Malignant Mesothelioma of Tunica Vaginalis of Testis: Revisiting A Rare Entity
Sonu Sharma1*, Rajinder Yadav1, Puneet Bansal1 and Shobhna Sharma2
1Department of Urology, Fortis Hospital, Shalimar Bagh, India
2Department of Pathology, Fortis Hospital, Shalimar Bagh, India
Submission: January 31, 2024;Published: February 07, 2024
*Corresponding author: Sonu Sharma, Department of Urology, Fortis Hospital, Shalimar Bagh, India
How to cite this article: Sonu S, Rajinder Y, Puneet B, Shobhna S. Malignant Mesothelioma of Tunica Vaginalis of Testis: Revisiting A Rare Entity. JOJ 002 Urology & Nephrology, 2024; 8(4): 555745.DOI:10.19080/JOJUN.2024.08.5559745.
Abstract
Introduction: Malignant mesothelioma is a rare tumour. Tunica vaginalis as the primary site is even rarer. Approximately, 300 cases have been reported to date in the literature. Its prevalence is 0.2 per million.
Case Presentation: 67-year-old male, came with complaints of painless swelling in left hemiscrotum for 5 months. On examination, he had an enlarged left hemiscrotum. Ultrasound showed an enlarged left testis with hydrocele, with multiple deposits in tunica vaginalis with increased vascularity. Preoperative tumour markers and metastatic workup were within normal limits. He underwent a left high-inguinal orchidectomy. Microscopy showed intra-cystic papillae with a fibro-vascular core lined by stratified columnar cells with eosinophilic cytoplasm and marked atypia. IHC was positive for calretinin, WT-1, D2-40, and negative for PAX 8, CK 5/6, and vimentin. Biopsy suggestive of malignant mesothelioma of the tunica vaginalis. His follow-up PET scan was normal.
Conclusion: Malignant mesothelioma is an uncommon malignancy arising mainly from the coelomic lining of pleural and peritoneal cavities, and rarely from pericardium and tunica vaginalis. A common presentation is scrotal enlargement. Ultrasound demonstrates deposits along with features of hydrocele. Treatment is high inguinal orchiectomy in limited-stage disease. Once the disease is diagnosed the metastatic workup is done. In the case of local disease, the role of adjuvant chemotherapy and radiation is not clear. For metastatic disease, treatment remains chemotherapy as per the pleural mesothelioma treatment protocol, but the outcome remains poor. We report this rare disease which should be considered a differential diagnosis in case of hydrocele and testicular tumours.
Keywords: Mesothelioma; Tunica vaginalis; Testis; Malignant; Rare
Abbreviations: IHC: Immunohistochemistry; WT-1: Wilms Tumour; D2-40: Mouse monoclonal antibody specific for human podoplanin; PAX 8: Marker for mesothelial lesion; CK 5/6: Cytokeratin; PET: Positron Emission Tomography; MMTVT: Malignant Mesothelioma of the Tunica Vaginalis Testis; MRI: Magnetic Resonance Imaging; US: Ultrasonography; CEA: Carcinoembryonic Antigen; EMA: Epithelial Membrane Antigen; UK: United Kingdom
Introduction
Malignant mesothelioma of the tunica vaginalis testis (MMTVT) is an extremely rare tumour, usually mimicking benign pathologies of the scrotum [1]. Most cases are reported between 55 and 75 years of age, while 10% of the cases are seen in patients younger than the age of 25 [2]. Due to its rare nature, its epidemiology and risk factors are still not well established. However, asbestosis, which is a well-known risk factor for mesothelioma, is only reported in 30%-40% of such cases [3].
