Does Race and Ethnicity Modify the Association of Age with Severe Nocturia and Associated Bother? The Multi-Ethnic Study of Atherosclerosis
Brandon Vavra1, Ramon Durazo-Arvizu1,3, Kiang Liu3, Erin D Michos4, Linda Brubaker5, Michael P Bancks6, Talar Markossian1 and Holly Kramer1,2*
1Department of Public Health Sciences, Loyola University Chicago, Maywood, USA
2Department of Medicine, Loyola University Chicago, Maywood, USA
3Department of Preventive Medicine, Feinberg School of Medicine, Northwestern University Feinberg School of Medicine, Chicago, USA
4Division of Cardiology, Johns Hopkins University School of Medicine, Baltimore, USA
5Department of Obstetrics, Gynecology and Reproductive Sciences, University of California San Diego, USA
6Department of Epidemiology and Prevention, Wake Forest School of Medicine, Winston-Salem NC, USA
Submission:February 12, 2024;Published:February 22, 2024
*Corresponding author: Holly Kramer, Department of Public Health Sciences, Loyola University Chicago 2160 S. First Avenue Maywood, IL 60153, Email: hkramer@lumc.edu
How to cite this article: Brandon V, Ramon Durazo-A, Kiang L, Erin D M, Linda B, et al. Does Race and Ethnicity Modify the Association of Age with Severe Nocturia and Associated Bother? The Multi-Ethnic Study of Atherosclerosis. JOJ Urology & Nephrology, 2024; 8(5): 555747 DOI:10.19080/JOJUN.2024.08.555747.
Abstract
Objective: To determine whether race and ethnicity modifies the association of age with severe nocturia defined as urinating ≥ 3 times per night and associated bother.
Methods: This cross-sectional analysis utilized data from the Multi-Ethnic Study of Atherosclerosis (MESA), a cohort of four racial/ethnic groups from six U.S. communities, to collect information on urinary symptoms during the sixth exam using the International Consultation on Incontinence Questionnaire. Sex-specific logistic regression models were used to examine the association of age and race/ethnicity with severe nocturia defined as urinating ≥ 3 times at night while adjusting for demographics, co-morbidities, and medication use. Cross-product terms of age x race/ethnicity were fitted in adjusted sex specific logistic regression models to explore interactions by age and race/ethnicity on prevalence of severe nocturia.
Results: Among 3086 participants, mean age was 73.7 years, 53% were women and race/ethnicity were Non-Hispanic White (NH) in 40.0%, Chinese in 13.3%, NH Black in 25.2%, and Hispanic in 21.5%. Severe nocturia was reported by 22.8% of men and 19.9% of women and adjusted odds of severe nocturia in age group 85+ years was three-fold higher among men (Odds Ratio [OR] 2.98; 95% CI 1.58, 5.61) and two-fold higher among women (OR 2.19; 95% CI 1.22, 3.92) compared to age 55-64 years. Prevalence of severe nocturia ranged from 30.7% to 17.7% among Hispanic and NH White men, respectively, and from 30.5% to 12.6% among Hispanic and NH White women, respectively. After adjustment for covariates, no significant interaction was noted between age, race/ethnicity, and prevalence of severe nocturia (P=0.2 for men and women).
Conclusion: Severe nocturia prevalence increases with age and differs by race/ethnicity but the age-related increase in nocturia does not differ by race/ethnicity.
Keywords: Nocturia; Aging; Bother; Race/ethnicity; sleep disorders
Introduction
Nocturia is one of the most prevalent and bothersome lower urinary tract symptom [1] and is associated with sleep disturbances, lower sleep quality [2] and increased risk for falls [3] and mortality [4]. Previous studies have reported that while nocturia affects men and women similarly [5] the burden of nocturnal urination increases with advancing age [1,6]. Nocturia prevalence may also differ by race/ethnicity [7,8]. For example, the Boston Area Community Health (BACH) study reported higher prevalence of nocturia among Black and Hispanic adults compared to White adults and hypothesized that socioeconomic factors accounted for some of these differences [7]. Race/ethnicity may also influence health with aging due to structural racism which can influence access to healthcare, healthy foods, safe places for exercise and health behaviors; [9,10] such life course differences in health factors can influence nocturia prevalence with advancing age [11]. In this study we examined the association of age and race/ ethnicity with severe nocturia prevalence and associated bother using data from the Multi-Ethnic Study of Atherosclerosis (MESA), an observational cohort of adults from four different racial/ethnic groups. We specifically examined whether race/ethnicity modifies the association of age with severe nocturia and associated bother. Information on age and racial/ethnic differences of nocturia and associated bother may help elucidate unique factors associated with nocturia that may inform identification and management.
