Comparison of Volumetric Values of Transabdominal and Transrectal Ecosonography with Regard to Postoperative Prostatic Weight in Hyperplasia
Julio Jesus Gutiérrez Villalobos*
Department of Urology, Hospital Universitario, Ecuador
Submission: February 14, 2017; Published: April 24, 2017
*Corresponding author: Julio Jesus Gutiérrez Villalobos, Department of Urology, Hospital Universitario, Ecuador, Tel: 0291-635-4450; Email: juliojgv@hotmail.com
How to cite this article: Julio J G V. Comparison of Volumetric Values of Transabdominal and Transrectal Ecosonography with Regard to Postoperative Prostatic Weight in Hyperplasia. JOJ uro & nephron. 2017; 2(5): 555598. DOI: 10.19080/JOJUN.2017.02.555598
Abstract
For the purpose of comparing the values of the volumetric transabdominal Echosonography on the weight transrectal prostate postsurgical patients with benign prostatic hyperplasia University Hospital "Dr. Manuel Nunez Tovar”, Maturin November 2011- February 2013, we conducted a prospective, cross-sectional comparison of 65 patients diagnosed with BPH requiring surgery. Data were collected including age, PSA value, prostate volume by transrectal and abdominal ecosonography prostate weight after surgery, getting some by review of medical records and the other for the realization of both methods ecosonography and prostate weight after extraction. We analyzed the data obtained; the age group with the highest incidence was between 60 and 80 years (85%). No correlation was found between age and the PSA value in these patients and was found that there was a moderate correlation between the values of abdominal and transrectal Echosonography with PSA. We conclude that there is a high correlation between both methods ecosonography and actual prostate weight values.
Keywords: Benign prostatic hyperplasia; Ecosonography; Transrectal ecosonography; Transabdominal postsurgical weight; PSA
Abbreviations:BPH: Benign Prostatic Hyperplasia; PSA: Prostate-Specific Antigen; TURP: Transurethral Resection of the Prostate Gland; LUTS: Lower Urinary Track Symptoms; SPSS: Statistical Package for the Social Sciences; PSA: Prostate Specific Antigen
Introduction
Benign prostatic hyperplasia (BPH) is one of the most frequent pathologies of the males. Characterized by a chronic and progressive growth of the prostate gland, causing a blockage of the outflow of urine, clinically manifesting itself in so- called lower urinary tract symptoms. In more advanced stages the obstruction of the flow can become chronic, appearing complications such as acute retention of urine, infection or kidney failure. In addition, patients may require surgery due to the disease itself or by any of the complications. [1].
Prostate-specific antigen (PSA) is a protein belonging to the family of kallikreins serum. It may be caused by the normal prostate epithelial cells and hyper plastic, malignant, the function in the body is the lisar the I clot seminal, can be carried in the blood due to rupture of the biological barriers that separate the prostate of the blood one of the causes of this break down is the increase in the number of ductal epithelial cells determined by benign prostatic hyperplasia (BPH) [2,3].
Nowadays can consider is the ultrasound abdominal as the technical of image of choice initial in study of the patient that consultation by a syndrome of prostatism. Identifies the practical totality of morphological anomalies induced by BPH in upper urinary tract and the lower, although the display of the first also has been considered optional; in our view, the comprehensive ultrasound of the urinary tract is a very economical method and not invasiveness and implementation is systematically advisable, all less in the initial evaluation. The via abdominal offers enough resolution for know the volume and the form of growth of the BPH, Finite book the transrectal for them stealthy of detection early of the cancer, touch rectal doubtful or PSA greater to 2.5ng/ml [4]. The handling and treatment of the BPH is varied the conduct expectant is an option in those with symptoms minimum and Sin complications associated.
