Profile and Prognostic Factors of Acute Postpartum Renal Failure in a Rural Center in Sub-Saharan Africa: Experience of the City of Touba in Senegal (West Africa)
Ndiaye Babacar1*, Kane Yaya2, Dieng Ameth3, Ndongo Modou4, SY Abou4, BA Mamadou Aw2, Niang Samba1, Banza Augustin T1, Faye Moustapha4, Faye Maria4, Lemrabott A Tall4 and Ka Eh Fary4
1Department of Nephrology and Hemodialysis, Matlaboul Fawzaini Hospital, Senegal, West Africa
2Department of Nephrology and hemodialysis, Peace Hospital/Assane Seck Ziguinchor University, Senegal, West Africa
3Department of Nephrology hemodialysis, CHR of Thiès / University of Thiès, Senegal, West Africa
4Department of HALD nephrology hemodialysis, /UCAD Dakar, Senegal, West Africa
Submission:December 04, 2023;Published:December 18, 2023
*Corresponding author: NDIAYE Babacar, Department of Nephrology and Hemodialysis, Matlaboul Fawzaini Hospital, Senegal, West Africa, Email id: baymbay89@gmail.com
How to cite this article: Ndiaye B, Kane Y, Dieng A, Ndongo M, SY Abou, et al. Profile and Prognostic Factors of Acute Postpartum Renal Failure in a Rural Center in Sub-Saharan Africa: Experience of the City of Touba in Senegal (West Africa). JOJ Urology & Nephrology, 2023; 8(4): 555741 DOI:10.19080/JOJUN.2023.08.555741.
Abstract
Introduction: The prevalence of acute postpartum renal failure (APP-RF) remains high in Senegal and is burdened with high mortality. Our study aimed to determine the profile of APP-RF and to evaluate the maternal prognosis.
Patients and Method: This was a retrospective descriptive and analytical study carried out in two departments: the nephrology-hemodialysis department and the gynecology department of the Matlaboul Fawzaini Hospital of Touba over two years (1 January 2020 to 31 December 2021). The patients received during this period and whose presented an APP-RF were included.
Results: The hospital prevalence of APP-RF was 2.52%. The average age of our patients was 29 ± 6.84 years. High blood pressure was present in 49.49% of patients at admission, disturbed consciousness in 9.09% of them, and oligo-anuria in 17.17% of them. The acute renal failure (ARF) occurred in a haemorrhagic context in 54.54% of patients and in context of pre-eclampsia in 31.31% of cases. Fourteen-point fourteen percent of patients (14.14%) received haemodialysis. Recovery of renal function was complete in 61.61% of cases and partial in 10.10%. Other complications were noted in 22 patients and were dominated by haemorrhagic shock and respiratory distress syndrome. Death occurred in 27 patients. The poor prognostic factors found were delay in nephrological treatment, dyspnoea, fever, oligo-anuria, severity of renal failure, depth of anaemia and use of furosemide.
Conclusion: In Africa and particularly in Senegal, we must implement all human and technical means to counter this scourge. This requires good prevention, improving the standard of living of populations and rigorous monitoring of pregnancies.
Keywords: Acute Renal Failure; Postpartum; Senegal; Thrombocytopenia; Metabolic Acidosis
Introduction
Acute postpartum renal failure (APP-RF) is defined by its occurrence in the period from delivery to three months [1]. It generally shares the same aetiologies as ARF in the third trimester of pregnancy [2]. Its prevalence has drastically decreased over the last twenty years in developed countries. In developing countries, however, the frequency has not decreased much, and pregnancy is still responsible for 15-20% of ARF [3]: 16% in South Africa and 19% in Morocco [4,5]. It is burdened with high maternal-foetal morbidity and mortality [3]. Among the causes of maternal mortality, APP-RF remains poorly understood. In this context, this study was carried out to determine the epidemiological, etiological, therapeutic, evolutive, and prognostic profiles of APP-RF.