Methods
Study Design and Population
This cross-sectional study focused on men and women who completed the sixth exam of MESA, an observational study which recruited 3213 men and 3601 women, age 45 to 84 years, from six communities in the U.S. (Baltimore, MD; Chicago, IL; Forsyth County, NC; Los Angeles County, CA; Northern Manhattan, NY; and St. Paul, MN) during years 2000-2002 [12]. All participants were free of clinical cardiovascular disease and heart failure at baseline per study design. The Institutional Review Boards at all participating centers approved the study, and all participants gave informed consent. Participants were asked to participate in follow-up exams and questions on urinary symptoms were included in the sixth MESA visit conducted during July 2015 - June 2016. A total of 1749 women and 1536 men returned for the sixth MESA exam and 1635 women (93.5%), and 1451 men (94.5%) completed the questionnaire.
Exposure Assessment
Potential participants self-identified their race/ethnicity using questions based on the U.S. 2000 census questionnaire. Respondents who reported race/ethnicity as White or Caucasian, Black or African American, Chinese, or Spanish/Hispanic/Latino were asked to participate. Race/ ethnicity variables were not mutually exclusive and were categorized as non-Hispanic (NH) White, NH Black, Chinese, and Hispanic.
Outcome Assessment
The primary outcome was the presence of severe nocturia and associated bother. Information on urinary symptoms was collected using the International Consultation on Incontinence Questionnaire (ICIQ),(Abrams, Avery, Gardener, Donovan, & ICIQ Advisory, 2006; Avery et al., 2004) a reliable and validated tool which measures an individual’s experience with urinary symptoms over the past four weeks and associated bother. Prevalence and frequency of nocturia was assessed by the question, “During the night, how many times do you have to get up to urinate, on average?” For this question, respondents were queried on frequency of nocturia episodes as “none”, “one”, “two”, “three”, or “four or more”. Severe nocturia was defined as getting up at night to urinate 3 or more times because this frequency of nocturnal urination is associated with high levels of associated bother [13]. The question on nocturia was followed by a question querying associated bother and asked, “How much does this bother you?” Participants were prompted to circle a number between 0 (indicating no bother) and 10 (a great deal of bother).
Cohort Description and Covariates
We selected potential covariates based on previous studies which examined factors associated with nocturia and bladder function. Demographic characteristics, medical history, cigarette usage, general health, parity and current medication use at exam 6 along with a fasting blood sample were collected during the standardized interview. The age at the 6th follow-up exam was categorized as 55-64, 65-74, 75-84, and ≥ 85 years. Diabetes status was based on self-reported physician diagnosis of diabetes, use of insulin or oral hypoglycemic agents or a fasting glucose ≥126 mg/dl. Information on physical activity was collected using the MESA Typical Week Physical Activity Survey, which identified the duration and frequency of various physical activities during a typical week and in the past month [14]. MESA participants were contacted every 6 months after baseline visit and queried on changes in health status including new cancer diagnoses and type of cancer including prostate cancer but treatments for prostate cancer were not ascertained. Information on new cardiovascular disease (CVD) events was obtained by trained personnel who contacted the participants or family members approximately every 6 to 9 months. Self-reported diagnoses were then confirmed via review of medical records and adjudication by 2 physician members of the MESA mortality and morbidity review committee. A CVD endpoint included myocardial infarction, angina, stroke, peripheral arterial disease, or heart failure.
Statistical Analysis
Participant characteristics were examined by completion of the ICIQ. Among the MESA participants who completed the ICIQ, characteristics, including medication use, were compared by number of reported nocturia episodes after stratifying by sex. The Chi-Square test was used to compare categorical variables and an unpaired t-test was used to compare continuous variables. To address the non-parametric distribution of reported bother scores ranging from 0 to 10, 1 was added to all scores and then scores were long transformed. Log transformed scores were compared by age and race/ ethnicity in sex stratified analyses using ANOVA. A Bonferroni P-value <.01 was used as the level of statistical significance to account for multiple comparisons (3 racial/ethnic groups compared to whites). Logistic regression was used to estimate odds ratios (OR) of severe nocturia by race/ ethnicity in sex stratified models.
