Prospective Evaluation of Postoperative Complications of Radical Cystectomy according to Clavien Dindo Classification: Laparoscopy Versus Conventional Surgery
Mrabet FZ and Moudouni I Sarf*
Department of Urology, A Ibn Tofail Hospital, Morocco
Submission: May 30, 2018; Published: June 15, 2018;
*Corresponding author: Fatima Zahra Mrabet, Department of Urology, A Ibn Tofail Hospital, Morocco, Email: mrabetfatimazahra@gmail.com
How to cite this article: Mrabet FZ, Moudouni I S. Prospective Evaluation of Postoperative Complications of Radical Cystectomy according to Clavien Dindo Classification: Laparoscopy Versus Conventional Surgery. JOJ uro & nephron. 2018; 5(4): 555670. DOI: 10.19080/JOJUN.2018.05.555670
Summary
Radical cystectomy with lymphadenectomy is the standard treatment for invasive bladder tumors and non-muscle invasive high-grade and/or recurrent after conservative treatment. The objective of this work is to make a comparison between the results of the cystectomy surgery for patients operated by laparoscopy with those operated by conventional surgery in terms of postoperative morbidity using the classification of CLAVIEN DINDO because it meets requirements internationales relying on more concrete criteria and gone in five grades upward gravity goals. Over a period of 6 years, a sample of 80 patients who underwent surgery for bladder tumor were part of our study. 40 are operated by laparoscopy (group1) and 40 by conventional surgery (Group 2) in the Urology’s serviceMed VI’s hospital Marrakech .Intraoperative there was a significant reduction in blood loss in group 1, with fewer complications despite a significantly longer operative time, post operative pain was significantly decreased in group1 with consumption significantly lower analgesic, a resumption of transit significantly earlier and an average length of post operative stay significantly shorter in the same group . there was no significant difference in the postoperative complications between the two groups .This prospective study shows, with a review of the literature, the benefits of Laparoscopy allows a quicker recovery, decreased postoperative morbidity and mortality. However, larger cohorts with a long decline is necessary to judge the superiority of one surgical technique to another
Keywords: Bladder neoplasm; Radical cystectomy; Laparoscopy; Conventional surgery; Post operatives complications
Introduction
Laparoscopy has now become a common surgical approach that is increasingly used in public and private hospitals. Indeed, it tends to achieve a real alternative to conventional surgery called «open». The main advantage of this approach compared to conventional surgery is the reproduction of what is done in conventional minimally invasive surgery. This means a significant reduction in parietal and visceral trauma, and therefore a reduction of postoperative pain. This saves time in hospitalization and convalescence, not to mention the aesthetic benefit of the scar.
