COVID-19 among Hospitalized Chronic Hemodialysis Patients: Clinical Features and Predictors of Mortality
Dahlan, Randah A1*, Faqihi, Ahmed Y2, Alsulami, Hajar A2 and Alkatheeri, Ali M1
1Department of Internal Medicine, Section of Nephrology, King Abdullah Medical City, Makkah, Saudi Arabia
2Department of Internal Medicine, King Abdullah Medical City, Makkah, Saudi Arabia
Submission:June 05, 2023;Published: June 20, 2023
*Corresponding author: Randah Dahlan, Department of Internal Medicine, Section of nephrology Al Mashair, Saudi Arabia
How to cite this article: Dahlan Randah A, Faqihi, Ahmed Y, Alsulami Hajar A, Alkatheeri Ali M. COVID-19 among Hospitalized Chronic Hemodialysis Patients: Clinical Features and Predictors of Mortality. JOJ Urology & Nephrology, 2023; 8(1): 555731. DOI: 10.19080/JOJUN.2023.08.555731
Abstract
Objectives: Chronic hemodialysis patients have an increased susceptibility to COVID-19 infection, and worse outcomes compared to the general population. This study aims to describe the clinical course and outcomes of hemodialysis patients with COVID-19 infection, and to describe predictors of mortality.
Methods: This retrospective observational study included adult chronic hemodialysis patients hospitalized to a tertiary care center with COVID-19 infection between January 1, 2020 and December 31, 2022. Data about their clinical features at time of diagnosis, and rate of complications were collected.
Results: 49 hemodialysis patients were hospitalized with COVID-19. The mortality rate was 26.5%, 45% required ICU admission, 28% required mechanical ventilation, 12% developed VTE, and the average length of hospitalization was 17 ± 15 days. When comparing survivals with non-survivals, age, initial level of C-reactive protein, LDH, haemoglobin, and initial abnormal chest X-ray were predictors of mortality.
Conclusion: This study confirms the high mortality rate observed among hemodialysis patients with COVID-19, and it suggests some clinical variables as predictors of mortality. We discuss the possibility of a geographical pattern of excess complications of COVID-19 among dialysis patients in the western region of Saudi Arabia compared to other regions, and we call for a higher prioritization to the western region for all supportive and preventative measures, especially the holy cities of Makkah and Medina. We believe this prioritization will have a positive impact on controlling COVID-19 infection nationally and internationally, because of the yearly mass gathering of all Muslims from all over the world in these two cities.
Keywords: COVID-19; Coronavirus; SARS-CoV-2; Hemodialysis; Chronic dialysis; End-stage renal disease.
Abbreviations: ICU: intensive care unit; LDH, lactate dehydrogenase; VTE: venous thromboembolic events.
Introduction
Coronavirus disease 2019 (COVID-19) is an illness that is caused by a novel coronavirus called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1]. Patients with end-stage renal disease (ESRD) who are on maintenance hemodialysis are at increased risk of acquiring COVID-19, and having worse outcomes compared to the general population [2–6]. This could be due to the high burden of comorbidities, altered immune system, and/or frequent visits to healthcare facilities with subsequent contact with patients and healthcare workers [6,7]. Despite having worse outcomes, their presenting clinical symptoms could be milder than those of the general population, and this might be explained by their weak immune system [8]. Several studies have been published to describe the clinical features of COVID-19 and risk factors for severe illness in chronic hemodialysis patients. These factors may differ from those observed in the general population. For example, D-dimer level is not a good predictor of mortality in hemodialysis patients with COVID-19 infection, however, it may be associated with outcomes when the general population develops COVID-19 [8]. Other predictors, like dialysis vintage, level of serum lactate dehydrogenase (LDH), lymphocytes count, and level of c-reactive proteins (CRP) have been associated with outcomes in hemodialysis patients [8]. Understanding of COVID-19 is still evolving, and not all the study results are generalizable, illustrated by the variation in the incidence and the mortality rates from country to country [9]. In fact, some data suggests that the rate of mortality from COVID-19 infection among dialysis patients is affected by geographical and temporal patterns observed within the same country [10]. Data about the clinical features and outcomes of hemodialysis patients with COVID-19 in Saudi Arabia are limited [11-13]. Identifying and understanding risk rates and factors are important when planning and implementing interventions, such as the COVID-19 vaccination. This study aims to describe the clinical course and the outcomes of hospitalized ESRD patients who tested positive for COVID-19 from January 1, 2020 till December 31, 2022. We also aim to describe risk factors that could affect mortality.