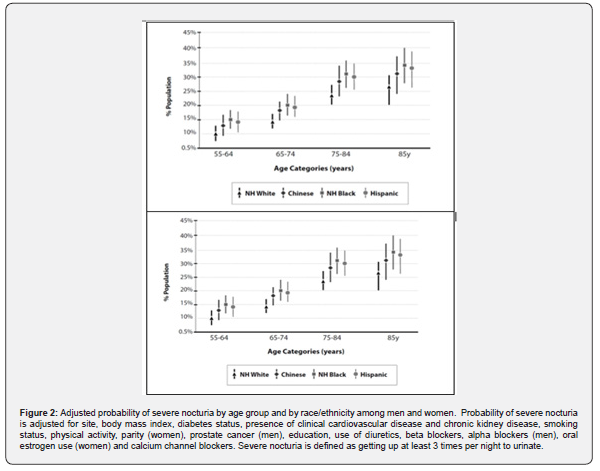
We created a set of sequentially adjusted models to examine association of severe nocturia with race/ethnicity with NH White race as referent group. Model 1 included age, race/ethnicity, and site. Model 2 added BMI, diabetes status, CVD, CKD, smoking status, parity (women), prostate cancer (men), physical activity and education to Model 1. Model 3 added use of diuretics, beta blockers, calcium channel blockers, alpha blockers (men), and oral estrogens (women) to Model 2. Parity was categorized as 0, 1, 2 and 3 live births (women) and education was categorized as less than high school, high school plus some college, and associate degree or higher. Linear trends of severe nocturia prevalence across age groups were examined by testing the linear association of the median values of the age group categories with severe nocturia after adjustment for all covariates in sex stratified models. Cross-product terms of age x race/ethnicity were fitted in fully adjusted sex specific logistic regression models to explore interactions by age and race/ethnicity on prevalence of severe nocturia. Ordinal probit regression with marginal effects was used to calculate the probability of severe nocturia frequency among men and women by race and ethnicity and by age group after adjusting for all covariates. Stata version 14 (College Station, TX) was used to perform the statistical analyses.
Results
Study Population
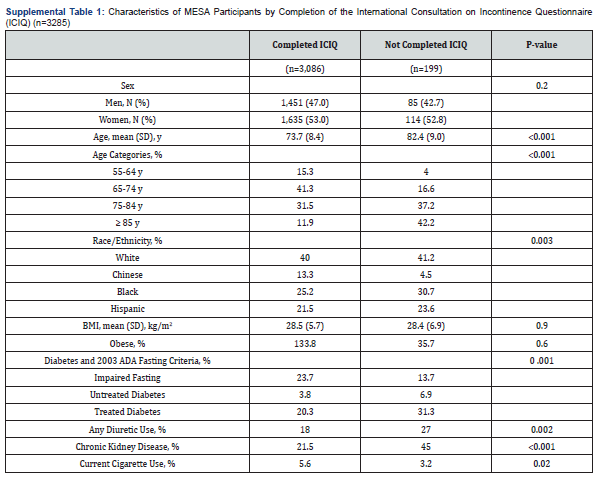
Differences of the characteristics of MESA participants by completion of ICIQ are shown in supplemental Table 1. Those who did not complete the ICIQ were older (mean age 82.4 [standard deviation [SD] 9.0] vs. 73.7 [SD 8.4] years; P <0.01) and had higher prevalence of diabetes (38.2% vs. 24.1%; P < 0.01) and greater diuretic use (27.0% vs. 18.0%; P < 0.01). Table 1 shows the characteristics of the 1451 men and 1635 women, respectively, who completed the ICIQ by frequency of nocturia episodes. Overall, mean age, BMI and prevalence of obesity, diabetes and CKD were generally higher with more nocturia episodes per night among both genders. Table 2 shows the distribution of medication use by number of nocturia episodes in men and women. Frequency of beta blocker and calcium channel blocker use differed by number of nocturia episodes and was highest in those with ≥ 3 nocturia episodes per night among both men and women. Diuretic use differed significantly by number of nocturia episodes among women only and ranged from 15.1% among women without nocturia to 31.2% among women with ≥ 3 nocturia episodes (see Table 2).