Materials and Methods
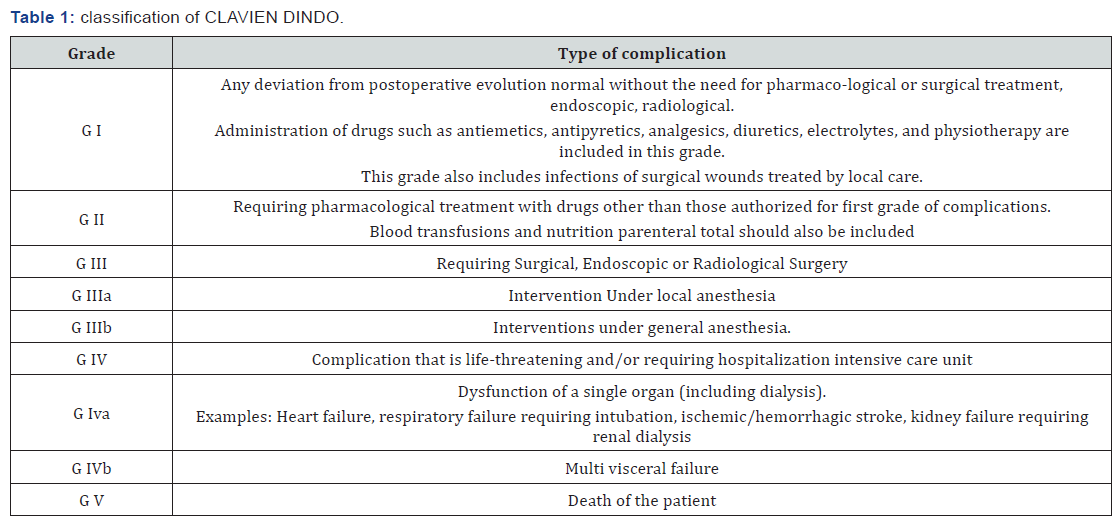
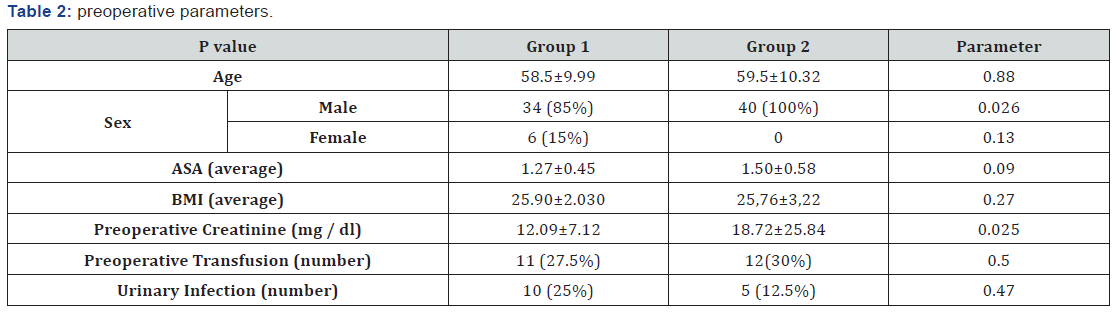
Our work is a prospective, non-randomized study comparing the results of radical cystectomy for bladder tumors laparoscopically (group 1) and by conventional surgery (group 2). Its objective is to evaluate the experience of the urology department at the MED-VI Medical Center of Marrakech in laparoscopy in terms of postoperative morbidity. The study concerns 80 patients with bladder tumor, of which 40 were operated by laparoscopy (group1), and 40 by conventional surgery (Group 2). the complications noted were classified according to the classification of «CLAVIEN DINDO», the latter, developed by CLAVIEN in 2004 [1] and revised by DINDO in 2009 [2], is considered a simple, reproducible and applicable classification whatever the field Surgical, it has 5 grades of complications of increasing severity which is based mainly on the type of therapy needed to curb the complication (Table 1 & 2). the statistical analysis was carried out at the epidemiology laboratory of the Faculty of Medicine and Pharmacy of Marrakech using a descriptive analysis for the qualitative variables (percentages, means and standard deviations) and a univariate analysis (test of Pearson’s khi2, student test and fisher’s exact test), the software used during the study is the SPSS version 16, the significance level set at 5%.
Results and Analyzes
Per operating, in group 1: The average operating time was 298.75±72min and the blood loss was between 60 and 700cc. In group 2: the operating time varies between 150min and 480min and blood loss is between 200 and 1500cc. In group 2: 1 patient (2.5%) had a perioperative rectal wound related to dissection of the posterior surface of the bladder, 2 patients (5%) presented with perioperative hemorrhage, in 1 patient in connection with the bleeding of Santorini and in the other in relation to poor control of the laterovesical pedicle. 13 patients (32.5%) required intraoperative transfusion because of significant bleeding (including 2 patients related to the bleeding incident). In group 1: 2 patients (5%) presented a vascular lesion of the epigastric artery at the introduction of the trocar easily controlled by bipolar forceps. 1 patient (2.5%) required an intraoperative transfusion, related with bleeding peroperatively. EVA in group 1 indicated «4» [3,4]. In group 2: The EVA indicated «6» [5,6]. In group 1: The mean transit time was 1.9±0.6 days and 2.4±0.9 in group 1 and 2 respectively. The mean time to resumption of feeding was 4.45±1.5 days and 4.7±1.7 days in the group 1 and 2 respectively. The duration of hospitalization was in average 8.5±5.3 days for group 1 and 11±5.4 days in group 2.