Case Presentation
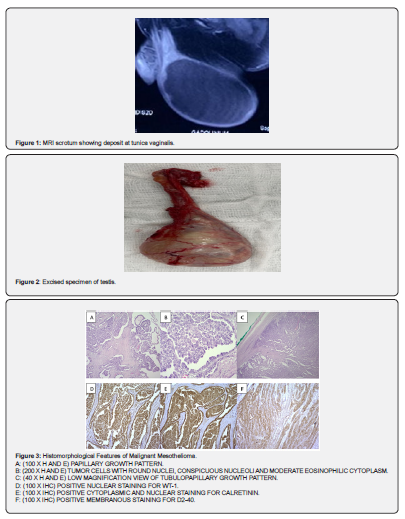
A 67-year-old male came with complaints of painless swelling in the left hemiscrotum for 5 months. On examination, he had an enlarged left hemiscrotum with a hard-solid mass giving suspicion of a tumor along with fluid in the scrotal sac Ultrasound showed an enlarged left testis with hydrocele, with multiple deposits in tunica vaginalis with increased vascularity. Serum tumour markers and metastatic workup were within normal limits. MRI scrotum (Figure 1) revealed moderate hydrocele with a deposit in tunica vaginalis. He underwent a left high inguinal orchidectomy (Figure 2). Microscopy showed intra-cystic papillae with a fibro-vascular core lined by stratified columnar cells with eosinophilic cytoplasm and marked atypia. IHC was positive for calretinin, WT-1, D2-40, and negative for PAX 8, CK 5/6, and vimentin (Figure 3). Biopsy is suggestive of malignant mesothelioma of the tunica vaginalis. His follow-up positron emission tomography (PET) scan was normal.
Conclusion
Malignant mesothelioma of tunica vaginalis of testis (also known as para testicular mesothelioma), is a rare tumour, comprising less than 1% of all mesotheliomas [4,5]. Meanwhile the first case was recorded in 1957 and since then only case reports and case series have been published, with less than 300 patients worldwide to date [6,7]. Malignant mesotheliomas are thought to develop from the coelomic epithelium at the pleura, peritoneum, pericardium and tunica vaginalis testis. Mesothelioma of the tunica vaginalis testis represents only 0.3–5% of all mesothelial neoplasms [8]. Risk factors include trauma, herniorrhaphy, long-term hydrocele or spermatocele, long-term epididymitis, orchitis or other inguinal inflammation [4]. The mechanism by which chronic serosal inflammation contributes to the development of mesotheliomas is not known, although it has been proposed that they may be mediated via the continuous production of interleukin-6 [9]. The rarity of testicular mesothelioma poses challenges to its diagnosis and that is seldom achieved preoperatively. The main symptoms are nonspecific, and patients usually present with enlargement of the scrotum, recurrent hydrocele and palpable scrotal mass [2]. Common differential diagnoses include epididymitis, scrotal or inguinal hernia and spermatocele [3]. Ultrasonography (US) is a non-invasive, simple and 90% accurate method used to detect testicular tumours [10].
In typical cases, tunica vaginalis mesotheliomas resemble their pleural and peritoneal counterparts [11]. Pure epithelioid and biphasic histologic subtypes comprise 60-75% and 20-40% of all testicular mesotheliomas respectively also few cases of pure sarcomatoid differentiation have been identified [12,13].
The tumour usually shows papillary, tubulopapillary or well-differentiated solid growth with or without spindle cell proliferation [11,13]. A large immunohistochemical profile by Winstanley et al facilitated the association of specific factors to disease of the tunica vaginalis as an alternative to extrapolating data from thoracic studies. The authors studied 18 cases from the UK between 1959 and 2004. They found that all cases were positive for calretinin and EMA, 16 (89%) were positive for thrombomodulin, 15 (83%) were positive for CK7, 13 (72%) were positive for CK5-CK6, and all cases were negative for CK20 and carcinoembryonic antigen (CEA) [14]. IHC was positive for calretinin, WT-1, D2-40, and negative for PAX 8, CK 5/6, and vimentin in our study.
Principles of management are frequently inferred from that of pleural or peritoneal mesotheliomas which may be a combination of surgery, radiation therapy and chemotherapy [15]. Pemetrexed with cisplatin, which has proven efficacy in pleural mesothelioma, is most often used in cases with unfavorable prognosis [16,17]. Gemcitabine is a valid option for patients, who do not respond well to platinum-based chemotherapy drugs [18]. Higher tumour stage (tumour, greater or equal to four centimeters, nodal involvement and metastasis) and biphasic histologic subtype are associated with significantly worse outcomes of testicular mesotheliomas [12]. Our patient did not receive radiotherapy because he was surgically treated at an early stage and showed no sign of metastasis. We present a case of a patient with testicular mesothelioma of tunica vaginalis. The rarity of testicular mesothelioma poses challenges to its aetiology research, diagnosis and treatment. Diagnosis of testicular mesotheliomas is challenging, as the tumour lacks specific clinical and radiologic features. Despite aggressive surgical procedures or extra testicular mesothelioma-based adjuvant therapies, the prognosis remains poor.