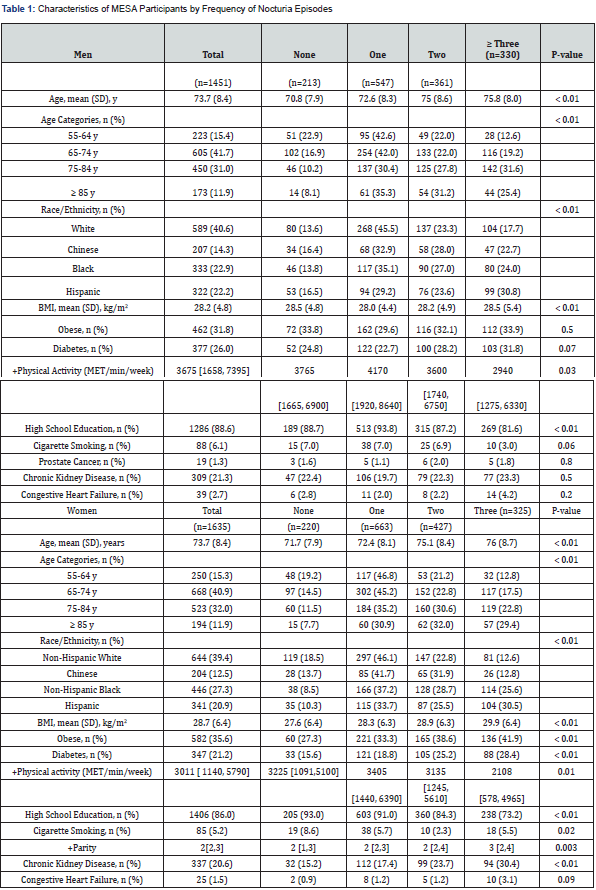
Data shown as % or mean (standard deviation) and total number of participants (percentage); + Data shown as median (interquartile range).
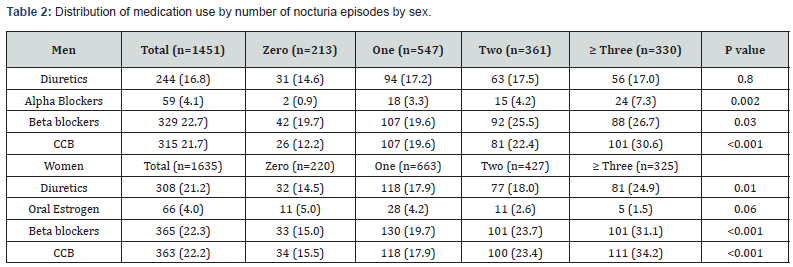
Data shown as total number participants (%) within a column.
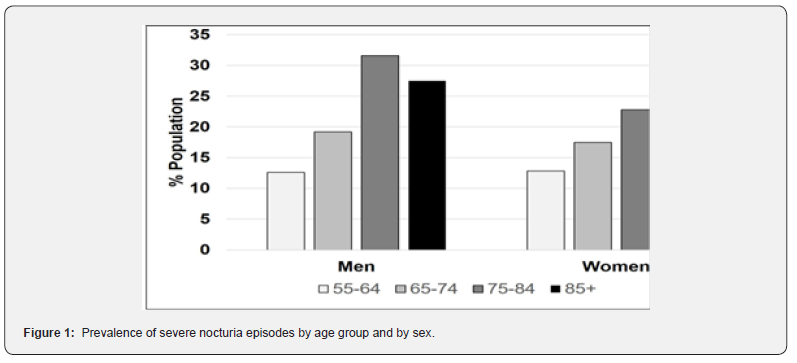
Severe nocturia was common among men and women and 22.8% of men and 19.9% of women reported > 3 nocturia episodes per night. Figure 1 depicts the bivariable analysis of severe nocturia by sex and by age group. In men, the prevalence of severe nocturia was highest among in men ≥85 years old (29.4%) and lowest among men 55-64 years old (12.6%). Severe nocturia in women was highest in the age 75-84 years (31.6%) group and lowest in the 55-64 years age group (12.6%). A significant linear trend in frequency of severe nocturia was noted across age groups for men (P < 0.001) and for women (P =0.03). In multivariable analyses with adjustment for age, co-morbidities, parity, smoking status, and physical activity, adjusted odds of severe nocturia was three-fold higher among men (OR 2.98; 95% CI 1.58, 5.61) and two-fold higher among women (OR 2.19; 95% CI 1.22, 3.92) in the age 85+ year group compared to age 55-64 ≥ years.
