Single Stoma Tubeless Cutaneous Ureterostomy: A New Approach to an Old Operation
Arman A Tsaturyan1, Armine K Smith2, Tigran A Oganov3*, Arthur H Levonyan3, Armen A Muradyan1and Ashot A Tsaturyan3
1Departemnt of Urology, Yerevan State Medical University, Armenia
2Departemnt of Urology, Johns Hopkins University, USA
3Departemnt of Urology, Artmed Medical Center, Armenia
Submission: May 12, 2017; Published: May 23, 2017
*Corresponding author: Tigran A Organov, Department of Urology, Artmed Medical Center, Armenia, Tel: 37491414329; Email: oganov@hotmail.com
How to cite this article: Arman A Tsaturyan1. Single Stoma Tubeless Cutaneous Ureterostomy: A New Approach to an Old Operation. 2017; 3(1): 555603. DOI: 10.19080/JOJUN.2017.3.555603
Abstract
Introduction: Cutaneous ureterostomy is the simplest and safest way for incontinent urinary diversion associated with the lowest rate of early postoperative gastrointestinal and metabolic complications; however, its use is limited because of high rate of stomal stenosis, making ileal conduit the standard method for incontinent urinary diversion.
Aim: Present our technique of constructing single site tubeless cutaneous ureterostomy as a valid alternative to ileal conduit.
Patients and surgical method: Ten patients underwent the radical cystectomy followed by single stoma tubeless cutaneous ureterostomy. The main differences of our method from previously described techniques were the preservation of parietal peritoneum covering the ureters as a mean for better blood supply preservation and fixation of ureteral orifices one to another forming one oval shaped stoma.
Result: One out of ten patients experienced stricture of the stoma meaning requiring a reconstructive surgery on stoma. Other patients were free of obstruction at six month and 12-month period.
Conclusion:Cutaneous ureterostomy is a safe method, which is the preferred method of urinary diversion for morbid patients. We believe that modified single stoma tubeless cutaneous ureterostomy could become a method of choice not only for morbid patients but also for patients who are candidates for IC.Keywords: Ureterostomy; Chemotherapy; Lymph node; Stoma
Introduction
It has been reported that at the time of the diagnosis 30% of bladder cancers are already muscle invasive for which the treatment includes surgery and/or chemotherapy and/or radiation therapy. Currently, radical cystectomy with extended lymph node dissection remains a gold standard for local control of muscle invasive bladder cancer [1]. The surgery has a high incidence of both early and late complications, and most of those are associated with the type of urinary diversion [2-4]. In fact, continent urinary diversion is associated with higher risk of developing postoperative complications and should be performed in healthier patients. Currently, the simplest and safest way for incontinent urinary diversion is cutaneous ureterostomy; however, its use is limited because of the high rate of stomal stenosis, making ileal conduit the standard method for incontinent urinary diversion [5]. Conversely, cutaneous ureterostomy can reduce the rate of postoperative gastrointestinal and metabolic complications and is more time-saving [6] and thus may represent a better option for elderly patients with more morbidities. The aim of our paper is to present our technique of constructing single site tubeless cutaneous ureterostomy as a valid alternative to ileal conduit.
Patients and Surgical Methods
Ureterocutaneostomy is performed following cyst- prostatectomy among males and anterior exenteration among females with standard or extended lymph node dissection.
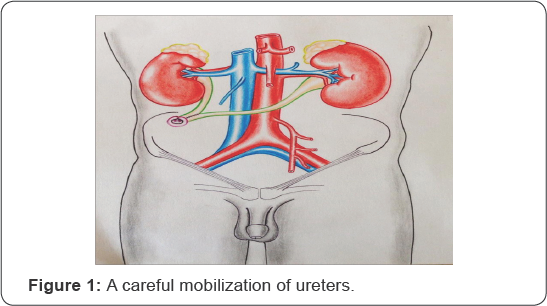
A careful mobilization of ureters is done to preserve sufficient peri-ureteric connective tissue, thus preserving adequate blood supply to the distal ends of the ureters. Stoma is generated at the right side. Skin excision is performed at the right side according to the ureter diameters, but not less than 1.5cm (Figure 1).
