Spermatic Cord Leiomyosarcoma: What is the Urologist’s Role?
Mohammed Alae Touzani1,2*, Souhail Regragui1,2, Amine Slaoui1,2, Nabil Jakhlal1,2, Tariq Karmouni1,2, Khalid El Khader1,2, Abdellatif Koutani1,2 and Ahmed Ibn Attya Andaloussi1,2
1Faculty of Medicine and Pharmacy, Mohammed V University, Morocco
2 Urology Department, Ibn Sina Teaching Hospital, Morocco
Submission: July 11, 2019; Published: July 23, 2019
*Corresponding author:Mohammed Alae Touzani, Faculty of Medicine and Pharmacy, Mohammed V University, Urology Department, Ibn Sina Teaching Hospital, Morocco
How to cite this article:Md Alae T, Souhail R, Amine S, Nabil J, Tariq K, et al. Spermatic Cord Leiomyosarcoma: What is the Urologist’s Role?. JOJ uro & nephron. 2019; 6(5): 555698. DOI: 10.19080/JOJUN.2019.06.555698
Abstract
Introduction: Spermatic cord tumors always represented a challenge for urologists, given their rarity and, thus, the lack of guidelines concerning surgical treatment and oncological follow-up. Spermatic cord leiomyosarcome (SCL) is one of the rarest and most aggressive tumor type. It is characterized by a painless clinical presentation, with a slow growing para testicular mass, contrasting with very aggressive histological features. Surgery is the first step in the patient’s care, and it must follow several rules when a SCL is suspected.
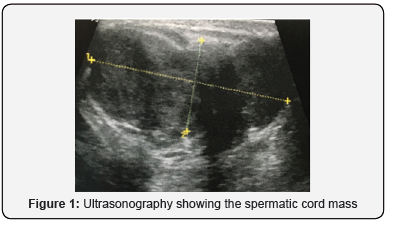
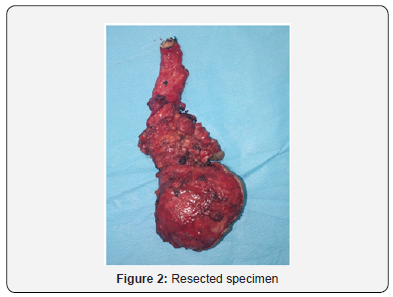
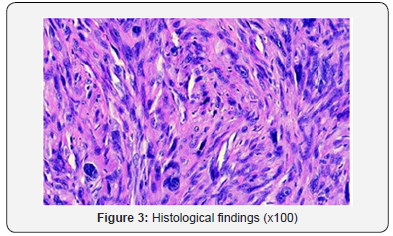
Case Report: We present here the case of a 78-year-old man who consulted for a left testicle swelling without pain nor inflammatory signs since several months. The clinical examination revealed a painless tumefaction of the left spermatic cord. An ultrasonography performed showed a heterogeneous left spermatic cord mass, measuring 45 mm x 15 mm, with a suspicion of left testicle infiltration, which is the seat of a mild hydrocele. The patient underwent a hemicortectomy with orchidectomy with a high ligation of the spermatic chord, and excision of the adjacent skin. The post-operative course was normal. The histological and immunohistochemical study concluded to a leiomyosarcoma. Surgical margins were clear. After a two-year follow-up, clinical examination and imaging showed neither signs of recurrence, nor metastasis.
Conclusion: SCL is a rare, but very aggressive form of spermatic cord tumors. While the therapeutic strategy is not well codified, surgery is ruled by a wide tumor resection. The outcome depends on the margins and the histological features (grade).
Keywords:Spermatic cord, Testicle, Leiomyosarcoma, Surgery
Introduction
Spermatic cord tumors always represented a challenge for urologists, given their rarity and, thus, the lack of guidelines concerning surgical treatment and oncological follow-up. Spermatic cord leiomyosarcome (SCL) is one of the rarest and most aggressive tumor type. It is characterized by a painless clinical presentation, with a slow growing paratesticular mass, contrasting with very aggressive histological features. Surgery is the first step in the patient’s care, and it must follow several rules when a SCL is suspected.
Case Report
We present here the case of a 78-year-old man who consulted for a left testicle swelling without pain nor inflammatory signs since several months. The clinical examination revealed a painless tumefaction of the left spermatic cord. An ultrasonography performed showed a heterogeneous left spermatic cord mass, measuring 45 mm x 15 mm, with a suspicion of left testicle infiltration, which is the seat of a mild hydrocele (Figure 1). The patient underwent a hemicortectomy with orchidectomy with a high ligation of the spermatic chord, and excision of the adjacent skin (Figure 2). The post-operative course was normal. The histological and immunohistochemical study concluded to a leiomyosarcoma (Figure 3). Surgical margins were clear. After a two-year follow-up, clinical examination and imaging showed neither signs of recurrence, nor metastasis.