Materials and Methods
This retrospective study included patients older than 18 years who had ESRD and were on chronic hemodialysis before presentation. All included patients were admitted to a single tertiary care hospital in Makkah, Saudi Arabia, (King Abdullah Medical City (KAMC), Makkah) from January 1, 2020, until December 31, 2022, and tested positive for COVID-19 at the time of/or during admission. Multiple admissions for one patient during the same month were counted as one admission.
This study received the approval of the Institutional Review Board (IRB) of KAMC, with IRB number 22-992. Eligible patients were identified by an independent electronic retrospective chart review conducted by two different authors. The following data were collected: patient’s age, gender, nationality, body mass index (BMI), duration on hemodialysis in years, history of diabetes (DM), Hypertension, ischemic heart disease (IHD), cerebrovascular accidents (CVA), history of chronic lung disease, Charlson Score (calculated), vaccination status, symptoms and vital signs at the time of testing (fever, cough, shortness of breath, gastrointestinal symptoms, fatigue, loss of smell or taste, respiratory rate, oxygen saturation, systolic blood pressure, and diastolic blood pressure), laboratory results at the time of COVID-19 testing (white cell counts (WBC), lymphocytes count, hemoglobin level, platelets, CRP, erythrocytes sedimentation rate (ESR), procalcitonin, LDH, Brainnatriuretic peptide (BNP), troponin, ferritin, and D- dimer), Chest X-ray (CXR) findings at the time of testing (normal CXR, unilateral infiltrate, bilateral infiltrate). Additionally, data on management strategies during hospitalization (requirement of continuous renal replacement therapy (CRRT), and use of antibiotics, antiviral, steroids, and biological agents), and complications and outcomes (venous thromboembolic (VTE) events, length of hospital stay, requirement of admission to the intensive care unit (ICU), requirement of mechanical ventilation, and death) were collected. COVID-19 was confirmed positive by detecting SARSCoV- 2 RNA using reverse transcription-polymerase chain reaction (RT-PCR) on a nasopharyngeal sample taken by a trained nurse. All samples were sent to a regional lab for testing.
Discrete variables were reported using counts and percentages, while continuous variables were reported using means and standard deviations. Comparative analysis was conducted between both mortality outcomes (non- survivals vs. survivals) using the T-test for continuous variables, and Fisher’s exact test for categorical variables. The significant p-value is less than 0.05.
Results
During the study period, forty-nine chronic hemodialysis patients were hospitalized, and all were diagnosed with COVID-19 infection during their hospitalization. Their main demographic, clinical characteristics, and main lines of management are summarized in Table 1. The average age of included patients was 57 ± 11.6 years, their average years on dialysis was 4.16 ± 2.7 years, and most of them (92%) were tested for COVID-19 because of suspicious symptoms, while the remaining (8%) were tested either pre-procedural or because of history of contact with a suspected patient. Most patients (92%) received no vaccination prior before their current infection or hospitalization. Of note, 22 of the total positive cases (45%) were in the year 2020, and 11 cases (22%) in 2021, the remaining 16 (33%) cases were in 2022. Out of the 49 patients, 13 patients died leading to a mortality rate of 26.5%, 22 patients (45%) required ICU admission, 14 patients (28%) required mechanical ventilation, and 6 patients (12%) developed venous thromboembolic disease. The average length of hospitalization was 17 ± 15 days. Of note, 70% of the mortalities occurred in the years 2021 and 2022.