Patients and Method
This was a retrospective descriptive and analytical study carried out in two departments: the nephrology-hemodialysis department and the gynecology department of the Matlaboul Fawzaini National Hospital of Touba from 1 January 2020 to 31 December 2021. Patients received during that period and whose presented APP-RF were included. Patients with pre-existing renal failure at the time of conception were excluded. We defined APP-RF as any sudden alteration of renal function occurring within one day to three months after delivery with a creatinine level above 13mg/l and normal-sized kidneys on renal ultrasound, with good cortico-medullary differentiation. For each patient included, we collected epidemiological parameters (age, area of residence, and time to nephrology treatment), medical and gynaeco-obstetrical history, clinical and biological parameters, and therapeutic data. The evolutive modalities were noted for each included patient. The cure was declared when the creatinine level at discharge returned to normal (less than 13 mg/l). The evolution was unfavourable in the following situations:
• Partial recovery, which was defined as resumption of diuresis, improvement in renal function without normalization of creatinine levels, and non-dependence on dialysis.
• Complication(s) related to APP-RF.
• Progression to end-stage renal disease, which is defined as failure to normalize renal function and permanent dependence on dialysis.
• Death.
To identify poor prognostic factors, two groups were considered: the first consisting of patients with a favourable evolution and the second with an unfavourable evolution. The data collected were entered using Excel 2019 and analyzed using R 4.1.2. Qualitative variables were presented as percentages and quantitative variables were presented as average plus or minus standard deviation or with a minimum and a maximum. The analytical study was done with cross-tabulations. To compare frequencies, the KHI 2 test or Fisher’s test was used. The difference was statistically significant for “p” < 0.05.
Results
During the study period, 3922 postpartum patients were hospitalized, 99 of them presented ARF and represented a hospital prevalence of 2.52%. The average age of our patients was 29 ± 6.84 years. The 25-35years age group was the most represented with 48 patients (48.48%). Thirteen patients had a medical history, with 10 hypertensive patients, including 6 chronic and 4 gravid hypertensives, 2 diabetic patients and one patient with heart disease. Fourteen patients (14.14%) lived in urban areas and 35 in rural areas (35.35%). The average time to the nephrology department from the day of delivery was 6±5.5 days. The average gravidity was 4 units [1-11]. The average parity was 4 pares [0- 10 pares] with a predominance of multiparas (75.75%). Thirty-three (33.33%) patients had a good pregnancy follow-up with at least 3 prenatal consultations and the pregnancy was monofetal in 92 patients (92.93%), twin in 5 patients (5.05%). Fifty-eight patients (58.59%) had full-term pregnancies while 41 patients had premature deliveries (41.41%). Delivery was by vaginal route in 32 patients (32.32%) and by caesarean section in 67 patients (67.68%).
Functional signs were dominated by abdominal pain in 14 patients (14.14%) and dyspnoea in 12 patients (12.12%) (Table I). In general signs, the conjunctival mucous membranes were pale in 65 patients (65.66%). Hypertension was present in 49 patients (49.49%) on admission (Table 2). Nine patients (9.09%) had impaired consciousness (ranging from obnubilation to coma) on admission and 17 patients had oligo-anuria (17.17%). Cardiovascular collapse was present in 3 patients (3.03%) (Table 3). The average blood urea was 0.62 ± 0.50 g/l and the average creatinine was 26.06 ±20.19 mg/l. The blood ionogram was measured in 17 patients. Six patients had hyponatremia on admission (35.3%), and hyperkalaemia was noted in 2 patients (11.77%). Anaemia was found in 80 patients (80.8%) with an average haemoglobin level of 8,54 ± 2,90 g/dl. Fifty-three patients had thrombocytopenia (53.53%). ARF occurred in the context of haemorrhage in 54 patients (54.54%) including 45 cases (45.45%) of retro-placental haematoma (RPH), 9 cases (9.09%) of post-partum haemorrhage (PPH) and in the context of pre-eclampsia in 31 patients (31.31%).