References
- Menut P, Hervé JM, Barbagelata M, Botto H (1996) Bilateral malignant mesothelioma of the tunica vaginalis testis. Apropos of a case [Article in French]. Prog Urol 6(4): 587-589.
- Plas E, Riedl CR, Pflüger H (1998) Malignant mesothelioma of the tunica vaginalis testis: review of the literature and assessment of prognostic parameters. Cancer 83(12): 2437-2446.
- Bisceglia M, Dor DB, Carosi I, Vairo M, Pasquinelli G (2010) Paratesticular mesothelioma. Report of a case with comprehensive review of literature. Adv Anat Pathol 17(1): 53-70.
- Mezei G, Chang ET, Mowat FS, Moolgavkar SH (2017) Epidemiology of mesothelioma of the pericardium and tunica vaginalis testis. Ann Epidemiol 27(5): 348-359.
- Marinaccio A, Binazzi A, Di Marzio D, Scarselli A, Verardo M, et al. (2010) Incidence of extrapleural malignant mesothelioma and asbestos exposure, from the Italian national register. Occup Environ Med 67(11): 760-765.
- Zhang N, Fu N, Peng S, Luo X (2017) Malignant mesothelioma of the tunica vaginalis testis: a case report and literature review. Mol Clin Oncol 7(6): 1053-1056.
- Chen J-L, Hsu Y-H (2009) Malignant mesothelioma of the tunica vaginalis testis: a case report and literature review. Kaohsiung J Med Sci 25(2): 77-81.
- Trenti E, Palermo SM, D’Elia C, Comploj E, Pycha A, et al. (2018) Malignant mesothelioma of tunica vaginalis testis: report of a very rare case with review of the literature. Arch Ital Urol Androl Organo Uff Soc Ital Ecogr Urol E Nefrol 90(3): 212-214.
- Dostert C, Pétrilli V, Van Bruggen R, Steele C, Mossman BT, et al. (2008) Innate immune activation through Nalp3 inflammasome sensing of asbestos and silica. Sci 320(5876): 674-6777.
- Blaivas M, Brannam L (2004) Testicular ultrasound. Emerg Med Clin North Am 22(3): 723-748.
- Amin MB (2005) Selected other problematic testicular and paratesticular lesions: rete testis neoplasms and pseudotumors, mesothelial lesions and secondary tumors. Mod Pathol Off J U S Can Acad Pathol Inc 18(Suppl 2): S131-S145.
- Nazemi A, Nassiri N, Pearce S, Daneshmand S (2019) Testicular mesothelioma: an analysis of epidemiology, patient outcomes, and prognostic factors. Urology 126: 140-144.
- Chekol SS, Sun CC (2012) Malignant mesothelioma of the tunica vaginalis testis: diagnostic studies and differential diagnosis. Arch Pathol Lab Med 136(1):113-117.
- Winstanley AM, Landon G, Berney D, Minhas S, Fisher, et al. (2006) The immunohistochemical profile of malignant mesotheliomas of tunica vaginalis: a study of 20 cases. Am J Surg Pathol 30(1): 1-6.
- Yan TD, Welch L, Black D, Sugarbaker PH (2007) A systematic review on the efficacy of cytoreductive surgery combined with perioperative intraperitoneal chemotherapy for diffuse malignancy peritoneal mesothelioma. Ann Oncol Off J Eur Soc Med Oncol 18(5): 827-834.
- Recabal P, Rosenzweig B, Bazzi WM, Carver BS, Sheinfeld J (2017) Malignant mesothelioma of the tunica Vaginalis testis: outcomes following surgical management beyond radical orchiectomy. Urology 107: 166-170.
- Vogelzang NJ, Rusthoven JJ, Symanowski J, Denham C, Kaukel E, et al. (2003) Phase III study of pemetrexed in combination with cisplatin versus cisplatin alone in patients with malignant pleural mesothelioma. J Clin Oncol Off J Am Soc Clin Oncol 21(14): 2636-2644.
- Favaretto AG, Aversa SML, Paccagnella A, Manzini VDP, Palmisano V, et al. (2003) Gemcitabine Combined with Carboplatin in Patients with Malignant Pleural Mesothelioma: A Multicentric Phase II Study. Cancer 97(11): 2791-2797.






