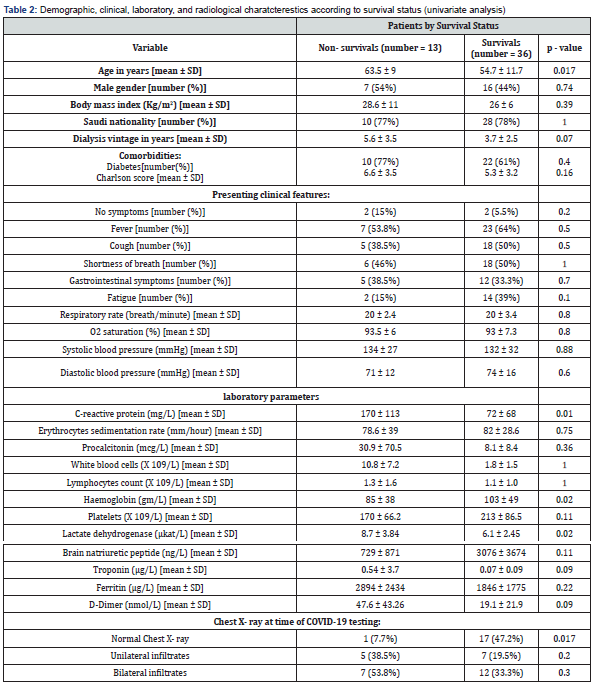
When comparing survivals with non-survivals (Table 2), nonsurvivals were older (63.5 ± 9 vs. 54.7± 11.7, p = 0.017), had a higher initial CRP level (170 ± 113 vs. 72 ± 68 mg/dl, p = 0.008), a lower initial hemoglobin level (85 ± 38 vs. 103 ± 49, p = 0.02), a higher initial LDH level (8.7 ± 3.84 vs. 6.1 ± 2.45, p = 0.02), and more likely to have had an abnormal chest X-ray at the time of COVID-19 testing. Additionally, non-survivals were more likely to have had a longer dialysis vintage (5.6 ± 3.5 vs. 3.7 ± 2.5, p = 0.07), and a higher initial troponin level (0.54 ± 3.7 vs. 0.07 ± 0.09, p = 0.09), but the difference was not statistically significant (Table 2). When looking at different lines of management, non-survivals were more likely to have required CRRT (92.3% vs.16.6%, p = 0.0001), to have received steroids (92.3% vs. 33.3%, p = 0.0003), to have received antibiotics (100% vs. 80.5%, p= 0.05), to have required ICU admission (92.3% vs. 27.7%, p = 0.001), and to have required mechanical ventilation (100% vs. 2.7%, p = 0.0001). There was no difference between non- survivals and survivals concerning receiving antiviral therapy (46% vs. 47% respectively, p = 1.0), or tocilizumab (23% vs. 16.6% respectively, p = 0.68) of note; there was no difference between non-survivals and survivals concerning the VTE events (15% vs.11%, respectively, p = 0.6).
Discussion
The Center for Disease Control and Prevention (CDC) has adopted the recommendations of the Advisory Committee on Immunization Practices (ACIP) for the allocation of the COVID-19 vaccine [14]. These recommendations suggest giving certain groups of people a priority for receiving the COVID-19 vaccine according to certain risk factors and classifying people into two groups (Group 1 and Group 2) [14]. Group 1 is further classified into Group 1a (which includes healthcare personnel and longterm care facility residents), Group 1b (which includes frontline essential workers, persons aged ≥ 75 years), Group 1c (which includes persons aged 65–74 years, persons aged 16-64 years with high-risk medical conditions, and essential workers not recommended for vaccination in group 1b). Group 2 includes all people over the age of 16 who have not been recommended for vaccination in Group 1. The highest priority is given to group 1a and the priority then goes in descending order. Hemodialysis patients currently fall into group 1c because of their highrisk medical condition. However, the International Society of Nephrology has urgently called for a higher prioritization of dialysis patients worldwide and moving them up to group 1a [15]. This “Call to Action” is justified by the following: [15]. The fact is that patients receiving in-center hemodialysis are required to go to their dialysis centers three times a week, during which they may come in close contact with other patients as well as health care providers. This makes them no different from residents of long-term care facilities, which are currently classified as group 1a.