On the therapeutic level, hygienic and dietary measures (water restriction in case of oligo-anuria; low sodium diet in case of sodium inflation and low potassium diet) were instituted in all our patients. Furosemide was used in 13 patients (13.13%), and antihypertensive drugs were used in 49 patients (49.49%) with calcium channel blockers being the most used. Seventy-three patients (73.73%) had received a blood transfusion. Fourteen patients (14.14%) received haemodialysis. Three patients underwent haemostasis hysterectomy. The evolution was favourable, towards recovery in 61 patients (61.61%) with resumption of diuresis and a return to normal renal function. The average time to complete recovery was 6 days [range: 2- 20 days]. An unfavourable evolution was noted in 38 (38.38%). Partial recovery was noted in 10 patients (10.10%). Progression to chronic dialysis was noted in 1 patient (1.01%).
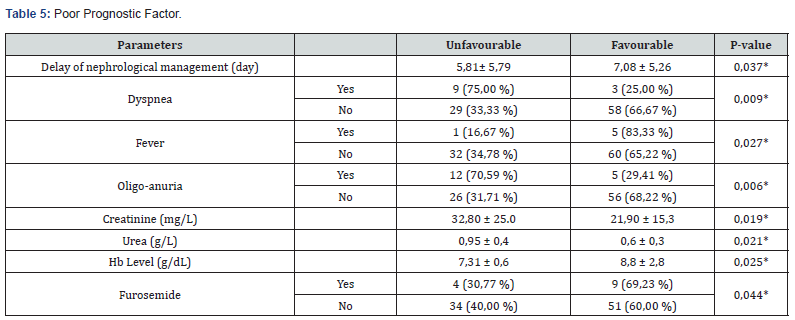
Other complications were noted in 22 patients and dominated by haemorrhagic shock (14.14%) and respiratory distress syndrome (4.04%) (see Table 4). Death was noted in 27 patients (27.27%). The causes of death were dominated by haemorrhagic shock and septic shock (Figure 1). The poor prognostic factors found were delay in nephrological treatment, dyspnoea, fever, oligo-anuria, severity of renal failure, depth of anaemia and the use of furosemide (Table 5).

Discussion
Prevalence of APP-RF varies according to the series and causes. During the study period, the hospital prevalence was 2.52%. This result corroborates white that reported by Miguil in Morocco which was 2.49% [5] and was lower compared to that reported by Lemrabott in Senegal and Fatimetou in Mauritania which were respectively 4.65% and 6.09% [6,7]. This result shows that efforts have been made to improve the monitoring of pregnancies in our various structures, particularly in rural areas. Most authors agree that the severity of ARI can be explained by the delay in treatment [8,9]. The setting time was significantly longer in patients who did not recover compared to patients who recovered their renal function. This delay was respectively 7.08±5.26 and 5.81±5.79 days (p=0.037). The delay in treatment was quite longer (6 days on average) compared to that found in the Kâ study (4 days on average) and like that found by Lemrabott (6 days on average) [10,11]. The average age of our patients was 29 years. This average age is comparable to that found in most African countries [4-7]. This average age corresponds to that of women of childbearing age. Clinically, 17 patients (17.17%) were oligo-anuric on admission. This rate is much lower than those reported by Lemrabott and Hmima with 82.2% and 64.51% respectively (6,12). Patients with preserved diuresis evolved much more favourably than those with oligo-anuria. (p =0.006). Twenty-seven patients (27.27%) had lower limb oedema. In the Lemrabott study, these oedemas represented 61% [6]. They are part of the pre-eclamptic syndrome or constitute a hydrosodic overload inherent to oligo-anuric PP-ARF [1]. High blood pressure was found in 49.49% of patients. Hmima and Fatimetou, in their series, found 70.76% and 68.62% respectively [7,12].