The pillar of the handling medical is the treatment with blocking of receptors alpha, which relax the stroma of the muscle smooth prostate and them inhibitors 5-reductase, which reduce the volume prostate [5]. The surgery is indicated when there is an increase in the symptoms attributable to symptoms of the tract urinary lower (LUTS) others complications of BPH. Transurethral resection of the prostate gland (TURP) is an established surgical practice. The prostate glands with volumes greater than 100 grams are often treated with open prostatectomy, primarily by concern of bleeding and improper fluid absorption. The vaporization photo selective of the gland prostate via Transurethral, using the laser «KTPYAG» (06) or the technical of enucleation with laser of holmium are emerging as an alternative surgical attractive even for large volumes prostate (07).
This study aims to compare the transabdominal misleading volumetric accuracy vs. the transrectal misleading in relation to the weight of the visited after prostate. Arises aims, compare both studies ultrasound with post-surgical prostate weight and distinguish with statistical precision single use of transabdominal ultrasonography in the diagnosis of BPH.
Material and Methods
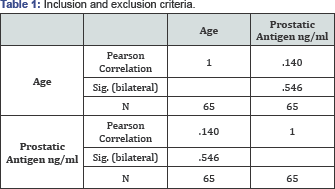
Study was conducted a prospective, comparative, cross section with approval by the Committee of ethics of our institution. A total of 65 patients, recruited aged between 40 and 79 years of age, who met the criteria for inclusion (Table 1) and under informed consent to accept such a study. In all the patients are documented the exploration clinical (touch rectal), values volumetric of ECOAB and ECOTR and weight postsurgical expressed in grams. The measurement by transrectal ultrasonography (ECOTR) prostatic diameters were recorded in the transverse and sagittal planes on the maximum length of the same. We use a Hitachi CS-200 ecosonography with transrectal transducer 7 MGHZ models, getting the images with the patient in left lateral decubitus. Volume was calculated by the software built into the ultrasound with the formula of the ellipsoid, whereas in the transverse plane in its maximum dimensions width (transversal diameter) and height (antero-posterior diameter) and in the sagittal plane, from the base to the apex, the maximum length (diameter cefalo-flow) [8]. All determinations were performed by the same examiner who in turn was the surgeon. We recorded the total prostate volume of 65 patients who were diagnosed with BPH and subsequently underwent an open prostatectomy. All the determinations were done by a same examiner that at its time was the surgeon. We recorded total prostatic volume of 65 patients who were diagnosed with BPH and subsequently undergoing Prostatectomy open or endoscopy. The values are correlated using the method of Pearson. Considered the value of p<0.05 the cut-off point to set as statistically significant differences. Both measures are compared with the surgical specimen weight, assuming that the specific weight of the prostate is equal to 1 (the volume in cubic centimeters (cc.) is equivalent to the weight in grams (g).
After the data analysis used statistical methods which are more adapted to the needs of the study. The data were processed by Statistical Package for the Social Sciences (SPSS) version 15.0 for Windows and were plotted with the use of Microsoft Excel 2007.
Inclusion and exclusion criteria inclusion
a. Inclusion
o Patients greater of 40 years of age with diagnosis of hyperplasia prostate benign.
o Patient with updated PSA.
o Patient with diagnosis of syndrome obstructive low.
b. Exclusion
o Patients with signs and symptoms of prostatism inconclusive for benign prostatic hyperplasia [9].
o Patients with prostate cancer.
Results
Result 1
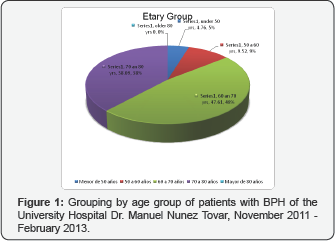
A total of 65 patients were enrolled in this study after applying the criteria of inclusion and exclusion. They were classified by age groups and it was observed that 5% (n=3) were under 50 years of age, 9% (n=7) between 50-60 years, 46% (n=30) between 60-70 years, 38% (n=25) between 70-80, 0% (n=0) over the age of 80 [10] (Figure 1).
