Salvage Lymphadenectomy in the Treatment of Nodal Recurrence of Prostate Cancer Detected by Magnetic Resonance Imaging and PET-PSMA CT - Case Report
Rodrigo Galves Mesquita Martins, André Luiz Lima Diniz, Ulisses Lopes Guerra Pereira Sobrinho, Diogo Eugenio Abreu da Silva, Tomás Accioly de Souza and José Anacleto Dutra de Resende Júnior*
Department of Urology, Lagoa Federal Hospital, Rua Jardim Botânico, Brazil, USA
Submission: September 14, 2017; Published: October 31, 2017
*Corresponding author: José Anacleto Dutra de Resende Júnior, Department of Urology, Lagoa Federal Hospital. Rua Jardim Botânico 501-6° andar, Jardim Botânico, Rio de Janeiro, Brazil, USA, Tel:+55(21)3111.5363 ; Email: joseanacletojuniour@gmail.com
How to cite this article: Martins RGM, Diniz ALL, Sobrinho ULGP, Silva DEA, Souza TA, Resende Junior JAD. Salvage Lymphadenectomy in the Treatment of Nodal Recurrence of Prostate Cancer Detected by Magnetic Resonance Imaging and PET-PSMA CT - Case Report. JOJ uro & nephron. 2017; 4(2): 555632. DOI:10.19080/JOJUN.2017.04.555632
Abstract
EFR, 63 years Diagnosis of prostate adeno carcinoma Gleason 6 (3+3) by biopsy indicated by elevation of PSA (4.8mg/dl), in 2011. Patient underwent Radical Prostatectomy (RP) by sampling obturator lymphadenectomy, whose histopathological report revealed ACP Gleason 8 (5+3) with free margins (pT2C) and lymph nodes with no malignancy (pN0). The PSA remained null during the three consecutive years, in 2014 PSA raised (3.14mg/dl). In 2016 PSA reached 17mg/dl. His disease was re-staged and 68Ga-PSMA-PET/CT revealed areas with anomalous increase of 68Ga-PSMA expression in periaortic and iliac lymph nodes on the left, suggestive of secondary neoplastic lesions. In august 2016, patient underwent retroperitoneal Salvage Lymphadenectomy. Lymph node enlargement was identified in the left obturator chain, left external iliac, paracaval and periaortic chain.
The histopathological report described metastatic bilaterally obturator chain carcinoma, left internal iliac, pre-sacral left and paraaortic. The 30-day postoperative PSA was 2.57. Salvage Lymphadenectomy is a path for treatment in patients with disease relapse limited to the LNM after RP, it is a method that can postpone androgen deprivation therapy and chemotherapy; clinical trials are needed to legitimize surgery in this specific scenario.
Keywords:Precision medicine; Hybrid imaging; 68Ga-PSMA-PET/CT; Prostate cancer; Salvage lymphadenectomy
Introduction
Prostate cancer (PC) still remains the most frequent oncologic disease in the urogenital tract, the second most frequently diagnosed cancer among men and the 5th leading cause of cancer death worldwide [1]. Screening may increase the chances of detection of the disease in the early stages however, despite all the technological advances and debates on the management of localized disease RP remains a good treatment option [2]. Unfortunately a successful surgery does not mean a disease-free status at the long term. A significant proportion of men undergoing curative treatment for PC will develop biochemical recurrence (BR) [3]. Some studies have shown proportion ranging from 15% to 40% of BR between those men treated by RP, which can be associated with local or systemic remaining of the disease [4,5].
Presenting concerns and diagnostic assessment
EFR, 63 years diagnosis of prostate adenocarcinoma Gleason 6 (3+3) by biopsy indicated by elevation of PSA (4.8mg/dl), in 2011.Patient underwent RP by sampling obturator lymphadenectomy, whose histopathological report revealed ACP Gleason 8 (5+3) with free margins (pT2C) and lymph nodes with no malignancy (pN0). The PSA remained null during the three consecutive years, in 2014 PSA raised (3.14mg/dl), clinical follow-up was choosed by assistents in his hometown. In 2016 he was referred to Federal Hospital of Lagoa Rio de Janeiro-Brazil, because PSA reached 17mg/dl. As inicial treatment received hormone-therapy, falling PSA to 10mg/dl. His disease was re-staged between june and july, results are bellow:

- Bone 99mTechnetium scintigraphy: Low probability of blast bone metastases.
- MRI: Lymph nodes 3.4cm and 2.3cm, showing signs of heterogeneous uptake by the contrast medium, at the level of the external iliac chain on the left. A 3.5cm lymph node with heterogeneous contrast uptake at the transition between the abdominal aorta and the left common iliac artery (Figure 1).