In our study, blood urea was on average 0.62 ± 0.50 g/l and its level was negatively correlated with the evolution of ARF (p=0.021). Blood urea constitutes a seriousness criterion from certain values, a rate greater than 3g/l is correlated with uremic encephalopathy, constituting an indication for emergency extra-renal therapy [13]. The average creatinine level was 26.06 ± 20.19 mg/l on admission. The severity of the renal damage was negatively correlated to the renal prognosis (p=0.019). The average creatinine level was significantly lower than that reported in several African studies [6,7]. This rise in average creatinine in our study could be explained by the delay in taking charge of the patients, as well as their low socioeconomic level. Indeed, most of our patients were seen by the nephrologist at day 6 postpartum. Usually normal in ARF, the low haemoglobin level in PP-ARF is due to several mechanisms: haemorrhagic delivery, and mechanical haemolysis in the context of HELLP syndrome or thrombotic microangiopathy [2]. In addition, deficiency anaemia, which is common in our region, is often associated with the mechanisms mentioned above. Anaemia was found in 80 patients (80.8%) with an average haemoglobin level of 8.54 g/dl. The depth of the anaemia seems to have an impact on the renal prognosis (p=0.025). Indeed, deep anaemia may maintain renal failure, the most frequent cause of which is acute tubular necrosis. Most studies, particularly in Africa, list pre-eclampsia as the main cause of PP-ARF [14-16]. Severe pre-eclampsia was noted in 31.31% of patients. In Morocco, Miguil noted a rate of 67.2% of pre-eclampsia [5]. Haemorrhagic causes were noted in 54.54% of patients, including 45.45% of HRP and 9.09% of PPH. In the HMIMA study in Senegal, haemorrhagic causes were noted in 29.03% of patients [12]. Therapeutically, furosemide was used in 13 patients (13.13%) and its use was negatively correlated with the evolution of PP-ARF (p=0.044) Furosemide, although widely used to stimulate diuresis to overcome the oliguria of ARF, does not allow for a faster recovery of renal function nor does it reduce maternal mortality and recourse to haemodialysis [17]. Its use can even be dangerous by inducing forced diuresis, which can lead to renal hypo-perfusion because of hypovolaemia [18]. Antihypertensive drugs were used in 49.49% of our patients. This result is like those found by Kabbali in Morocco with 45% of use [6,19]. This treatment improves renal function in APP-RF, especially if this high blood pressure is malignant. Haemodialysis was performed in 14 patients (14.14%) in our series. In APP-RF, recourse to extrarenal purification may be indispensable in certain situations: anuria, acute pulmonary oedema, hyper-uraemia, hyperkalaemia, and metabolic acidosis.
In our study, the evolution was favourable in 61 patients (61.61%) with resumption of diuresis and normal renal function. The cure rate in our series was like those reported in previous studies in Senegal. Indeed, Bennani found a cure rate of 60% [20] while Lemrabott published an even lower rate of 45.9% [6]. Unfavourable evolution was noted in 38 patients (38.38%). Recovery was partial in 10 patients (10.10%). Lemrabott and Bennani found a higher rate with respectively 24% and 40% of partial recovery [6,20]. Complications were noted in 22 patients (22.22%) and dominated by haemorrhagic shock in 14 patients (14.14%). The mortality rate was 27.27% and the causes of death were dominated by haemorrhagic shock. This rate is close to those found in other studies in Senegal with Hmima (22.58%), Lemrabott (23.2%) and Bennani (30%) [6,12,20]. This could be explained by the persistence of a long delay in diagnosis and inadequate initial treatment.
Conclusion
Acute postpartum renal failure has become rare in industrialised countries but remains common in developing countries. This affection poorly documented in our context constitutes an important and non-negligible cause of maternal morbidity and mortality. In Africa, and particularly Senegal, must implement all human and technical means to counter this scourge This requires good prevention, improving the standard of living of populations and rigorous monitoring of pregnancies.
References
- Moulin B, Hertig A, Rondeau E (2010) Rein et préé Ann Fr Anesth Reanim 29(4): e83-90.
- Belenfant X, Pallot J-L, Reziz K, Saint Léger S (2004) Insuffisance rénale aiguë et grossesse. EMC-Néphrologie 1: 44-54.