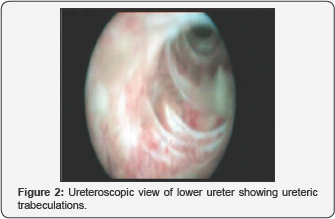
The fatty subcutaneous tissue is excised and a cross-like incision is made on the anterior rectus sheath. The rectus muscle is separated bluntly and a cross-like incision of the posterior rectus sheath and the peritoneum is performed on the tip of the underlying finger. Anterior and posterior rectus muscle sheaths are sutured together to fix the tunnel length. Both ureters together with preserved parietal peritoneum are pulled through without tension and distortion at least 1.5-2cm above skin level. The left ureter is directed to the right side via a retroperitoneal cavity above the mesenteric inferior artery. Both of the ureters are brought through in a completely extra peritoneal manner in all patients (Figure 2).
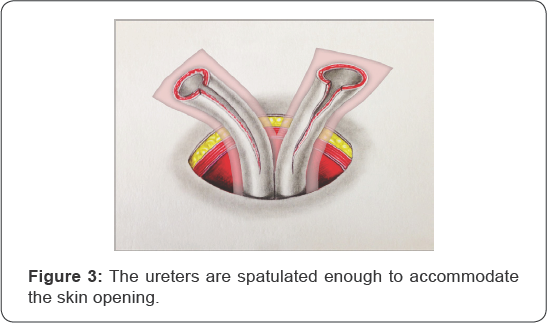
The ureters are spatulated enough to accommodate the skin opening. The parietal peritoneum is sutured and fixed to the formed tunnel wall using 4-0 Vicryl sutures (Figure 3).
The arterial capillary bleeding and spontaneous urinary jets are checked. The inside edges of the ureters are then conjoined in a side-by-side fashion using 4-0 Vicryl (Figure 4).
The outside (external) edge of ureteral flap reaches up a length of 1.0cm, whereas the inner edge of the ureteral flap is formed up to 2cm, which enables creating oval-shape stoma 1.0cm in size (Figure 4 & 5).

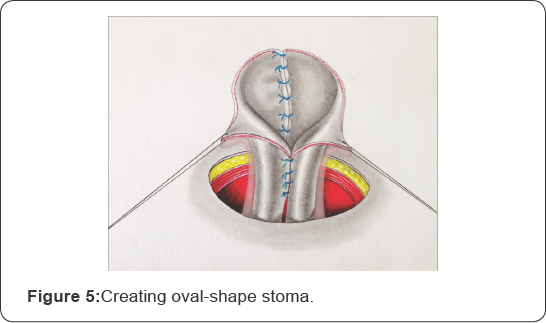
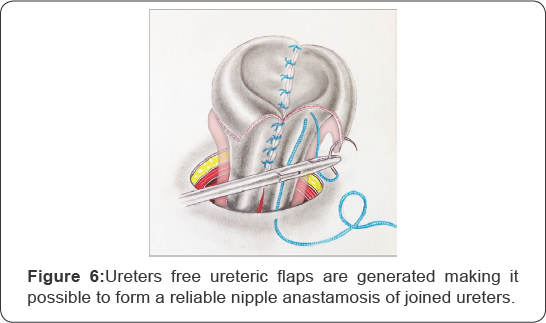
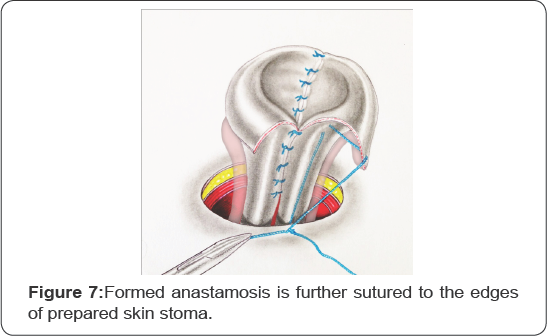
As a result of such conjunction of both of the ureters free ureteric flaps are generated making it possible to form a reliable nipple anastamosis of joined ureters. The formed anastamosis is further sutured to the edges of prepared skin stoma (Figure 5-7).