Result 2
After correlating the ages of them patients with them values blood of the Antigen prostate specific (PSA) is observed a coefficient of correlation of Pearson of 0.14 (p>0.05) (Table 1).
Result 3
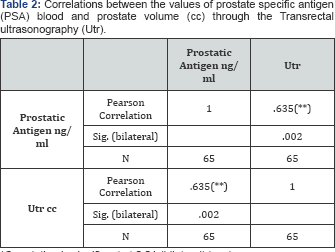
After obtaining the prostatic volume in patients with BP by transrectal ultrasonography and prostate Antigen (PSA) blood values was observed a correlation coefficient of Pearson between both variables of 0.635 (p<0.05) [11] (Table 2).
*Correlation is significant at 0.01 (bilateral) level.
*Correlation is significant at 0.01 (bilateral) level.
Result 4
To obtain the prostatic volume through the transabdominal ultrasonography and also relate to the values of prostate-specific antigen (PSA) was observed a correlation coefficient of Pearson between both variables of 0,631 (p<0.05) [12] (Table 3).
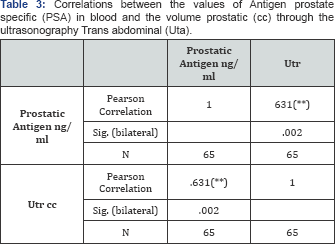
* The correlation is significant at the level 0.01 (bilateral). Source: Table of data collection
Result 5
After get the weight prostate back to the Prostatectomy in each patient, is compared with the volumes prostate obtained through the ultrasonography transabdominal and transrectal. Is observed a coefficient of correlation of Pearson between the weight postsurgical and the volume prostate through the ultrasonography transabdominal of 0,881 (p<0.05) and of 0.928 (p<0.05) with the ultrasonography transrectal (Tables 4 & 5) [13].
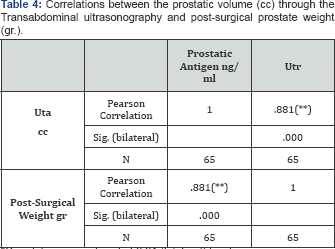
*Correlation is significant at 0.01 (bilateral) level.
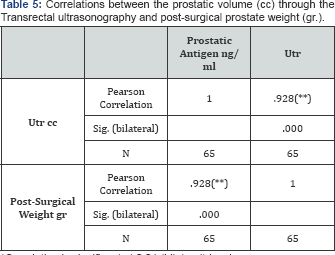
*Correlation is significant at 0.01 (bilateral) level.
Discussion
The BPH is the tumor benign more often of the male. The age of start is between the fourth and to the fifth decade of her life. The growth of the prostate is slow or non-existent to them 30 years, when starts to increase of size. This growth is more pronounced from age 50. 80% of those older than 50 years have, in greater or lesser extent, BPH, so 33% of those older than 50 years already present a well-structured adenoma. At the age of 80-95% has HBP. It has been estimated that the probability that a man of 80 years of life need Prostate Surgery is 30% [14]. The prevalence of the HPB in Venezuela is of 85% in men over 80 years of age, 65% in the group age of 61-80 years and of 50% in the Group of 50 to 60 years, according to data supplied by July Caesar Potenziani, urologist of the «Hospital private Center doctor in Caracas» [15]. Most of the patients included in our study have aged between 60 and 80 years (86%), age at which it is advisable to annually undergo Antigen and rectal touch the prostate as a preventive method in BPH and prostate cancer. The value of the PSA serum is associated both with the age as with the size of the gland. Babain and col. correlated serum PSA with age and prostate volume, the latter determined by transrectal ultrasonography. They calculated that the value of the PSA increases 45% per decade. Patients young, minor of 50 years had values serum of PSA of 4ng/ml or less, also showed that the PSA is increased with the size of the gland prostate, increase that was of the 38% by cm3. The same conclusion reached Nadier et al. in his studio in Missouri, USA, in 1995 where 148 patients were studied.
