder tumors. We sought to reflect on our experience and outcomes for patients who underwent HoL-ERBT with secondgeneration Moses™ technology compared to traditional bipolar TURBT.
Methods
Under institutional review board (IRB) approval (STU00219563), using our institution’s enterprise data warehouse, we conducted a retrospective review of all patients who had undergone HoL-ERBT at our institution from January 2020 to August 2023. As there is no singular Current Procedural Terminology (CPT) code for HoL-ERBT, we conducted our search by querying CPT codes 52224, 52234, 52235, and 52240 for resection of bladder tumor in conjunction with searching for the keyword’s “holmium” or “laser” in the surgeon’s operative note. We then manually excluded patients who were captured because they had undergone holmium laser enucleation of prostate (HoLEP) at time of their resection of bladder tumor to find our final cohort of patients who had undergone HoL-ERBT. All patients were over the age of 18 and all HoL-ERBT procedures were performed by a single surgeon using Moses™ 2.0 laser technology with a 550-micron laser at laser settings of 0.5J and 30Hz. All HoL-ERBT procedures were performed with en-bloc resection of the bladder tumor followed by bipolar resection of the tumor bed to ensure sampling of detrusor tissue. Removal of tumor tissue unable to be removed in one piece through the scope was completed with either laser resection to smaller pieces after resection or with morcellation. Morcellation was completed with a Wolf™ Piranha morcellator. Using the enterprise data warehouse, we performed propensity matching of our HoL-ERBT cohort to find a comparable control group that had undergone traditional bipolar TURBT in this time period. We propensity matched our controls based on age, sex, BMI, and bladder tumor size via CPT coding. Tumor size categorization was based on established CPT codes designated for transurethral resection of bladder tumor, including tumors less than 2cm, tumors between 2 and 5cm, and tumors greater than 5cm. We added a size category for tumors between 5 and 8cm to help better stratify the degree of large tumor burden. Propensity matching by tumor number was not completed as this was not clearly coded in the electronic medical record database.
Baseline clinical characteristics for all patients were collected and included age, sex, BMI, ASA score, and anticoagulation status. All patients had their anticoagulation held prior to their procedure and were not bridged. Baseline tumor characteristics collected included tumor nature (primary vs. recurrent), tumor number, tumor type (papillary vs. nonpapillary), tumor size, and tumor site (posterior vs. lateral vs. dome vs. trigone vs. multifocal). Intraoperative characteristics included operative time and intraoperative complications. Postoperative outcomes included need for catheterization, length of foley catheterization, presence of hematuria requiring continuous bladder irrigation (CBI), length of hospitalization, 30-day complications, and rate of recurrence on follow up. Catheterization and length of catheterization following surgery was determined by the surgeon and dependent on degree of hematuria and degree of resection. At our institution, patients typically have a follow up cystoscopy within 4-6 weeks of a high-volume primary tumor or within 3 months for secondary/recurrent tumors. Tumor outcomes included pathology, pathology grade, presence of detrusor sampling, and presence of cautery artifact. All data analyses were performed using SPSS (IBM SPSS Statistics for Windows v.29). Descriptive statistics and comparisons between groups were performed with Mann-Whitney-U and Chi-square tests for continuous and categorical variables, respectively, with p<0.05 considered statistically significant.
Results
We identified 14 patients who had undergone HoL-ERBT and propensity matched 14 patients who had undergone traditional bipolar TURBT for a total of 28 patients. Each group had 9 (64%) men and 5 (36%) women. Table 1 shows baseline characteristics for each group. The TURBT and HoL-ERBT groups were similar in both age (71.2 vs 74.2 years, p=0.329) and BMI (27.8 vs 27.1, p=0.946). There were 3 (21%) patients in the TURBT group who were on anticoagulation compared to 2 (14%) patients in the HoL-ERBT group, however this was not statistically significant (p=0.62). In the TURBT group, one patient was on apixaban, one patient on warfarin, and one patient on rivaroxaban. The HoLERBT group had two patients on apixaban. All patients had their anticoagulation held and were not bridged with any therapy. There was a statistically significant difference between the groups with regards to baseline tumor characteristics. There were 7 (50%) patients in the TURBT cohort who had primary tumors and 7 (50%) who had recurrent bladder tumors. In contrast, 12 (86%) patients in the HoL-ERBT cohort had primary tumors and only 2 (14%) were recurrent in nature (p=0.04). The type of tumors noted intra-operatively (papillary vs non-papillary) did not differ between the two groups (p=0.403). As shown in Table 1, there was also no significant difference in median number of tumors (1.0 vs 1.0, p=0.306), total tumor burden (p=0.33), or location of the tumors (p=0.13). Table 2 shows intraoperative and postoperative outcomes for the two groups. Median operative time was shorter in the TURBT cohort compared to the HoL-ERBT cohort; however, this finding did not reach statistical significance (55.5 vs 70.5 minutes, p=0.104). Rates of catheterization postoperatively were 79% in the TURBT group and 64% in the HoL-ERBT group (p=0.403). HoL-ERBT patients had similar foley duration compared to TURBT patients (2.0 vs 1.5 days, p=0.910) as well as hospital stay duration (0 vs 0 days, p=0.804). There were no significant differences in rates of hematuria requiring CBI, with 1 patient (7%) in the TURBT group and 2 patients (14%) in the HoL-ERBT group (p=0.541).