Race/ethnicity was also associated with severe nocturia in men and women. In bivariable analyses, severe nocturia ranged from as high as 30.7% among Hispanics to 17.7% among NH Whites among men. Among women, severe nocturia prevalence ranged from 30.5% among Hispanics to 12.6% among NH Whites. Table 3 shows the multivariable adjusted odds of severe nocturia by race/ethnicity. In both men and women, odds of severe nocturia were higher among Black and Hispanic adults compared to Whites after adjustment for age and site (Model 1). Further adjustment for demographics and co-morbidities attenuated these associations of race and ethnicity with severe nocturia (Model 2). After adjustment for all covariates including age, co-morbidities, and physical activity, only Hispanic women showed significantly higher odds of severe nocturia compared to White women while race/ ethnicity was not significantly associated with severe nocturia in men. No significant interaction was noted between age and race/ ethnicity and prevalence of severe nocturia for both men (P = 0.2) and women (P=0.2) after adjustment for all covariates. Figure 2 shows the multivariable adjusted probability of severe nocturia by age group and by race and ethnicity for both men (top panel) and women (bottom panel). Across all racial and ethnic groups, adjusted probability of severe nocturia increased with advancing age.
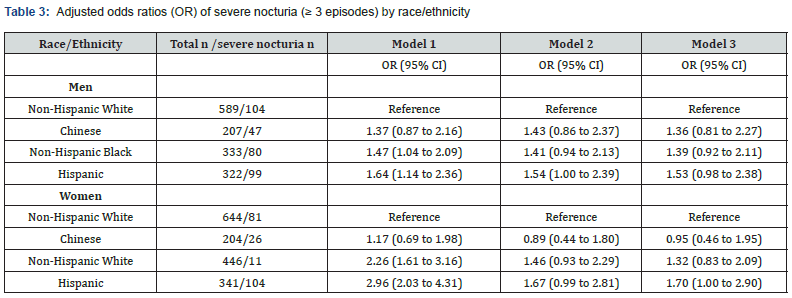
Model 1 adjusts for age and site; Model 2 adds body mass index, diabetes, clinical cardiovascular disease, chronic kidney disease, smoking status, physical activity, parity (women), prostate cancer (men) and education to Model 1; Model 3 adds use of diuretics, beta blockers, alpha blockers (men), oral estrogen use (women) and calcium channel blockers.T3
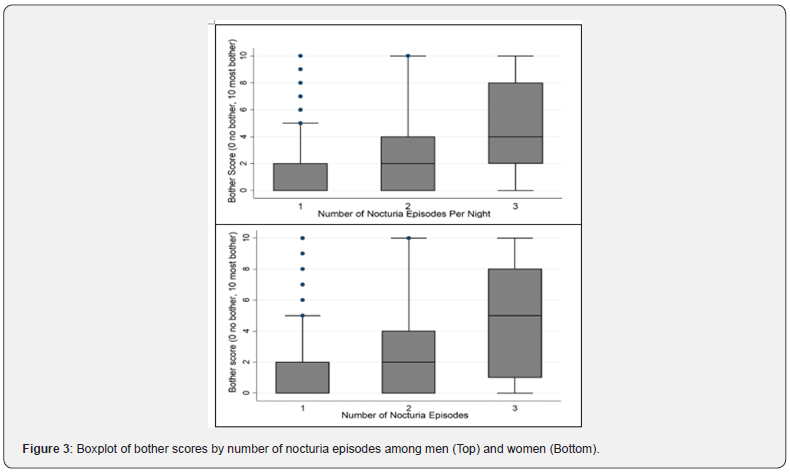
The distribution of self-reported bother scores with at least one nocturia episode is shown in Figure 3 for men (top panel) and women (bottom panel). Bother scores increased with increasing number of nocturia episodes among men and women and log-transformed bother scores differed significantly by number of nocturia episodes among men and women (P < 0.001). Bother scores among men and women with severe nocturia did not differ by race/ethnicity (ANOVA F test = 0.2 for both men and women) or by age group (F test = 0.08 for men and 0.4 for women). No significant interaction was noted between age and race/ ethnicity and log transformed bother scores for both men (P = 0.5) and women (P=0.2) with severe nocturia after adjustment for all covariates.