Hatch and cols. evaluated them levels of PSA by ages, obtaining an increase progressive of these values, corresponding them major figures to those patients with more than 70 years [16]. On the other hand, Sanchez in evaluating the importance of studies for the diagnosis of prostate cancer, concerned that the age is the number one for prostatic diseases risk factor, since 50 years the possibility of prostate cancer or BPH increasing rapidly, since more than 80% of the cancer prostate are diagnosed past age 65, while it is rare that this disease occurs in under 50 years of age. Oesterling and cols, told a study population where those levels blood of PSA suffer strong influence by the age, increasing as more elderly is the individual population. Like Babain and cols, Ana Zevallos, conducted his research work carried out in Lima, Peru, the correlation between the serum PSA levels with age and prostate volume [17]. Studied 100 patients who came to the National Hospital Almanzor Aguinaga Asenjo-Lambayeque, where these patients PSA blood values were correlated with age and prostate volume, prostate sizes were categorized as <30g, 30-39gr, 40-59g and 60g, with an average value of PSA's 4.35, 4.38, 15.24, 6.9ng/ml respectively [18]. Parametric correlation of Pearson to age versus prostate volume (r=0.4520). While all patients included in our study had diagnosis of BPH failed to show a statistically significant correlation between age and serum PSA values [19]. Probably this is because not there was variety of groups age since it most of them patients (85%) have ages understood between 60 and 80 years.
Zevallos present data where it was clearly observed a progressive increase in blood levels of PSA, influenced by the prostate volume [21]. Ercole and cols and Ferrero and cols [15,16], found PSA elevated in 24% and 33% of confirmed cases of BPH, respectively [15,16,22]. According to Weber et al. PSA correlates better with epithelial weight that with prostate weight and may be variation of up to 3 times in the epithelial contribution to prostate weight [23]. This indicates that the main factor influencing the elevation of PSA in patients with BPH is the histological composition if same, mainly its epithelial content. While our work considers only patients with symptoms that I require surgery and not to asymptomatic patients, we can say that the alterations found in serum PSA levels have great similarity. According to our results, there is a correlation moderate between obtained by misleading transrectal prostatic volume and PSA. Is observed a coefficient of correlation of Pearson between these variables of 0.635 (p<0.05). Same results by correlating values of prostate volume obtained by abdominal misleading and PSA where a coefficient of Pearson correlation between two variables of 0.631 was observed (p<0.05). The correlation of both methods with the PSA is moderate and statistically significant.
Comparisons between the volumes estimated by ECOTR and the actual weight of the surgical specimen were established in other series published in the literature. Zlotta et al. (1999), found a good correlation (0.95) between the estimated volume of the zone of transition (ZT) and weight of énucléé adenoma, while the difference between the estimated average volume and the average weight of adenoma was not significant (p=0.07) [24-28]. Total prostatic volume and the weight of the piece of prostatectomy, these authors found a somewhat weaker correlation (0.78), with significant differences between the average prostate volume and the average weight of the piece (p<0.001). His work concludes that the estimation of the volume of the ZT is a secure parameter in the management of patients with BPH. For Milonas (2003), in a similar study with 120 patients, there is a good correlation between the volume of the ZT and the weight of énucléé adenoma (0.94), in 30 patients who underwent surgery. Finding no significant difference between the volume estimated medium and the average weight of the adenoma (p=0.6) [29]. Balatac (2000) is also a good (0.95) correlation between the volume of the ZT and the weight of the piece, but with a significant difference between volume and weight (p<0.001) [30]. Blaming this difference and its apparent contradiction with Zlotta, to difficulties in measurement of the ZT or incomplete enucleation of the adenomatous tissue during surgery. In their conclusions, they maintain that although the estimate of the volume of the ZT is useful in the clinic, methods for their measurement, it must agree to make it more accurate.