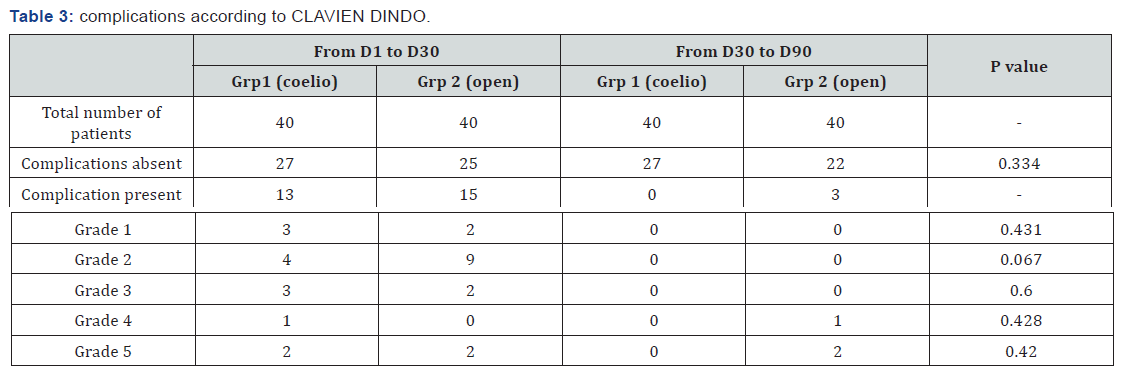
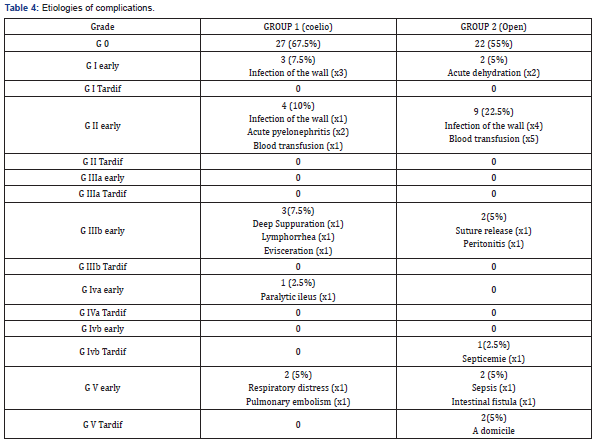
For the results of postoperative complications of the two groups of our study are shown in Table 3 according to CLAVIEN DINDO classification, for the etiologies of these complications, they are shown in Table 4.
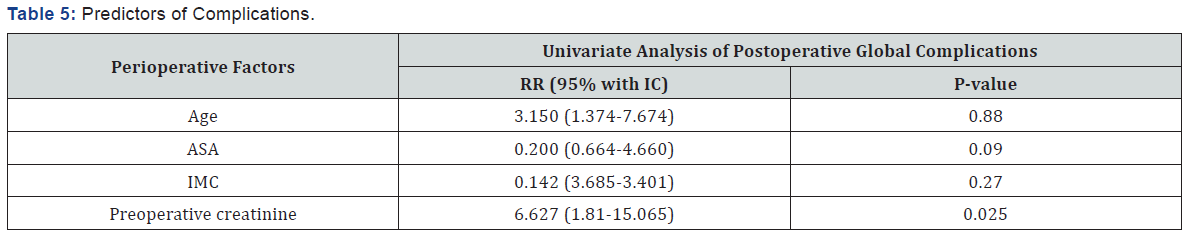
The perioperative factors that may influence the overall complication rate in the series, namely age, ASA score, BMI, and preoperative creatinine, were subject to univariate analysis; the results showed that in our current series there is no correlation between these perioperative factors and the increase in the rate of global complications (Table 5).
Radical cystectomy with pelvic lymph node dissection is the standard treatment for infiltrating or non-muscle invasive bladder tumors and/or recurrent after conservative treatment [7], our review of the literature found only three prospective comparative studies, comparing the morbidity of two conventional and laparoscopic approaches and which, unfortunately, treat the chapter «postoperative complications» by an old and non-standardized method [major or minor complication]. In our literature search we found no study that deals with the «complications of cystectomy» using CLAVIEN DINDO’s classification, hence the importance of our work which brings together a series, certainly at its beginning but which reflects a courageous approach to our service to a technique that is worldwide in testing and expertise. Throughout our series, we have found a significant length of laparoscopic surgical procedure compared to conventional surgery, the same results were found by Guillotreau J et al. [3] in a prospective series comparing 38 laparoscopic cystectomies to 30 open cystectomies as well as Hemal AK et al. [5] in their prospective series of 35 laparoscopic radical cystectomies compared to 30 patients operated by laparotomy. Laparoscopic cystectomy is a procedure that combines both the difficulties of laparoscopy and those of pelvic cancer surgery while respecting the principles of minimally invasive surgery, including careful haemostasis to ensure a clean surgical field. This may explain this lengthening of the operating time. G-Pascal Haber [8], Guillotreau and Hemal and others have shown that blood loss is significantly lower in laparoscopy, which was the same for our work. A more precise dissection, a better vision of the small vessels and a fine coagulation with the bipolar forceps can explain it. It is recognized today that the laparoscopic approach in cystectomy reduces the use of analgesics postoperatively and avoids the use of opioids [4,5,8- 10]. The EVA used for the assessment of pain in our patients indicated «4» in group 1 against «5.3» in group 2. Ileus is the most common complication after cystectomy [6,11] and a usual cause of prolongation of hospitalization [12], laparoscopy allows to decrease it, which has been proven through comparisons of Porpiglia et al. [13]. Basillote as well as Guillotreau, our study concluded with the same results. This reduction of pain with the reduction of analgesic consumption, and the early resumption of transit allows early ambulation, hence a decrease in the risk of pulmonary infection, and a reduction in the duration of hospitalization which is clearly lower in our series. Laparotomy cystectomy is an intervention associated with morbidity rates of 25 to 35% and mortality rates of up to 4% [1,12] regarding laparoscopic cystectomy. Haber [15] had shown a greater morbidity and surgical revision with laparoscopic derivation. Our classification of postoperative complications did not show any difference between the two groups despite a higher parietal complication rate in the second group, the same results being found by the different comparative studies except that of Guilletreau.