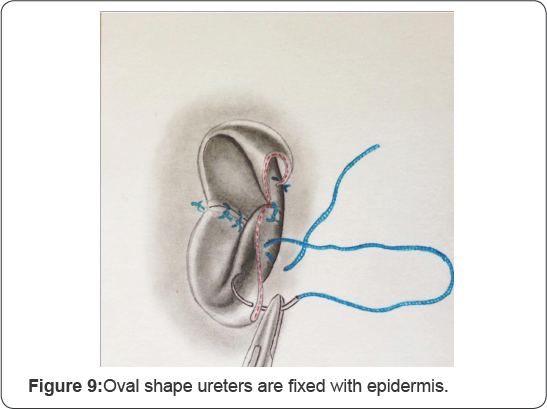
Oval shape ureters are fixed with 6-8 interrupted 5-0 PGA sutures to the aponeurosis and epidermis adapting everted cutaneous ureterostomy (Figure 8 & 9).

Two 6-French catheters are inserted and fixed to the skin, and a stoma bag is applied. Ureteric stents are removed 4 weeks following the surgery and the stoma gets its final appearance.
All patients received intra-operative antibiotic injection and subcutaneous low-molecular heparin starting on the day of surgery. All the surgical procedures were performed by a single expert surgeon.
In total 10 patients underwent modified technique of single stoma cutaneous ureterostomy in 2016. The advantages of existing urine derivation techniques were explained to all patients. All 10 patients gave their consent for the selected surgery. Six out of the 10 patients were clinically morbid patients and chose the method as a less morbid option, while others chose it because of advanced age. The surgery lasted from 150 to 240 minutes. There was no need for intra- or post-operative blood transfusion. No significant in-hospital complication was observed. Patients were discharged on the 8th day following the surgery.
Discussion
The present study shows a new technique of cutaneous ureterostomy with probable less stomal stenosis and higher catheter-free survival.
The use of cutaneous ureterostomy (CU) is limited due to formation of stomal stenosis and has been preserved for morbid patients. Nowadays, it is gaining its popularity with the increasing number of studies suggesting new approaches and comparing quality of life of those patients. Not only does CU represent the first and simplest urinary diversion following radical cystectomy, it does not require intestinal violation, minimizes the operating time and intraoperative blood loss, thus reducing postoperative complications. Another important issue among these patients is quality of life. A recently published article compared the quality of life of patients with CU and ileal conduit (IC). Interestingly, CU with single stoma was superior comparing the complications without any negative impact quality of life in comparison with IC [6]. This suggests that a well performed cutaneous ureterostomy could be used and even preferred as an alternative to IC.
Several approaches have been made and several techniques described to improve the outcome of CU. The first tubeless cutaneous ureterostomies were described by Ariyoshi and Toyoda in 1975 and 1977, respectively [78]. Ariyoshi et al. [7] reported that an everted ureteral nipple combined with triangular skin flap is essential for maintaining a tubeless ureterostomy, while Toyoda reported that firm fixation of ureters to the skin without a nipple formation is the key for permanent stoma [7,8]. Toyoda performed a longitudinal incision of the distal ends both of the ureters and sutured each edge of the ureter to the corresponding skin area. His results were satisfactory, though further modifications of the of the Toyoda's technique were published.
Terai et al. [9] further investigated the Toyoda's method of CU and presented their outcomes. Ninety-five patients had undergone the surgery with a catheter free rate of 82% at median follow-up of 23 months. They stated the need to sufficiently enlarge the abdominal wall tunnel and presented the following factor as a reason for failure in most of the cases [9]. Kim et al. [10] reported their results and emphasized the length of abdominal tunnel as one of the important factors. They applied Toyoda's technique with fixation of the anterior and posterior sheaths of rectus muscle and improved the catheter free rate from 60.5% to 89.9%. According to them, the main cause for postoperative stenosis was the compression of ureters in the abdominal wall, thus decreasing their blood supply and mechanically obstructing them [10]. We also believe that the length of abdominal tunnel plays an important role and therefore used the fixation technique for our cases. Unlike Toyoda's method and its modifications, our method involved a nipple formation similar to IC.