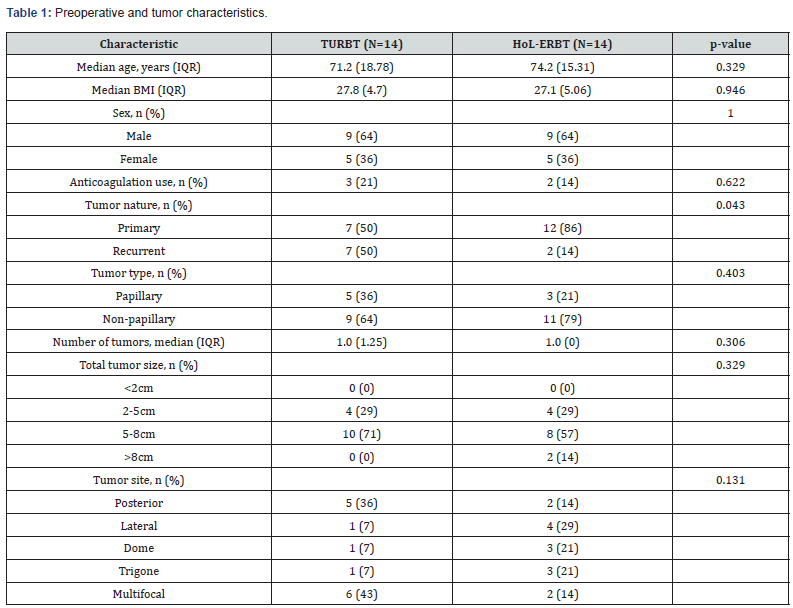
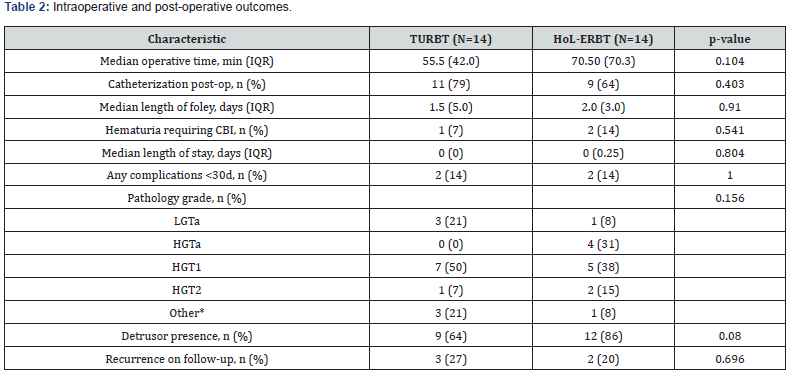
*Other includes patients diagnosed with CIS, SCC of bladder, invasive prostatic cancer, and small cell neuroendocrine tumor
The distribution of pathologic grade was overall similar between the two cohorts (p=0.16). In the TURBT group, 3 (21%) patients were found to have low grade Ta (LGTa) disease, 7 (50%) had high grade T1 (HGT1), and 1 (7%) had high grade T2 (HGT2). Carcinoma in-situ (CIS) was found in 1 (7%) patient, 1 had high grade squamous cell of the bladder, and 1 had invasive prostate cancer into the bladder. In the HoL-ERBT group, 1 (7%) had LGTa, 4 (31%) had high-grade Ta (HGTa), 5 (38%) had HGT1, and 2 had HGT2 disease. A small cell neuroendocrine tumor of the bladder was identified in 1 patient, and another patient did not have any specimen. Rates of detrusor presence trended towards higher in the HoL-ERBT cohort compared to TURBT (86 vs 64%, p=0.08). The 30-day complication rate was the same for both cohorts, with two patients (14%) in each group experiencing a complication. In the TURBT group, one patient was admitted on post-op day 3 with urinary retention requiring foley catheterization. Another patient developed a UTI requiring antibiotics. In the HoL-ERBT group, one patient presented to the emergency department on post-op day 1 with a mechanical foley issue, and the other patient experienced post-op delirium overnight on post-op day 0. Recurrence rates on follow up were similar, with a mean initial follow up duration of 3 months. Three patients in the TURBT group had tumor recurrence on initial follow up cystoscopy compared to two patients in the HoL-ERBT group (p=0.70). Of the patients who underwent TURBT, three ultimately received intravesical BCG, four received intravesical gemcitabine +/- docetaxel, one underwent cystectomy, and three underwent observation. Of the patients who underwent HoL-ERBT, six received intravesical BCG, one underwent chemoradiation, and 3 underwent observation. There were 3 patients in the TURBT cohort and 4 patients in the HoL-ERBT cohort who did not follow up after surgery.