Conclusion
In our current experience, there is no difference in morbidity between laparoscopy and conventional surgery, but the difference that would make the difference statistically significant, between the two approaches, in favor of laparoscopy, would come with the increase of the number of patients compared and the improvement of the operative technique. The terms «MINOR» and «MAJOR» used to report the complications of a surgical technique must be removed from the surgical literature as they give a subjective, ambiguous, inaccurate and confusing picture of the real value of these complications. Thus modification of the general principle of classification of surgical complications is warranted for ongoing clinical trials and randomized studies have more hindsight to judge the efficacy of a laparoscopic procedure.
References
- Clavien PA, Barkun J, de Oliveira ML, Vauthey JN (2009) The Clavien- Dindo classification of surgical complications: five-year experience. Ann Surg 250(2): 197-198.
- Daniel D, Demartines N, Pierre-Alain C (2004) Classification of Surgical Complications A New Proposal with Evaluation in a Cohort of 6336 Patients and Results of a Survey. Annals of Surgery 240(2): 522-530.
- Guillotreau J, Gamé X, Mouzin M, Doumerc N, Mallet R, et al. (2009) Radical cystectomy for bladder cancer: morbidity of laparoscopic versus Open Surgery. J Urol 181(2): 554-559.
- Cathelineau X, Arroyo C, Rozet F, Vallancien G (2005) Laparoscopic assisted radical cystectomy: the montsouris experience after 84 cases. Eur Urol 47(6): 74-80.
- Hemal AK, Kolla SB (2007) Comparison of laparoscopic and open radical cystoprostatectomy for localized bladder cancer with 3-Year oncological followup: a single surgeon experience. J Urol 178(6): 2340- 2234.
- Zerbib M, Bouchot O, Coloby P (2002) Mortalité, morbidité et résultats fonctionnels de la cystectomie totale. Prog Urol 12: 891-911.
- Jakse G, Algaba F, Fossa S, Stenzl A, Sternberg C (2006) Recommendations on muscle-invasive and metastatic bladder cancer. EAU Guidelines 44: 350-366.
- Haber GP, Crouzet S, Gill IS (2008) Laparoscopic and robotic assisted radical cystectomy for bladder cancer: a critical analysis. European Urology 54(1): 54-62.
- Basillote JB, Abdelshehid C, Ahlering TE, Shanberg AM (2004) Laparoscopic assisted radical cystectomy with ileal neobladder: a comparison with the open approach. J Urol 172(2): 489-493.
- Simonato A, Gregori A, Lissiani A, Bozzola A, Galli S (2005) Laparoscopic radical cystoprostatectomy: our experience in a consecutive series of 10 patients with a 3 years follow-up. Eur Urol 47(6): 785-792.
- Chang SS, Cookson MS, Baumgartner RG, Wells N, Smith JA (2002) Analysis of early complications after radical cystectomy: results of a collaborative care pathway. J Urol 167(5): 2012-2016.
- Novotny V, Hakenberg OW, Wiessner D, Heberling U, Litz RJ, et al. (2007) Perioperative complications of radicalcystectomy in a contemporary serie. Euro Urol 51(2): 397-401.
- Porpiglia F, Renard J, Billia M, Scoffone C, Cracco C, et al. (2007) Open versus laparoscopy-assisted radical cystectomy: results of a prospective study. J Endourol 21(3): 325-329.
- Vaessen C, Mouzin M, Malavaud B, Gamé X, Berrogain N, et al. (2004) Cystoprostatectomie laparoscopique, expérience initiale à propos de 13 cas. Prog Urol 14: 590-593
- Haber GP, Campbell S, Colombo JR, Fergany A, Kaouk J, et al. (2006) Cystectomie totale laparoscopique avec dérivation urinaire : «laparoscopie pure » versus «laparoscopie assistée ». Prog Urol 16(1): 40-46.






