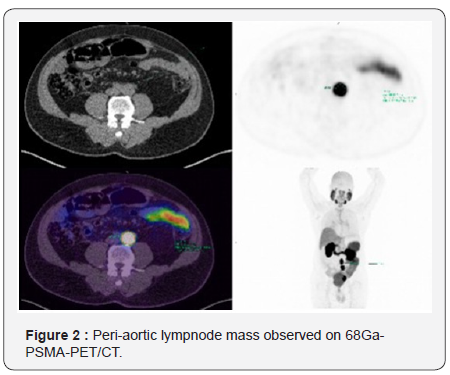
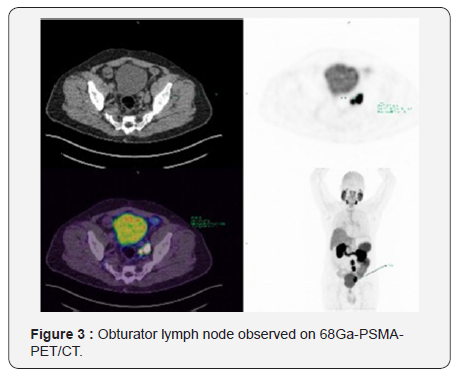
- 68Ga-PSMA-PET/CT: Areas with anomalous increase of 68Ga-PSMA expression in periaortic and iliac lymph nodes on the left, suggestive of secondary neoplastic lesions (Figure 2 & 3).
In august 2016, patient underwent retroperitoneal S-LND (Figure 4A & 4B). Lymph node enlargement was identified in the left obturator chain, left external iliac, paracaval and periaortic chain. Procedure extended for 4 hours. Blood loss was minimal. There were no intra operative or extra operative complications, being discharged on the 6th day after surgery. The 30-day postoperative PSA was 2.57. The histopathological report described metastatic bilaterally obturator chain carcinoma, left internal iliac, pre-sacral left and paraaortic.

Discussion
The improvement of imaging methods helped us to understand the scenario of biochemical recurrence in patients submitted to radical prostatectomy. Heidenreich et al. [6] purposed oligometastatic PC as defined by three or less to five metastatic lesions, no rapid spread to more sites, and feasibility of targeted treatment of all metastatic lesions with surgery or radiation therapy. Hövels et al. [7] perfomed a meta-analysis including 24 studies and showed that CT and MRI have both a poor performance on identifying LMN. For CT, pooled sensitivity was 0.42 (0.26-0.56; 95% CI) and pooled specificity was 0.82 (0.8-0.83; 95% CI). For MRI, the pooled sensitivity was 0.39 (0.22-0.56 95% CI) and pooled specificity was 0.82 (0.79-0.83; 95% CI) [8]. However, given the availability of access in our environment, both techniques are still used. In the presented case, the MRI was successful due to the high level of PSA and the large lymphnode volume.
A tomography enhanced, the choline PET/CT, has been employed; however, it also might underestimate nodal burden, Passoni NM et al have repoted that only 35% of patients undergoing salvage nodal dissection guidedby choline PET/ CT scan have lymph node metastases limited to the positive spots at preoperative imaging. But in times of precision medicine, it creates an unique need of characterization and location of the cancer [9]. Image and treat’ strategy is possible with 68Ga-PSMAPET/ CT and so, a tailored path to the particular characteristics of the individual cancer patient can be chosen [10]. Rauscher I et al. performed a retrospective study including 48 patients with BR who underwent 68Ga-PSMA-PET/CT imaging, and found that the specificity of 68Ga-PSMA-PET/CT and morphologic imaging was 97.3% and 99.1%, respectively. However, 68Ga-PSMAPET/ CT detected LNM in 53 of 68 histopathologically proven metastatic LN fields (77.9%) whereas morphologic imaging was positive in only 18 of 67 (26.9%) [11].
In terms of surgery, Hadaschik et al. [12] brings a controvertial point which is the extent of treatment once salvage therapy based on PSMA imaging is initiated; in their opinion, the data available today suggest that bilateral template-based surgery should be performed to overcome the limitations of 68Ga-PSMAPET/ CT imaging in detecting micro metastases. S-LDN should be performed according to the surgical team’s expertise and the availability of methods. Montorsi et al. [13] reported their initial experience with robot-assisted salvagenodal dissection for the management of 16 patients with lymphnode recurrence after radical prostatectomy. Median operative time, blood loss, and length of hospital stay were 210min, 250ml, and 3.5 days. The median number of nodes removed was 16.5 [14].
Positive lymph nodes were detected in 11 (68.8%) patients. Overall, four (25.0%) and five (31.2%) patients experienced intra operative and postoperative complications, respectively. Overall, one (6.3%) and four (25.0%) patients had Clavien I and II complications within 30 days after surgery respectively. Overall, five (33.3%) patients experienced BR after robot assisted S-LDN. Their study is limited by the small cohort of patients evaluated, by method of lymph node detection which was by PET/CT and by the short follow-up duration [15].