Discussion
Although TURBT is the gold standard for management of bladder tumors, there are several risks including obturator nerve reflex, bladder perforation, bladder irritation, and postoperative bleeding. HoL-ERBT potentially offers opportunity to mitigate some of these risks and has been shown in the literature to improve time of catheterization and hospitalization. A meta-analysis by Li, et al showed that catheterization time was shorter in the HoLRBT group compared to traditional TURBT by a mean of 1.02 days. Similarly, hospitalization time was shorter by 1.11 days in their analysis [10]. Our data also shows that catheterization rates, length of catheterization, and length of stay are non-inferior for patients undergoing HoL-ERBT compared to traditional bipolar TURBT. Although prospective studies are needed, HoL-ERBT may improve surgeon comfort with leaving the patient catheterfree postoperatively and/or removing the catheter sooner potentially because of the theoretical benefit of quicker resolution of hematuria and better hemostasis intraoperatively. Patient selection is crucial when it comes to obtaining the maximal benefit over conventional TURBT. Tumor location should be considered, as it may be a more difficult to approach tumors located in the bladder dome and anterior wall with HoL-ERBT [11]. Surgeons may be more inclined to utilize HoL-ERBT for operations at higher risk for bleeding such as the anticoagulated patient or a patient with a large mass. Similarly, HoL-ERBT may offer better visualization and more efficient resection of a bulky tumor. In our study, we found that patients who underwent HoL-ERBT were more likely to have primary rather than recurrent tumors compared to patients who underwent TURBT. Two HoL-ERBT patients had very large (>8cm) tumor burdens. In our experience, patients who were chosen to undergo HoL-ERBT initially rather than traditional TURBT had large, primary tumors and were selected because accurate pathologic staging and hemostasis were prioritized. As such, one of the major limitations of this study is patient selection bias. Patients carefully selected for HoLERBT had non-inferior outcomes compared to similar patients who underwent standard TURBT. Prior comparative studies have shown no significant differences in operative times between TURBT and HoLRBT. Kramer, et al retrospectively identified 221 patients across six academic hospitals in Europe and found no differences in operative time, with a mean time of 27 minutes vs 29 minutes [12]. Similarly, a prospective study of 88 patients by Razzaghi, et al also found no difference in operative duration, with averages of 26 and 28 minutes [13]. The operatives times in our study were also not significantly different from each other but were much longer than the durations found in the literature. This is likely because our patient cohort had much larger tumors, with a median range of 5-8cm of tumor burden, compared to the prior studies which have mean tumor sizes of less than 3cm [12,13]. The authors from the aforementioned studies comment that the precise cutting line around the tumor and better vision makes HoL-ERBT preferable for resection of larger tumors [12].
