Malacoplakia in Urologic Specimen
Sierra Pablo*, Henao Matilde, Gaviria Federico and Velez Alejandro
Department of Urology and Pathology, Hospital Pablo Tobón Uribe, Universidad CES, Colombia
Submission: March 30, 2017; Published: May 30, 2017;
*Corresponding author: Sierra Pablo, Department of Urology and Pathology, Hospital Pablo Tobón Uribe, Universidad CES, Colombia, Email: sierrapablo@hotmail.com
How to cite this article: Sierra P, Henao M, Gaviria F, Velez Alejandro. Malacoplakia in Urologic Specimen. JOJ uro & nephron. 2017; 3(2): 555607. DOI: 10.19080/JOJUN.2017.03.555607.
Abstract
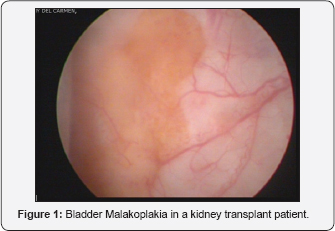
Malacoplakia is an inflammatory condition characterized by yellow-brown plaques with granulomatous lesions. It probably results from abnormal macrophage function in response to a bacterial infection. This rare entity is characterized by one o multiple tumoral growths in any part of the body and is usually misdiagnosed as a malignant condition. The genitourinary tract is frequently involved (up to 75%). Pathologic studies of these lesions show tissue infiltrated by macrophages and hystiocytes with intracytoplasmic inclusions (Michaelis-Gutmann bodies).
There is a very sparse evidence published in the literature, mostly case reports. Previously in 2006 we reported 6 cases of malakoplakia, now we present an update with six additional cases to a total of twelve events in the same institution during a period of 17 years.
Keywords: Malacoplakia; Urinary Tract infections; Prostatitis
Abbreviations:Keywords: MLP: Malacoplakia; MGB: Michaelis-Gutmannbodies; UTI: Urinary Tract Infection; ATB: Antibiotics
Introduction
Malakoplakia is extremely rare granulomatous inflammatory condition that can affect many systems including musculoskeletal, respiratory, and gastrointestinal and specially the urinary tract, most commonly the bladder. It is considered to develop as a result of a defective immune response to bacterial agents, the most common Escherichia coli [1-3]. Although more commonly affects genitourinary tract, isolated cases have been reported in colon, stomach, lung, liver, bone, uterus and skin [4].
In the histopathological examination, malakoplakia is characterized by the presence of foamy histiocytes with distinctive basophilic inclusions, which are known as Michaelis- Gutmannbodies (MGB), this name after whom described the condition in 1902 [5]. It was Von Hansemann in 1903 who employed the word malakoplakia (from the greekmalakos, soft, and plakos, plaque) [6] to define this process according to its macroscopic aspect.
Malakoplakia of the genitourinary system is more commonly diagnosed in women. It is usually observed between the fifth and seventh decades of life but is has been described also in pediatric and other unique group such as kidney transplant immunosuppressed patients.
It is a challenging clinical diagnosis that is usually mistaken for malignancy, it could lead to a formation of a mass anywhere in the urinary tract, elevate prostate specific antigen (PSA), cause visible changes on ultrasound, CT and MRI of the involved organ and promote thickening of the bladder wall forcing erroneous treatments and in some cases radical surgeries [7-9].
Patients and Methods
A retrospective review to identify patients with a diagnosis of malacoplakia of the urinary tract was performed, 12 patients were found to have this diagnosis along 17 years in Hospital Pablo Tobon Uribe and Dinamica IPS in Medellin, Colombia. All cases where evaluated by the same uropathologist and challenging cases where reviewed by and experienced uropathologist in a reference center in US. Records were retrieved and complete clinical history reviewed and described in this case series as well as laboratory findings, pathology specimen and radiology images were included were available. This study was conducted under the Hospital Pablo Tobon Uribe institutional review board and patients confidentiality was assured.