The great impact of vaccinating hemodialysis patients on protecting other patients, dialysis staff, and patients’ families. This is especially true with the easy accessibility to dialysis patients and hence the delivery of vaccination, which could be given during their hemodialysis sessions.
To minimize the indirect effect of the COVID-19 pandemic on hemodialysis patients which comes from patients fear and anxiety of contracting the infection during hemodialysis, leading to their decision (or sometimes the dialysis unit decision during the surge of infection) of reducing their dialysis sessions from 3 to 2 with subsequent potential impact on their clinical condition and the health care system.
Above all, dialysis patients are at a higher risk of acquiring COVID-19 compared to the general population [2-6,15], and once infected, they are 30% to 130% more likely to die than hospitalized patients with COVID-19 but no chronic kidney disease with case fatality rates varying from 16% to 32% [15]. These increased risks are higher than the risk of the other groups (i.e., patients with other comorbidities like diabetes, obesity, etc.) currently classified as 1c [15].
A systematic scoping review of the COVID-19 data on chronic HD patients indicates the poor prognosis among hospitalized patients, with up to 70.5% requiring ICU admission with their mortality rate reaching up to 100% [16]. Are these rates and results generalizable? The answer is likely no, supported by the variation in the reported mortality rate of COVID-19 among hemodialysis patients from country to country [17]. Even within the same country, the mortality rate may differ, as exampled by the geographic and temporal patterns of excess mortality observed among HD patients dialyzing in different facilities in the United States when comparing their observed and predicted monthly number of deaths [10]. Understanding this variation is important when implementing different preventative strategies, like vaccination, as well as when managing and prioritizing the allocation of resources. Therefore, each country (and maybe each region within a country) may need to study their patients’ risks as well as various factors affecting their outcomes, especially with the evolving knowledge about COVID-19 and its episodes of outbreaks. Data about COVID-19 among chronic HD patients in Saudi Arabia are limited [11-13]. Table 3 summarizes the currently available data about the outcomes of COVID-19 among chronic dialysis patients in Saudi Arabia. Although all studies were single centers and included a small number of patients, each study attempted to address the mortality rate and predictors of outcomes of COVID-19 among dialysis patients (mostly hemodialysis) within a different region in Saudi Arabia. Tawhari et al. looked at ESRD patients who developed COVID-19 in the central and found an overall mortality rate of 18% [11]. However, the mortality rate was higher (up to 23%) among patients who were symptomatic at the time of admission, and predictors of mortality were the need for inotropes, age, and CRP level on admission [11]. Of note, in this study all patients were admitted as part of the center routine practice with ESRD patients who tested positive for COVID-19 regardless of the severity of symptoms. In another study from the southwest region of Saudi Arabia, Hakami et al. reported a mortality rate of 19.8% among chronic HD patients with COVID-19 and found that age, heart disease, lymphocytopenia, neutrophilia, D-Dimer, ferritin, blood urea nitrogen, and aspartate transaminase level were the predictors of mortality [12]. Alkhunaizi et al looked at ESRD patients who developed COVID-19 in the eastern region and found an overall mortality rate of 17%, which