The increased operative times associated with HoL-ERBT in our study may have been due to the learning curve associated with the procedure. We expect operative times to decrease as surgeons become more comfortable with the procedure. Moreover, for the HoL-ERBT patients in our study, the surgeon decided to use bipolar resection to take a deeper bite of the muscularis propria after resection of the bladder tumor to ensure adequate tissue sampling, which would add additional operative time. This may also negate some of the advantages of en-bloc laser resection such as reduced obturator reflex and risk of bleeding. None of the patients in our study across both groups experienced intraoperative complications such as obturator reflex or bladder perforation. Contrary to initial concerns that laser therapy may not provide adequate tissue for bladder cancer staging, some studies have shown that en-bloc resection may have superiority to conventional TURBT in obtaining tissue for histologic evaluation and local staging as it may allow for well-oriented 1-piece specimens that can accurately show the microanatomic relationship [10,11]. Improved staging quality may also reduce need for second TURBTs required 4-6 weeks later. In our study, there were high rates of detrusor present in specimen for both TURBT and HoL-ERBT groups. However, the surgeon in our study elected to take a deeper resection with a bipolar resectoscope after laser resection to ensure adequate muscle sampling. This prevents us from making any definitive conclusions about improvements in staging with HoL-ERBT alone compared to TURBT. For all but one patient in the HoL-ERBT group, the holmium laser was used to fragment the resected tumor into smaller pieces such that it could be evacuated through the cystoscope. For one patient with large tumor burden >8cm, a morcellator was used to morcellate the large tumor into smaller pieces for extraction and did not compromise pathologic analysis upon review with our pathologist. One patient in the HoL-ERBT group did not have any specimen sent to pathology. This patient had a large recurrent vascular tumor (inflammatory myofibroblastic tumor on prior resection) and underwent extensive tumor ablation. This patient was included in this study to show that HoL-ERBT can be a safe modality for these types of tumors.
To our knowledge, the majority, if not all, of the prior studies comparing TURBT to HoL-ERBT have been performed with a standard low-power holmium laser. In 2017, Lumenis® developed a 120W holmium laser (Moses™) that can reach up to 80 Hz. More recently, the new generation Moses 2.0 can reach as high as 120 Hz. A review of first-generation Moses and Moses 2.0 for laser lithotripsy by Corrales, et al showed that there was currently limited clinical evidence to suggest clinically relevant improvement with 2.0 over 1.0. Within the realm of lithotripsy, most studies did not find significantly different stone-free rates even comparing Moses to non-Moses technology [14]. In contrast, there are appreciable differences with regards to Moses technology and manipulation of soft tissue such as prostate. Nevo, et al performed a randomized control trial of Moses 2.0 vs non-Moses technology in patients undergoing holmium laser enucleation of prostate (HoLEP) and found that Moses 2.0 resulted in significantly shorter enucleation times (21 vs 36.7 min), higher enucleation efficiency, and shorter hemostasis time (4.1 vs 9 min).8 Nottingham et al also found quicker hemostasis time and rate for patients undergoing HoLEP with Moses 2.0.9 While HoLEP generally involves a larger surface area and amount of tissue resected compared to HoL-ERBT, it theoretically confers the same benefits of efficiency and safety. We sought to reflect on our limited experience with HoL-ERBT to add to the literature in this space. This study does have several limitations, namely its retrospective nature and small sample sizes. This study was overall underpowered to detect significant differences in postoperative outcomes such as catheterization rate and duration. As mentioned previously, there was also significant but often intentional selection biases that would influence outcomes such as operative time. Finally, in our study we had short follow up durations and limited information with regards to long-term oncologic outcomes. The distribution of NMIBC and MIBC on histologic evaluation was comparable and consistent with reported literature.2 Rates of recurrence on initial follow up cystoscopy were also comparable [15]. The three patients that had recurrence in the TURBT group all had HGT1 disease while one patient in the HoL-ERBT group had HGTa and one patient had HGT2 and underwent chemoradiotherapy.
There remain several challenges in comparing the safety and efficacy of HoL-ERBT versus TURBT. There is a lack of high-quality evidence, as much of the data currently comes from retrospective or non-randomized prospective studies. There is also heterogeneity with regards to patient and tumor characteristics when selecting patients for treatment. The main challenge is balancing the hemostasis/efficiency advantage with the oncologic benefit of the technique. HoL-ERBT has been shown to improve catheterization rates and hospital stay duration through improved hemostasis and shorter operative times. This benefit is presumably pronounced for larger, bulky tumors. However, tumors larger than 3cm cannot be extracted in one piece when resected en-bloc and require fragmentation for extraction. There is no data whether oncologic outcome is compromised for larger tumors that require fragmentation or morcellation. Notably, there is no standardized way to perform laser en-bloc resection and there are several techniques and laser systems available to surgeons [16,17]. Future studies will be needed to evaluate patients in a prospective manner to limit selection bias and allow for more accurate comparison of different en-bloc resection techniques. Long-term studies are needed to determine the oncologic benefits of HoL-ERBT.
Conclusion
Holmium laser en-bloc resection of bladder tumors (HoLERBT) is a safe and effective technique to stage and treat bladder tumors with non-inferior outcomes compared to traditional bipolar TURBT. Our study demonstrates the safety of high-power pulse modulation HoL-ERBT for bladder tumors using Moses 2.0 technology. Compared to traditional TURBT, HoL-ERBT may confer better hemostasis and may be best suited for patients with bulkier disease or those at higher risk for bleeding. Future studies will determine if the greatest benefit is in more complex patients such as those who are chronically anticoagulated or with bleeding disorders.