A systematic MEDLINE/Pubmed review was performed on the 27th of may 2016 according to the PRISMA guidelines. The main search terms were "malakoplakia" and"urinary tract". 267 articles were retrieved, 77 articles remained after applying limits for papers published after 2000. The search result was first screened for relevance by title and limited to English and Spanish literature, abstracts were read and 33 publications of interest were selected for full text review. The search was complemented with own files articles, hand search and articles suggested by important publications until no additional papers were retrieved. The search sensitivity was evaluated by comparing the articles identified against those already known to the authors and those cited in previous seminal reviews. If an article was missed, the title and abstract where carefully reviewed to identify terms that would improve the sensitivity of the search.
Results
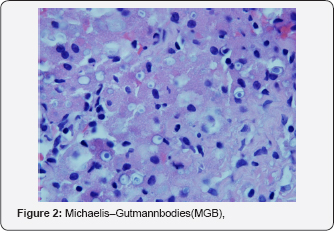
Twelve patients were found to have malakoplakia, median age at presentation was 66.5 years, most patients being older than 35 years (11/12) and only one patient in the pediatric age. Most common organ involved was prostate, in fact 7/12 patients had compromise of this gland, all of them had lower urinary tract symptoms (LUTS), all required surgical intervention due to recurrent UTI and voiding obstruction non responsive to pharmacologic therapy. Interestingly, 3 patients had PSA elevation and a transrectal ultrasound guided biopsy was performed, all evidenced MGB in the pathologic slides confirming malakoplakia, one patient was found with concurrent adenocarcinoma of the prostate and underwent a radical prostatectomy. One of the patients that did not have PSA elevation was taken to transurethral resection of the prostate and was found with prostate cancer along with malacoplakia.
The only pediatric patient is a 4 month old male with an enlarging testicular mass confounded with a neoplasia of the testis at doppler US, serum tumor markers were negative, he was taken to inguinal radical orchiectomy and the final pathologic specimen showed a benign inflammatory process with abundant lymphocytes, plasmocytes, giant cell and hystiocytes with MGB that suggest the diagnosis of MLP, he had a positive urine culture for E. Coli.Patients characteristics are listed on Table 1.
Six of patients had E. Coli proven UTI by urine culture (50%), this percentage is expected be even higher but unfortunately some of the patients didn't have urine culture reports previous to the initiation of antibiotics.
Discussion
Malakoplakia is a rare clinical entity, accurate diagnosis relies on biopsies or surgery specimen reviewed by experienced pathologists. MLP features Hansemanncells , which are hystiocytes with small nuclei and granular acidophilic cytoplasms and MGB, which are basophilic periodic acid- Schiff, diastase-resistant and calcific inclusions seen within the hystiocytes8.This are not usual findings and requires active search for the pathognomonic characteristics of the disease and a good clinical and pathological correlation. Apparently the pathogenesis is explained because impaired host defenses and a defect in phagocytosis not well understood, this would contribute to formation of a granulomatous reaction due to the accumulation of the products of abnormally killed bacteria.
Literature is very scarce on MLP of the urinary tract, most of the published articles are case reports with only a few case series. Velasquez et al9. Previously described the largest report of malakoplakia with the first 6 patients in our institution, in this current case series we added 6 additional patients. Interestingly we have found malakoplakia in a diverse setting and heterogeneous patients, we found compromise in different organs such as testicle, kidney, prostate, bladder, ureters and female reproductive system (cervix, uterus, vagina).