Despite any imaging method used for diagnosis, Abdollah et al. [16] suggests that when a S-LDN is considered, it should be extended to all regional lymph node stations and not limited to the sites of positive spots at preoperative imaging. Accordingly to their systematic review, data suggest that S-LND can delay clinical progression and postpone hormonal therapy in almost one-third of the patients, although the majority will have BCR. An accurate and attentive preoperative patient selection may help improve these outcomes. The most frequent complication after S-LND was lymphorrhea (15.3%), followed by fever (14.5%) and ileus (11.2%) [17,18].
Conclusion
The evolution of imaging systems is currently at increase, year by year new methods are presented to scientific community. Those tools must be presented to patient carefully [19]. Prospective studies must be performed to increase the level of evidence and help us to establish guidelines for the best orientation of practitioners and patients. S-LND is a path for treatment in patients with disease relapse limited to the LNM after RP, it is a method that can postpone androgen deprivation therapy and chemotherapy; clinical trials are needed to legitimize surgery in this specific scenario. We must be careful to treat the patient before treating his exams [20]. The well-being of those who entrust us to their health should be in the first place. Hippocratic principles should never be forgotten.
References
- Mellman I, Fuchs R, Helenius A (1986) Acidification of the endocytic and exocytic pathways. Annu Rev Biochem 55: 663-700.
- Wellwood JM, Ellis BG, Price RG, Hammond K, Thompson AE, et al. (1975) Urinary N-acetyl-beta-D-glucosaminidase activities in patients with renal disease. Br Med J 16(3): 408-411.
- Dos Santos AC, Colacciopo S, Dal Bo CM, dos Santos NA (1994) Occupational exposure to lead, kidney function tests and blood pressure. Am J Int Med 26(5): 635-643.
- Shibasak T, Nakano H, Ohno I (1994) Effect of pentoxifylline on CdCl -induced nephrotoxici-2ty in the rat. Biol Trace Elem Res 41: 245-251.
- Hong CY, Chia KS (1998) Markers of diabetic nephropathy. J Diabetes Complications 12(1): 43-60.
- Sherman RL, Drayer ED, Leyland JBR (1983) N-Acetyl-betaglucosaminidase and beta 2-microglobulin. Their urinary excretion in patients with renal parenchymal disease. Arch Intern Med 143(6): 1183-1185.
- Hultberg B, Ravnskov U (1981) The excretion of N-acetyl-betaglucosaminidase in glomerulonephritis. Clin Nephrol 15(1): 33-38.
- Jung K, Mattenheimer H, Burchardt U (1992) Urinary Enzymes in Clinical and Experimental Medicine. Springer Verlag, Berlin, Germany.
- Price RG (1992) Measurement of N-acetyl-beta-glucosaminidase and it’s isoenzymes in urine, methods and clinical applications. Eur J Clin Chem Clin Biochem 30(10): 693-705.
- Hofmann W, Guder WG (1989) A diagnostic programme for quantitative analysis of proteinuria. J Clin Chem Clin Biochem 27(9): 589-600.
- Chiu JSP (1994) Models used to asses renal function. Drug Devel Res 32(4): 247-255.
- Price RG (1992) The role of NAG (N-acetyl-D-beta-glucosaminidase) in the diagnosis of kidney disease including the monitoring of nephrotoxicity. Clin Nephrol 38(suppl 1): S14-S19.
- Tucker SM, Pierce RJ, Price RG (1980) Characterization of human N-acetyl-beta-D-glucosaminidase isoenzymes as an indicator of tissue damage in disease. Clin Chim Acta 102(1): 29-40.
- De Duve C (1964) Principles of tissue fractionation. J Theor Biol 6(1): 33-59.
- Thuss S, Milano G, Kubar J, Namer M, Schneider M (1986) Clinical and pharmacokinetics evidence of a life-threatening interaction between methotrexate and ketoprofen. Lancet 1(8475): 256-258.
- Brater DC (1986) Drug-drug and drug-disease interaction with nonsteroidal anti-infamatory drugs. Am J Med 80(1A): 62-77.
- Tracy TS, Krohn K, Jones DR, Bradley JD, Hall SD, et al. (1992) The effect of salicylate, ibuprofen and naproxen on the disposition of methotrexate in rheumathoid arthritis. Eur J Clin Pharmacol 42(2): 121-125.
- Stewart CF, Fleming RA, Arkin CR, Evans WE (1990) Coadministration of naproxen and low-dose methotrexate in patient with rheumathoid arthritis. Clin Pharmacol Ther 47(4): 540-546.






