increased to 30% among those who developed pneumonia [13]. In this study, half of the patients had mild symptoms, and the remaining half developed pneumonia. Age, diabetes and coronary artery disease were predictors of the development of pneumonia [13]. In our current study, an overall mortality rate of 26.5% (27.6% among symptomatic patients) was observed. We found that age, CRP level, anemia, LDH level, and abnormal initial chest X-ray were predictors for mortality. When having a general look at these four studies, there are no geographical or temporal patterns of excess mortality among chronic HD patients in Saudi Arabia. However, there is a tendency toward a higher rate of all complications observed in our current study. Nevertheless, it is hard to make a solid conclusion if we take into consideration the small sample size of all four studies, differences in the characteristics of the included patients (e.g. severity of symptoms), and the potential effect of some difference in the timeliness between our study and other conducted studies which may have coincided with different waves of COVID-19 and/ or different COVID-19 variants. However, there is a possibility that this higher rate of complications from COVID-19 among HD patients in the western region compared to other regions is a true difference. This possibility is because the complications rate among HD patients may mirror that of the general population. In the general population, data looking at the overall mortality rate caused by COVID-19 in Saudi Arabia by region found that the highest rate is in the western region, specifically Makkah city [20]. Another data which looked at the incidence of the prevalence of COVID-19 in Saudi Arabia found that it varies by region or areas, reflected by a higher seroprevalence rate of COVID-19 observed in Makkah city compared to some other cities [21]. This could be explained by the fact that the city of Makkah and Medina cities are travel destinations for millions of pilgrims across the world, and international travel has been shown to have a major role in the spreading of COVID-19 [22]. Even before the era of COVID-19, it was known that the epidemiology of respiratory viruses in Saudi Arabia is likely affected by the mass gathering during the Islamic rituals (Hajj and Umrah) in the holy sites of Makkah and Medina [23]. In fact, a few cases of COVID-19 occurred in Umrah pilgrims before international travel was banned, and the first patient who died of COVID-19 in Pakistan was a returned Umrah pilgrim.
Saudi Arabia suspended the Umrah on March 03, 2020, and on June 22, 2020, the Saudi government announced the complete ban of international visitors for the 2020 annual Hajj pilgrimage to Makkah, and Hajj was restricted to a limited number of residents who had no chronic diseases and were younger than 65 years. Even after the end of the global health emergency of COVID-19, Makkah and Medina cities will continue to require more efficient preventative measures and support compared to other cities, as they will continue to be a travel destination for millions of pilgrims across the world. These measures will have a national and international impact on controlling COVID-19 pandemic. Our current study is limited by the fact that it was retrospective, had a small sample size, and some patients had missing laboratory data during the peak of the pandemic when no more laboratory reagents were available. Additionally, the limited number of patients who had received the vaccine or some other lines of management (e.g. antiviral or tocilizumab) makes it difficult to study their effects on outcomes.
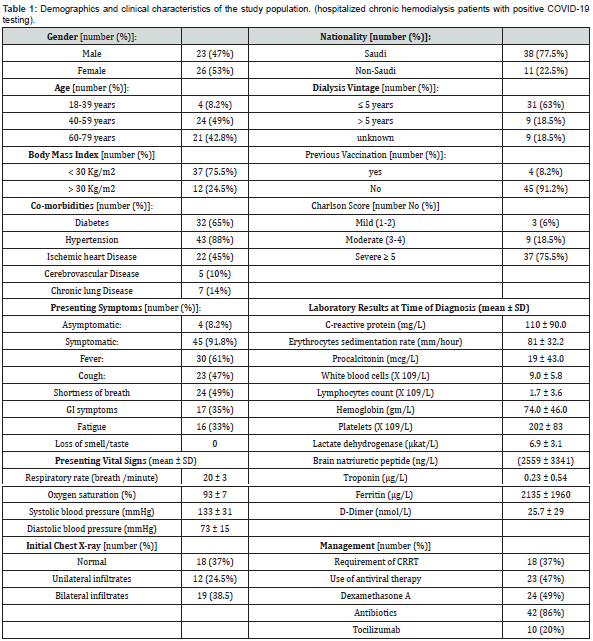
CRRT: Continous Renal Replacement therapy, SD: standard deviation.