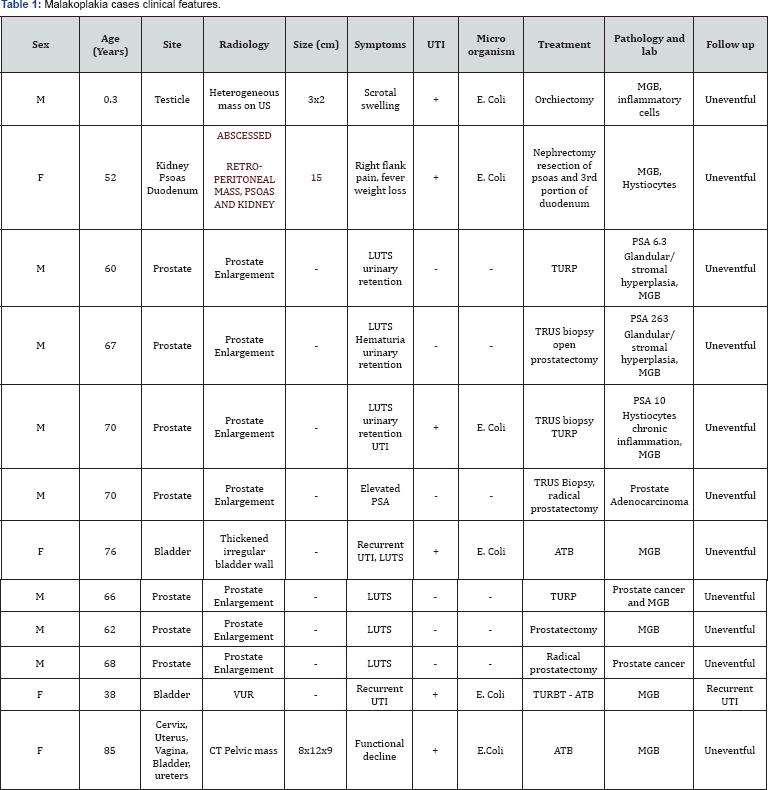
All structures in the urinary tract could harbor malakoplakia; Bladder is the most frequently affected organ, especially in females3the symptoms are hematuria and all others associated with UTI like frequency, hesitancy and dysuria. Those patients usually have repetitively positive cultures with E.coli, being the most frequent isolated organism. We had two cases with bladder MLP, the first is an usual case of an elderly patient with recurrent UTI, cystoscopy and biopsy was done and revealed MLP that responded adequately to conservative treatment with ATB. The second case occurred in a 38 years old female kidney transplanted patient who presented with recurrent UTI, cystogram revealed vesicourethral reflux (VUR) and cystoscopy showed yellow soft plaques with multiple foci affecting the bladder (Figure 1), biopsy showed MGB the patient received ATB, unfortunately symptoms recurred, at control cystoscopy we found larger lesions that required transurethral resection, pathologic examination confirmed the etiology. Outcomes were satisfactory with lower episodes of UTI after resection and continuous prophylactic ATB. Other structures can be affected by malakoplakia, Love et al. [10] described MLP of the urethra causing strictures and accounting as an exceptional etiology for this disease, surgery was not necessary in this particular case.
Malakoplakia has to be excluded in the differential diagnosis for neoplasia of the genitourinary tract. There is a special challenge in patients with scrotal masses, most of this patients end up having a radical orchiectomy because at ultrasound the mixed echotexture of the testis or epididymis is very difficult to differentiate from a testicular or epididymal malignancy [11]. It is well established that an enlarged mass in the testicle with suspicious ultrasound is an indication for surgery therefore the diagnosis of MLP of the testis is usually always done after conservative measures are not possible. Radical surgeries have been performed also for kidney MLP [12], prostate [9,13], ureter [14], urachus [15] and even for cervix, uterus and vagina [16] due to cancer misdiagnosis.
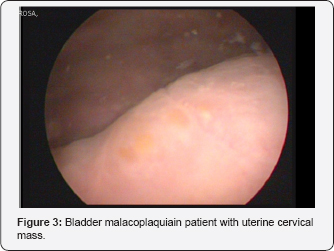
Our last case is quite interesting, this is an 85 years old women with recurrent UTI, functional impairment, asthenia and adinamia. Contrasted abdomen and pelvic CT evidenced a heterogeneous mass with necrosis foci measuring 8.2x12.8x9.4cm between the bladder wall and the uterus compromising the vagina and rectum (Figure 2). The clinical suspicion was for a cervix advancer tumor, biopsy revealed MLP, we performed additional cystoscopy were additional yellow plaques were encountered within the bladder (Figure 3) the pathologic analysis of this vesical lesions also revealed malakoplakia. ATB treatment was instituted with complete resolution of the lesion????.
There is a particular enthusiasm in the urology field about MRI in prostate cancer diagnosis, management and clinical decision-making. MRI technology is improving markedly by including functional sequences, diffusion-weighted imaging and dynamic contrast enhancement (DCE) coupled to a better image resolution that allows radiologists to discriminate more confidently potentially aggressive tumors [17]. Unfortunately even with these improvements, multiparametric MRI cannot differentiate between prostate cancer and MLP, the findings are low T2 signal intensity, diffusion restriction and hyper enhancement at DCE imaging for both pathologies [18]. None of our patients had MRI.