According to our results, measurements made by abdominal misleading and transrectal misleading shows a high correlation with post-surgical prostate volume, with a correlation coefficient of 0.881 (p<0.05) for the abdominal and 0.928 (p<0.05) with transrectal ultrasonography. This shows that the correlation between both methods is very strong and statistically significant, we therefore consider that the supra pubic method can be a reliable alternative for accurate diagnosis of BPH, compared to the ECOTR, where it is uncomfortable and embarrassing, especially in patients with diseases Annals. In accordance with our findings, Prassopoulos and cols, also reported a strong correlation between the ultrasound transrectal and the supra pubic in the measurement of the volume prostate [16,31]. Yuen and cols. (2002), found that the measurement of the volume prostatic transabdominal had a good correlation with the measurements carried out by ultrasound transrectal and therefore, not had need of ultrasound transrectal uncomfortable [32-34]. We showed a correlation very strong between the measurements of volume carried out by misleading supra pubic and transrectal.
Conclusion
We studied patients who attended the consultation of Urology at the «Manuel Núñez Tovar University Hospital Dr.» aged between 40 to 80 years, with increased incidence of BPH age group was between 60 and 70 years. There is a direct relationship between age and the value of prostate-specific antigen in patients with BPH. Estadísticamente, existeuna correlation moderate between the volume prostatic retrieved through the misleading transrectal and abdominal and the value of PSA. Both ecosonograficos methods have proved effective for the measurement of the prostate volume by the high correlation between the values obtained through the abdominal and transrectal ultrasonography and prostate weight postoperative. Not there is difference statistically significant in the correlation between the values of the ultrasonography transabdominal and transrectal with the weight prostate postoperative. He employment of the ultrasound has eased significantly the evaluation of the BPH, helping to determine the volume prostate with more precision that others explorations and to objectify the practice all of anomalies morphological of the tract urinary induced by this disease. The ultrasound transabdominal is the technical of choice initial in the study and follow-up of patients with BPH. The transrectal via will be indicated at the suspicion of cancer, rectal suspicious and/or elevation of PSA the supra pubic image is of poor quality or for specific clinical protocols.
References
- Abad M, Zuluaga G, Espuela O (1996) Current state of prostatic ultrasound. Urol lnteg Invest 1: 257.
- Barry MJ, Fowler FJ, O'Leary MP, Bruskewitz RC, Holtgrewe HL, et al. (1992) The American Urological Association Symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol 148(5): 1549-1557.
- Blanes M, Velázquez G, Cabral M (2005) Reference values of prostate specific antigen. Mem Inst Invest Cienc Salud 3(1).
- Cabello B, Rascón J, Monzó J, López I, Subirá D, et al. (2006) Correlación ecográfico-anatómica de la medición del volumen prostático total y de la zona transicional mediante ecografía transrectal. Actas Urol Esp 30(2): 175-180.
- Debruyne F (2004) Efficacy and safety of long-term treatment with the dual 5 alpha-reductase inhibitor dutasteride in men with symptomatic benign prostatic hyperplasia. Euro Urol 46(4): 488-495.
- Tanagho EA, McAninch JW (2005) General urology of Smith. (13th edn), Editorial El Manual Moderno, Mexico.
- Herranz F, Verdú F, Salamanca J (2006) Cáncer De Próstata Y Ecografía Transrectal. Arch Esp Urol 59(4): 361-375.
- Granados E, Chechile G, Villavicencio H (1991) Agonistas LH-RH como alternativa terapéutica en pacientes con hiperplasia benigna de próstata (HPB) y contraindicación quirúrgica. Seguimiento a largo plazo. Arch Esp Urol 49: 923-937.
- Jimenez C, Resel E (1994) Informe sobre nueva terapéutica de la hiperplasia benigna prostática. Actas Urol Esp 17: 629.
- Kim S (2005) Imágenes en urología. (1st edn), Editorial Medica Panamericana, Argentina.