Wada et al. [11] described their technique for maintaining ureteral blood preservation. They implemented Ariyoshi's techniques and added that the fascia between spermatic cord and ureter, which was usually cut, played a significant role. They reported an improvement rate from 26% to 92% after applying the technique [11]. Another technique for improvement of ureteric blood supply was suggested by Lodde et al. [12] Unlike our technique, the stoma incision was performed on the left side and right ureter was brought to the left through mesosigmoid and sutured to the skin without nipple formation. In addition, the ureters were wrapped with the greater omentum supposing to improve their blood supply. With a follow-up varying from 6 to 24 months all 15 patients were without stents [12].
We personally think that careful dissection of the ureter with preservation of its blood supply and adequate formation of abdominal wall tunnel play key role in tubeless CU. In our initial experience, the results have been promising. All the patients to date are free from the catheters. The results will be more apparent with the increased number of patients and a longer of follow-up. ConclusionCutaneous ureterostomy is a safe method, which is the preferred method of urinary diversion for morbid patients. Its use is limited to those patients because of high rate of stoma site stenosis. Nevertheless, modifications of the technique are suggested by different authors for its improvement. We present our technique with promising results and believe that this could become a method of choice not only for morbid patients but also for patients who are candidates for IC.
References
- Witjes JA, Comperat E, Cowan NC, De Santis M, Gakis G, et al. (2014) EAU guidelines on muscle-invasive and metastatic bladder cancer: summary of the 2013 guidelines. Eur Urol 65(4): 778-792.
- Hollenbeck BK, Miller DC, Taub D, Dunn RL, Khuri SF, et al.(2005) Identifying risk factors for potentially avoidable complications following radical cystectomy. J Urol 174(4 Pt 1): 1231-1237.
- Konety BR, Allareddy V, Herr H (2006) Complications after radical cystectomy: analysis of population-based data. Urology 68(1): 58-64.
- Novotny V, Zastrow S, Koch R, Wirth MP (2011) Radical cystectomy in patients over 70 years of age: impact of comorbidity on perioperative morbidity and mortality. World J Urol (6): 769-776.
- Lee RK, Abol-Enein H, Artibani W, Bochner B, Dalbagni G, et al. (2014) Urinary diversion after radical cystectomy for bladder cancer: options, patient selection, and outcomes. BJU Int 113(1): 11-23.
- Longo N, Imbimbo C, Fusco F, Ficarra V, Mangiapia F, et al. (2016) Complications and quality of life in elderly patients with several comorbidities undergoing cutaneous ureterostomy with single stoma or ileal conduit after radical cystectomy. BJU Int 118(4): 521-526.
- Ariyoshi A, Fusijawa Y, Ohshima K, Hiratsuka Y, Sakamoto K (1975) Catheterless cutaneous ureterostomy. J Urol 114(4): 533-535.
- Toyoda Y (1977) A new technique for catheterless cutaneous ureterostomy. J Urol 117(3): 276-278.
- Terai A, Yoshimura K, Ueda N, Utsunomiya N, Kohei N, et al.(2006) Clinical outcome of tubeless cutaneous ureterostomy by the Toyoda method. Int J Urol 13(7): 891-895.
- Kim CJ, Wakabayashi Y, Sakano Y, Johnin K, Yoshiki T, et al. (2005) Simple technique for improving tubeless cutaneous ureterostomy. Urology 65(6): 1221-1225.
- Wada Y, Kikuchi K, Imamura T, Suenaga T, Matsumoto K, et al. (2008) Modified technique for improving tubeless cutaneous ureterostomy by Ariyoshi method. Int J Urol 15(2): 144-150; discussion 150.
- Lodde M, Pycha A, Palermo S, Comploj E, Hohenfellner R (2005) Uretero-ureterocutaneostomy (wrapped by omentum). BJU Int 95(3): 371-373.






