Our study has limitations, its retrospective nature. The inability to follow the patients up to date to know if other events presented and the impossibility to obtain complete documentation of the cases with leading imaging technologies.
Conclusion
Malakoplakia is a rare granulomatous disease that can affect the genitourinary tract, Urologists and Pathologists need to know main features of this differential diagnosis to avoid frequent confusion with neoplasia of the urinary tract.
References
- Tuzlali P, Igdem AA, Balci MBC, Yilmaz G, Sahan EC (2001) Themalakoplakia case which has beendiagnosedbyprostatetru- cutbiopsy: a case report. TurkishJournal of Urology 27(1): 98-100.
- Ali Z, Farouk K, Khan MA, Hanif S, Javed J (2010) Malako- plakia of the urinary bladder: a case report. Journal of Postgrad- uate Medical Institute 24(2): 165-167.
- Stanton MJ, Maxted W (1981) Malakoplakia: a study of the literature and current concepts of pathogenesis, diagnosis and treatment. J Urol 125: 139.
- Wagner D, Joseph J, Huang J, Xu H (2007) Malakoplakia of the prostate on needle core biopsy: a case report and review of the literature. Int J SurgPathol 15: 86e9.
- Michaelis L, Gutmann C (1902) Ueber Einschlusse in Blasentumoren. Zeitschriftfurklinische Medizin 47: 208-215.
- McClure J (1983) Malakoplakia. J Pathol 140: 275-330.
- Ali Z, Farouk K, Khan MA, Hanif S, Javed J (2010) Malako- plakia of the urinary bladder: a case report. Journal of Postgrad- uate Medical Institute 24(2): 165-167.
- Wielenberg AJ, Demos TC, Rangachari B, Turk T (2004) Malakoplakia presenting as a solitary renal mass. AJR Am J Roentgenol 183(6): 17031705.
- Velásquez López Juan G, Vélez Hoyos A, Uribe Arcila JF (2006) Malacoplaquia en urología: aportación de seis casos y revisión de la literatura. Actas Urológicas Españolas 30(6): 610-618.
- Love KD, Chitale SV, Vohra AK, Ball RY (2001) Urethral stricture associated with malacoplakia: a case report and review of the literature. Urology 57(1): 169.
- Kang YJ, Kim SW, Lee KS, Kim KH (2013) Malacoplakia of the Epididymis. Korean J Urol 54(4): 274-276.
- Tam VK, Kung W, Li R, Chan K (2003) Renal parenchymal malacoplakia: a rare cause of ARF with a review of recent literature. American Journal of Kidney Diseases 41(6): e13-17.
- Kahraman DS, Sayhan S, Diniz G, Ayaz D, Karadeniz T, et al. (2014) A Pit fall in Transrectal Prostate Biopsy: Malakoplakia Evaluation of Two Cases Basedon the Literature Review. Case Reports in Pathology 2014: 150972.
- Inoue T, Nishiyama H, Yoshimura K, Ito N, Kamoto T, et al. (2007) Solitary upper ureteral malakoplakia successfully diagnosed by ureteroscopic biopsy and treated conservatively. Int J Urol 14(9): 859861.
- Lnci O, Taştekin E, Gençhellaf H, Arabaci Ö, lşler S, et al. (2015) A Case of Urachal Malacoplakia that Seems Like Urachal Cancer. Balkan Medical Journal 32(1): 114-117.
- Chou SC, Wang JS, Tseng HH (2002) Malacoplakia of the ovary,fallopiantube and uterus: A case associated with diabetes mellitus.Pathol Int 52(12): 789-793.
- Scarpato KR, Barocas DA (2016) Use of mpMRI in active surveillance for localized prostate cancer. Urol Oncol 34(7): 320-326.
- Kitzing YX, Prando A, Varol C, Karczmar GS, Maclean F, et al. (2015) Benign Conditions That Mimic Prostate Carcinoma: MR Imaging Features with Histopathologic Correlation. Radiographics 36(1): 162175.






