Discussion
In this cross-sectional analysis of older adults recruited from six communities across the U.S., prevalence of severe nocturia defined as >3 nocturia episodes per night increased with older age in both men and women. Our findings of greater prevalence of severe nocturia with increasing age are consistent with a large cross-sectional population-representative survey of nocturia among men and women from the US, United Kingdom, and Sweden [15]. A review of 43 studies reporting nocturia prevalence in community-based populations also reported that at least 60% of older people void >2 times nightly [16]. Nocturia, as a symptom, can be broadly classified based on etiology including increased fluid intake and urine production (overall or just at night), reduced bladder capacity or secondary to sleep disorders [1]. Among older adults, nocturia is often a function of increased urine production and thus intervening solely with medications for bladder dysfunction may not benefit this population with nocturia [17]. Initial interventions for nocturia in older adults should focus on lifestyle and behavior approaches [18] and lack of strong sex differences in nocturia prevalence suggest that sex-specific factors (e.g. prostate disease or parity) are not singular causes.
Our analyses also showed marked differences in severe nocturia prevalence by race/ethnicity, especially among women. Odds of severe nocturia were over two-fold higher among those Hispanic or NH Black vs. NH White women and adjustment for demographics and co-morbidities substantially attenuated the associations. Our findings further support the presence of racial/ ethnic disparities in severe nocturia among older adults, which may in part be mediated by a higher burden of metabolic related co-morbidities in some racial/ethnic groups. However, other factors that occur across the lifecourse such as occupation and behaviors may also influence the racial/ethnic disparities in severe nocturia [19,20]. Our findings of racial/ethnic disparities in severe nocturia are supported by the Boston Area Community Health Study, a survey of 5,506 adults aged 30-79(7) which reported a higher prevalence of ≥ 1 nocturia episode in Black (38.6%) and Hispanic (30.7%) vs. NH White adults (23.3%). A study of 1000 community-dwelling adults age 65 to 106 years recruited from Medicare beneficiary lists found nocturia was more common among Black than White adults [21]. Regardless of prevalence differences, the evaluation and treatment of nocturia should not differ by race/ethnicity. A retrospective study that analyzed 24-hour frequency-volume charts completed by men seeking treatment for lower urinary tract symptoms found no difference in etiology of nocturia between White and Black men for those with ≥ 1 nocturnal voids, and thus suggested that race/ ethnicity should not play a role in the evaluation of patients seeking treatment for nocturia (8) More studies are needed to discern reasons for racial/ethnic differences in nocturia because such could better identify interventions for nocturia prevention.
Our study also found that bother scores for nocturia did not differ significantly by race/ethnicity or by age group among men or women. Bother scores were higher with greater number of nocturia episodes per night, and both men and women reported very low bother scores with only one nocturia episode per night. Our findings are supported by a study performed by Tikkenen and colleagues who reported that the degree of bother and health-related quality of life correlates with the number of voids [13].
Strengths and Weaknesses
The strengths of this study include the use of a study population recruited from six U.S communities across four different racial/ethnic groups encompassing men and women. Moreover, our MESA study included Chinese participants who have been underrepresented in previous studies on racial/ethnic differences in nocturia. Urinary symptoms were ascertained using the ICIQ which has been previously validated and asks persons to recall urinary symptoms over the past four weeks and queries associated bother with urinary symptoms. This study also collected information on medication use and presence of co-morbidities including CVD. While the response rate for the ICIQ in MESA exceeded 90%, the non-response could have led to an underestimation of nocturia prevalence because the participants who did not complete the ICIQ were older with more co-morbidities compared to those who completed the ICIQ. Another limitation of this study is lack of direct measures of nocturia such as timed urine collections and the question on nocturia in the ICIQ does not specifically ask about sleep interruption.
Overall, this study shows that severe nocturia is common in both men and women and increases with advancing age regardless of race/ethnicity. Due to the high frequency of severe nocturia and the potential negative impact of severe nocturia on health outcomes, clinicians should consider screening for nocturia in older adults in all racial/ethnic groups to discuss implementation of safety measures to prevent falls and treatment.
References
- Wein AJ (2013) Re: A contemporary assessment of nocturia: definition, epidemiology, pathophysiology, and management--a systematic review and meta-analysis. J Urol 190(3): 973.