Discussion
The origin of SCL has a direct implication on surgical treatment. Indeed, it originates from muscle cells of the cremaster, arterial walls or vas deferens wall, and so, the surgical management is based on an en-bloc resection of the testicle, epididymis, and spermatic chord with a high ligation of it, and a large excision of adjacent tissues, mainly fat, muscles and skin [1].
The SCL is mostly found in elderly patients. Less than 100 cases have been described. After liposarcomas, it is the the most frequent paratesticular malignancy (20 %) [2,3]. It is often a palpable and painless spermatic cord mass, and the testicular origin is easily dismissed. However, in case of large mass and/or infiltration of the testicle, diagnosis is more difficult, and it can be taken for a huge hernia or testicular tumor. Ultrasonography can reveal a heterogeneous spermatic cord mass, with necrosis areas, rarely calcifications and hypervascularization on Doppler [4]. Several authors recommend performing a thoracoabdominal CT-scan for staging the tumor before surgery [2,3]. It can also be done after surgery.
The first step of treatment is surgery: orchidectomy with a high ligation of the spermatic chord, and large excision of the adjacent tissues [5]. Indeed, sarcoma’s “pseudo-capsule” is often infiltrate by tumor cells, and in case of a resection flush to the tumor, there is high rates of residual disease and recurrence. Thereby, a wide excision is necessary to locally control the SCL. In case of the histological study concluded for positive margins, a re-intervention with large excision of tissues is required [5].
As in our case, if the tumor is small and localized in the lower spermatic cord segment, hemiscrotectomy must be realized and skin reconstruction is easy. Contrariwise, if the tumor is large and/or localized in the upper spermatic cord segment or in the inguinal segment, the large excision may sacrifice the abdominal wall muscles, skin and fat, or sometimes the pubis bone [5]. ENOCH and al. described the different techniques for reconstruction of the anterior abdominal wall and inguinal region, ranging from skin and fat flaps, to muscle flaps and free flaps. This is depending on the nature of tissue loss, the flap avaibility and the surgeon experience [5]. We did not find any case in literature of vascular (femoral vein or atery) involvement of SCL. This constitutes, in theory, a greater surgical challenge requiring the placement of vascular graft in a patient in which complete resection would be more than doubtful. Concerning systematic retroperitoneal lymph nodes dissection (RPLND), there is not enough data and evidence to recommend it for SCL, unless CT-scan shows nodal involvement.
Because of the high rates of recurrences, data suggest that patients should undergo an adjuvant radiation therapy (ART), especially when the tumor is high-grade or the complete resection is doubtful [2,5]. With ART, the recurrence rate decreases by 10 to 30 % [2,5]. It should include the resection bed, inguinal canal and pelvic nodes. There is not enough data to suggest that neoadjuvant radiation therapy or chemotherapy can improve neither survival nor recurrence [2].
Conclusion
SCL is a rare, but very aggressive form of spermatic cord tumors. While the therapeutic strategy is not well codified, surgery is ruled by a wide tumor resection. The outcome depends on the margins and the histological features (grade). Adjuvant radiotherapy should be proposed for unfavorable prognostic patients.
References
- Frigerio P, Muruato Araiza JS, Marcos-Morales S, CepedaNieto AC, Berdeal-Fernandez E, et al. (2016) Spermatic Cord Leiomyosarcoma Rare Case. Urol Case Rep 6: 15-17.
- Beydoun B, Weinberg B, Hurst N, Khoury N, Ahmed S, et al. (2017) A case of spermatic cord leiomyosarcoma: Clinical presentation, treatment and literature review. Appl Rad Oncol 6(4): 37-40.
- Moschini M, Mattei A (2017) Diagnosis and management of spermatic cord tumors. Curr Opin Urol 27(1): 76-79.
- Secil M, Kefi A, Gulbahar F, Aslan G, Tuna B, et al. (2004) Sonographic features of spermatic cord leiomyosarcoma. J Ultrasound Med 23(7): 973–976.
- Enoch S, Wharton SM, Murray DS (2005) Management of leiomyosarcomas of the spermatic cord: the role of reconstructive surgery. World J Surg Oncol 3: 23.






