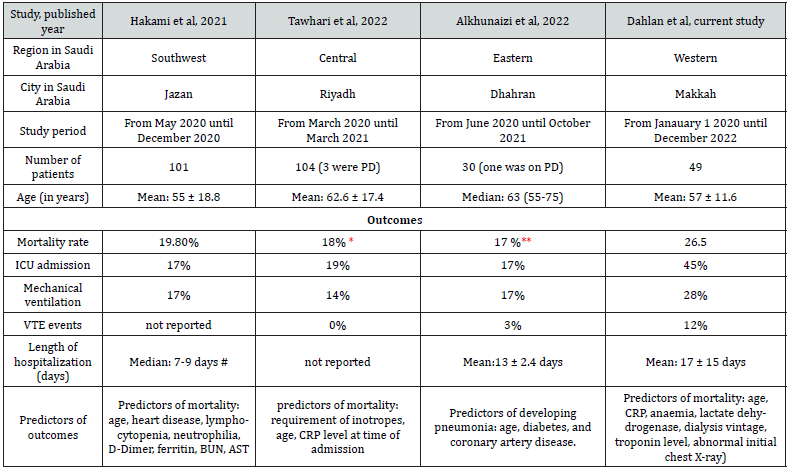
#: Median duration from admission to recovery: 7 days, median duration from admission to death: 9 days
*: The mortality rate was 23% among patients who were symptomatic at time of diagnosis.
**: The mortality rate was 30% among patients who developed pneumonia
AST: aspartate transaminase, BUN: blood urea nitrogen, CRP: C-reactive protein, ICU: intensive care unit, PD: peritoneal dialysis, VTE: venous thromboembolism,
Note: all studies looked at hospitalized patients, except Alkhunaizi et al study (90% of patients were hospitalized).
Conclusion
Our study agrees with other national and international studies which showed a high rate of mortality from COVID- 19 infection among chronic hemodialysis patients compared to the rate observed in the general population. Age, initial hemoglobin, LDH, CRP levels, and abnormal CXR on presentation are found to be predictors of mortality in this study. There is a tendency or a possibility of a geographical pattern of excess rate of complications from COVID- 19 among chronic dialysis patients in Makkah city compared to other cities in Saudi Arabia. Although this finding needs to be supported by a stronger level of evidence and large sample size, this possibility falls in with the available data about a higher rate of COVID-19 mortality in the western region (specifically Makkah) observed in the general population when compared to other regions. Mass gathering, during the Islamic rituals (Hajj and Umrah) in Makkah and Madina cities of the western region, takes place every year. The International Society of Nephrology is calling for a higher prioritization of chronic dialysis patients worldwide to receive COVID-19 vaccination, and we call for a local prioritization for those who live in the western region of Saudi Arabia, especially Makkah and Medina cities. Not only to give them priorities for vaccination but for all other supportive and preventative measures, as these preventative measures will likely have national and international beneficial effects.
References
- Zhu N, Zhang D, Wang W, Li X, Yang B, et (2020) A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 382(8): 727-733.
- Caplin B, Ashby D, McCafferty K, Hull R, Asgari E, et al. Risk of COVID-19 Disease, Dialysis Unit Attributes, and Infection Control Strategy among London In- Center Hemodialysis Patients. Clin J Am Soc Nephrol 16(8):1237-1246.
- Valeri AM, Robbins-Juarez SY, Stevens JS, Ahn W, Rao MK, et Presentation and Outcomes of Patients with ESKD and COVID-19. J Am Soc Nephrol 31(7):1409-1415.
- Stefan G, Mehedinti AM, Andreiana I, Zugravu AD, Cinca S, et al. Clinical Features and Outcome of Maintenance Hemodialysis Patients with COVID- 19 from A Tertiary Nephrology Care Center in Romania. Ren Fail 43(1): 49-57.
- Ng JH, Hirsch JS, Wanchoo R, Sachdeva M, Sakhiya V, et al. Outcomes of patients with end-stage kidney disease hospitalized with COVID-19. Kidney Int 98(6): 1530-1539.
- Guidotti R, Pruijm M, Ambühl PM (2022) COVID-19 Pandemic in Dialysis Patients: The Swiss Experience. Front Public 10: 795701.