- Bliwise DL, Foley DJ, Vitiello MV, Ansari FP, Ancoli-Israel S, et al. (2009) Nocturia and disturbed sleep in the elderly. Sleep Med 10(5): 540-548.
- Pesonen JS, Vernooij RWM, Cartwright R, Aoki Y, Agarwal A, et al. (2020) The Impact of Nocturia on Falls and Fractures: A Systematic Review and Meta-Analysis. J Urol 203(4): 674-683.
- Pesonen JS, Cartwright R, Vernooij RWM, Aoki Y, Agarwal A, et al. (2020) The Impact of Nocturia on Mortality: A Systematic Review and Meta-Analysis. J Urol 203(3): 486-495.
- Schatzl G, Temml C, Schmidbauer J, Dolezal B, Haidinger G, et al. (2000) Cross-sectional study of nocturia in both sexes: analysis of a voluntary health screening project. Urology 56(1): 71-75.
- Soysal P, Cao C, Xu T, Yang L, Isik AT, Turan Kazancioglu R, et al. Trends and prevalence of nocturia among US adults, 2005-2016. Int Urol Nephrol 52(5): 805-813.
- Kupelian V, Link CL, Hall SA, McKinlay JB (2009) Are racial/ethnic disparities in the prevalence of nocturia due to socioeconomic status? Results of the BACH survey. J Urol 181(4): 1756-1763.
- Epstein MR, Monaghan TF, Khusid JA, Suss NR, Agudelo CW, et al. (2019) Comparison of nocturia etiology in black and white male patients. Can J Urol 26(3): 9769-9773.
- Rhee TG, Marottoli RA, Van Ness PH, Levy BR (2019) Impact of Perceived Racism on Healthcare Access Among Older Minority Adults. Am J Prev Med 56(4): 580-585.
- Yearby R (2018) Racial disparities in health status and access to healthcare: The continuation of inequality in the United States due to structural racism. Am J Economics and Sociology 77(3-4): 1113-1152.
- Jones NL, Gilman SE, Cheng TL, Drury SS, Hill CV, et al. (2019) Life Course Approaches to the Causes of Health Disparities. Am J Public Health 109(S1): S48-S55.
- Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, et al. (2002) Multi-Ethnic Study of Atherosclerosis: objectives and design. Am J Epidemiol 156(9):871-881.
- Tikkinen KA, Johnson TM, 2nd, Tammela TL, Sintonen H, Haukka J, et al. (2010) Nocturia frequency, bother, and quality of life: how often is too often? A population-based study in Finland. Eur Urol 57(3): 488-496.
- Bertoni AG, Whitt-Glover MC, Chung H, Le KY, Barr RG, et al. (2009) The association between physical activity and subclinical atherosclerosis: the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 169(4): 444-454.
- Madhu C, Coyne K, Hashim H, Chapple C, Milsom I, et al. (2015) Nocturia: risk factors and associated comorbidities; findings from the EpiLUTS study. Int J Clin Pract 69(12): 1508-1516.
- Bosch JL, Weiss JP (2013) The prevalence and causes of nocturia. J Urol 189(1 Suppl): S86-S92.
- Birder LA, Van Kerrebroeck PEV (2019) Pathophysiological Mechanisms of Nocturia and Nocturnal Polyuria: The Contribution of Cellular Function, the Urinary Bladder Urothelium, and Circadian Rhythm. Urology 133S: 14-23.
- Tyagi S, Chancellor MB (2023) Nocturnal polyuria and nocturia. Int Urol Nephrol 55(6): 1395-1401.
- Brady SS, Arguedas A, Huling JD, Hellemann G, Lewis CE, et al. (2024) Job strain, occupation, and bladder health among women. Neurourol Urodyn 43(1): 69-80.
- Markland A, Chu H, Epperson CN, Nodora J, Shoham D, et al. (2018) Occupation and lower urinary tract symptoms in women: A rapid review and meta-analysis from the PLUS research consortium. Neurourol Urodyn 37(8): 2881-2892.
- Burgio KL, Johnson TM, Goode PS, Markland AD, Richter HE, et al. (2010) Prevalence and correlates of nocturia in community-dwelling older adults. J Am Geriatr Soc 58(5): 861-866.






