- Ricci Z, Ronco C, D’amico G, De Felice R, Rossi S, Bolgan I, et al. (2006) Practice patterns in the management of acute renal failure in the critically ill patient: an international survey. Nephrol Dial Transpl 21(3): 690-696.
- Randeree IGH, Czarnocki A, Moodley J, Seedat YK, Naiker IP (1995) Acute renal failure in pregnancy in South Africa. Ren Fail 17(2): 147-153.
- Miguil M, Salmi S, Moussaid I, Benyounes R (2011) Insuffisance rénale aiguë hémodialysée en obstétrique. Néphrol Ther 7(3): 178-181.
- Lemrabott AT, Cissé MM, Faye M, Seck SM, Niang A, et al. (2019) Insuffisance rénale aiguë du post-partum au Sénégal: Profils épidémiologique, étiologique, thérapeutique, pronostique et é Rev Afr Malg de Reche Scien 1.
- Abdelkader F, Saleh AM (2020) Insuffisance rénale aigue du post partum : à propos de 102 cas au centre hospitalier National de Nouakchott, Mauritanie. PAMJ-Clin Med 4(48).
- Aya AGM, Mangin R, Laloucey l (1996) Prééclampsie sévè principales modalités de la prise en charge avant transfert. J Gynecol Biol Reprod 25: 196-205.
- Sibai BM, Ramadan MK, Usta I, Salama M, Mercer BM, et al. (1993) Maternal morbidity and mortality in 442 pregnancies with hemolysis, elevated liver enzymes, and low platelets (HELLP syndrome). Am J Obstet Gyn 169(4): 1000-1006.
- Ka EHF, Cissé MM, Faye M, Fall K, Niang A, Diouf B (2012) Contribution à l’étude de l’insuffisance rénale aiguë du postpartum (à propos de 146 cas colligés à Dakar). Néphrol Thér 5: 362.
- Lemrabott AT, Mah SM, Faye M, Saleck M, Cissé MM, Fall K, et al. (2017) Insuffisance rénale aiguë du post-partum en Mauritanie: prévalence, étiologies et facteurs pronostiques. Néphrol Ther 13(5): 365.
- Leye PA, Bennani M, Fall ML, Bah MD, Beye DM, et al. (2014) Insuffisance rénale aiguë du post-partum en réanimation au CHU de Dakar. Rev Afr Anesth Med Urg.
- Khellaf G, Arzour H, Gaoua H, Lebid S, Samrani R, et al. (2011) L’insuffisance rénale aiguë du post-partum. Néphrol Thér 7(5): 335.
- Drakeley AJ, Le Roux PA, Anthony J, Penny J (2002) Acute renal failure complicating severe preeclampsia requiring admission to an obstetric intensive care unit. Amer J Obs Gyn 186(2): 253‑25
- Miguil M, Chekairi A (2008) Eclampsia, study of 342 cases. Hypertens Pregnancy 27(2): 103‑1
- Mjahed K, Alaoui SY, Barrou L (2004) Acute renal failure during eclampsia: incidence risks factors and outcome in intensive care unit. Ren Fail 26(3) :215-2
- Trabold F, Tazarourte K (2010) Prise en charge pré-et interhospitalière des formes graves de préé Ann Fr Anesth Reanim p. e69-73
- Moonen M, Fraipont V, Radermacher L, Masset C, Firre E, (2010) Acute kidney injury: from concept to practice. Néphrol Ther 7(3): 172-177.
- Kabbali N,Tachfouti N, Arrayhani M,Harandou M,Tagnaouti M, et al. (2011) Insuffisance rénale aiguë et grossesse : résultats d’une étude prospective nationale au Maroc. Néphrol Thér 5: 274.
- Leye PA, Bennani M, Fall ML, Bah MD, Beye DM, Diouf E (2014) Insuffisance rénale aiguë du post-partum en réanimation au CHU de Dakar. Rev Afr Anesth Med Urg.






