References
- SEER Database. American Cancer Society.
- Ashish M Kamat, Noah M Hahn, Jason A Efstathiou, Seth P Lerner, Per-Uno Malmström, et al. (2016). Bladder cancer. The Lancet 388(10061): 2796-2810.
- Chang SS, Boorjian SA, Chou R, et al. (2016) Diagnosis and Treatment of Non-Muscle Invasive Bladder Cancer: AUA/SUO Guideline. The Journal of Urology 196(4): 1021-1029.
- Thomas RW Herrmann, Evangelos N Liatsikos, Udo Nagele, Olivier Traxer, Axel S Merseburger, et al. (2012) EAU Guidelines on Laser Technologies. European Urology 61(4): 783-795.
- Das A, Gilling P, Fraundorfer M (1998) Holmium laser resection of bladder tumors (HoLRBT). Techniques in urology 4(1): 12-14.
- Seiichi Saito (2001) Transurethral En Bloc Resection of Bladder Tumors. The Journal of Urology 16(6): 2148-2150.
- Ventimiglia E, Traxer O (2019) What Is Moses Effect: A Historical Perspective. Journal of endourology 33(5): 353-357.
- Amihay Nevo, Kassem S Faraj, Scott M Cheney, Jonathan P Moore, Karen L Stern, et al. (2021) Holmium laser enucleation of the prostate using Moses 2.0 vs non-Moses: a randomised controlled trial. BJU international 127(5): 553-559.
- Charles U Nottingham, Tim Large, Deepak K Agarwal, Marcelino E Rivera, Amy E Krambeck (2021) Comparison of Newly Optimized Moses Technology vs Standard Holmium: YAG for Endoscopic Laser Enucleation of the Prostate. Journal of Endourology 35(9): 1393-1399.
- Changlong Li, Liang Gao, Jindong Zhang, Xiaokang Yang, Chuan Liu (2020) The effect of holmium laser resection versus standard transurethral resection on non-muscle-invasive bladder cancer: a systematic review and meta-analysis. Lasers in medical science 35(5): 1025-1034.
- Yaofeng Zhu, Xianzhou Jiang, Jianping Zhang, Weili Chen, Benkang Shi, et al. (2008) Safety and Efficacy of Holmium Laser Resection for Primary Nonmuscle-Invasive Bladder Cancer Versus Transurethral Electroresection: Single-Center Experience. Urology 72(3): 608-612.
- Mario W Kramer, Jens J Rassweiler, Jan Klein, Alexey Martov, Nikolay Baykov, Lukas Lusuardi, et al. (2015) En bloc resection of urothelium carcinoma of the bladder (EBRUC): a European multicenter study to compare safety, efficacy, and outcome of laser and electrical en bloc transurethral resection of bladder tumor. World Journal of Urology 33(12): 1937-1943.
- Mohammad Reza Razzaghi, Mohammad Mohsen Mazloomfard, Mahmoud Yavar, Sheida Malekian, Pouria Mousapour (2021) Holmium LASER in Comparison with Transurethral Resection of the Bladder Tumor for Non-muscle Invasive Bladder Cancer: Randomized Clinical Trial with 18-month Follow-up. Urology journal 18(4): 460-465.
- Corrales M, Sierra A, Traxer O (2022) Moses and Moses 2.0 for Laser Lithotripsy: Expectations vs. Reality. Journal of clinical medicine 11(16): 4828.
- Babjuk M, Böhle A, Burger M, Capoun O, Cohen D, et al. (2017) EAU Guidelines on Non-Muscle-invasive Urothelial Carcinoma of the Bladder: Update 2016. European urology 71(3): 447-461.
- Evangelos N Symeonidis, Ka-Lun Lo, Ka-Lun Chui, Ioannis Vakalopoulos, Petros Sountoulides (2022) En bloc resection of bladder tumors: challenges and unmet needs in 2022. Future Oncology 18(20): 2545-2558.
- Evangelos N Symeonidis, Panagiotis Baniotis, Georgios Langas, Panagiotis Stefanidis, Stavros Tsiakaras, et al (2023) En bloc resection, is this the future of non-muscle invasive bladder cancer management? Presentation of our technique and brief review of the literature. Urologia 90(1): 75-79.






