- Almonte K, Weiner DE (2020) COVID-19 Universal Testing in Hemodialysis Facilities to Reduce Infection Kidney Med. 2(6): 681-683.
- Goicoechea M, Sánchez Cámara LA, Macías N, Muñoz de Morales A, et al. (2020) COVID-19: clinical course and outcomes of 36 hemodialysis patients in Kidney Int 98(1): 27-34.
- Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU): COVID-19 Dashboard by CSSE at JHU.
- Ziemba R, Campbell KN, Yang TH, Schaeffer SE, Mayo KM, et al. (2020) Excess Death Estimates in Patients with End- Stage Renal Disease - United States, February-August 70(22): 825-829.
- Tawhari M, Alrushid E, Alquwaiee G, Alanazi S, Alkhudair J, et al. (2022) Presentation and Outcomes of Patients with End-Stage Kidney Disease Hospitalized With COVID-19 at a Tertiary Center in Riyadh, Kingdom of Saudi Arabia. 14(3): e23575.
- Hakami A, Badedi M, Elsiddig M, Nadeem M, Altherwi N, et al. (2021) Clinical Characteristics and Early Outcomes of Hospitalized COVID-19 Patients with End-Stage Kidney Disease in Saudi Int J Gen Med 14: 4837-4845.
- Alkhunaizi AM, Elnabi HA, Amir A, Anwar A (2022) COVID-19 in patients with end stage kidney disease at a large community hospital in Eastern Saudi A prospective study. Saudi Med J. 2022 43(6): 633-636.
- Center for Disease Control and Prevention (2020) The Advisory Committee on Immunization Practices’ Updated Interim Recommendation for Allocation of COVID-19 Vaccine United States.
- Francis A, Baigent C, Ikizler TA, Cockwell P, Jha V (2021) The urgent need to vaccinate dialysis patients against severe acute respiratory syndrome coronavirus 2: a call to Kidney Int 99(4): 791-793.
- Alfano G, Ferrari A, Magistroni R, Fontana F, Cappelli G, et al. (2021) The Frail World of Hemodialysis Patients in the COVID-19 Pandemic Era: A Systematic Scoping J Nephrol 34(5): 1387-1403.
- Alberici F, Delbarba E, Manenti C, Econimo L, Valerio F, et al. (2020) A report from the Brescia Renal COVID Task Force on the Clinical Characteristics and Short-term Outcome of Hemodialysis Patients with SARS-CoV-2 Infection. Kidney Int 98(1): 20-26.
- Stefan G, Mehedinti AM, Andreiana I, Zugravu AD, Cinca S, et al. Clinical Features and Outcome of Maintenance Hemodialysis Patients with COVID-19 from A Tertiary Nephrology Care Center in Romania. Ren Fail. 43(1): 49-57.
- Tomacruz ID, So PN, Pasilan RM, Camenforte JK, Duavit MI (2021) Clinical Characteristics and Short-Term Outcomes of Chronic Dialysis Patients Admitted for COVID-19 in Metro Manila, Philippines. Int J Nephrol Renovasc Dis 14: 41-51.
- Javed N, Zuber M, Amin S, Bugis B, Al-Mohaithef M (2022) COVID-19 cases and deaths after implementation of prevention strategies, Saudi East Mediterr Health J 28(2): 95-107.
- Alharbi NK, Alghnam S, Algaissi A, Albalawi H, Alenazi MW, et al (2021) Nationwide Seroprevalence of SARS-CoV-2 in Saudi J Infect Public Health 14(7): 832-838.
- Hoang VT, Gautret P, Memish ZA, Al-Tawfiq JA (2020) Hajj and Umrah Mass Gatherings and COVID-19 Curr Trop Med Rep 7(4): 133-140.
- Farrag MA, Hamed ME, Amer HM, Almajhdi FN (2019) Epidemiology of respiratory viruses in Saudi Arabia: toward a complete Arch Virol 164(8): 1981-1996.






