- Kim SH, Kim SH (2008) Correlations between the Various Methods of Estimating Prostate Volume: Transabdominal, Transrectal and Three-Dimensional US. Korean J Radiol 9(2): 134-139.
- Kirby RS (1998) Revisión de las Enfermedades Prostéticas; Atlas de enfermedades prostáticas. TG Hostench 1: 12-24.
- McConell JD (1995) Diagnóstico y tratamiento de la hiperplasia prostática benigna. Practical cases in urology. Practical management of BPH. American Urological Association. Inc. Office of Education, pp. 45-57.
- Martínez S, Pedro (1998) Hiperplasia prostática benigna: fisiopatología, clínica y tratamiento no invasivos. BoletEsc de Med UnivCat de Chile 27: 84-88.
- Mayayo D, Rivas E, Galmes B, Cols Y (1995) Posibilidades de la Ecografía en los Algoritmos Diagnósticos Urológicos. Arch Esp Urol 48: 665.
- Mayayo D, Maganto P, Lovaco C, Cols Y (1981) Estudio ultrasonográfico de la próstata normal y patológica. Actas Urol Esp 5(4): 227232.
- Mayayo D (1993) Estudio ultrasonográfico del aparato urogenital. Tratado de Urología. Barcelona, pp. 213.
- Mayayo D (1993) Ecografía transrectal y cáncer de próstata: visión personal. Arch Esp Urol 46: 755.
- Edward M, Vikram D, Judd B (2006) Ecografía transrectal en la evaluación de la próstata. RadiolClin N Am 44. 679-687.
- Milonas D, Trumbeckas D, Juska P (2003) The importance of prostatic measuring by transrectal ultrasound in surgical management of patients with clinically benign prostatic hyperplasia. Medicina 39(9): 860-866.
- Morote R (1991) Comportamiento del antígeno prostético específico en población sana: valoración de su especificidad. Antígeno prostético específico. Enard Fabregat pp. 79-86.
- Navas R, Mayayo E, Funez F, Rodriguez R, Mayayo D (2006) Diagnóstico y seguimiento de la hipertrofia prostática benigna mediante ecografía. Arch Esp Urol 59(4): 353-360.
- Wasserman F (2006) Hiperplasia benigna de la próstata: revisión y clasificación ecográfica. RadiolClin N Am 44: 689-710.
- Ozden E, Gogus C, Kilic O, Yaman O, Ozdiler E (2009) Analysis of Suprapubic and Transrectal Measurements in Assessment of Prostate Dimensions and Volume. Urol J 6: 208-213.
- Potenziani, Julio C (2001) Enfermedades de la próstata. (1st edn), Caracas Editorial Ateproca.
- Rodríguez, Baluja M, Bermudez Senia I (2007) Patologías benignas de la próstata: prostatitis e hiperplasia benigna. Rev Biomed 18: 47-59.
- Romero C, Mayayo D, Cols Y (1980) Evaluation comparative del volumen prostatique par l'ecographie transabdominale, le profil uretral et la radiologie. J D'Urologie 86: 675.
- Salina J (1993) Los estudios urodinámicos en la valoración de la hipertrofia prostática benigna. Monografía del LVIII Congreso Nacional de Urología: tratamiento quirúrgico de la hipertrofia benigna de próstata pp. 43-57.
- Schwartz S, Shires T, Spencer F, Daly J, Fisher J, et al. (2000) Principios de Cirugía. (7th edn), Editorial McGraw Hill, Mexico.
- Paul S, Grant B (2009) Ultranosido del sistema urogenital. (1st ed.), Editorial Amolca, Colombia.
- Varela M, López Y, Lopez J, Fasanella H (2000) Antígeno prostético específico y su densidad en el diagnóstico de la hiperplasia prostática benigna y del adenocarcinoma de la próstata. GacMéd Caracas 108(3): 315-330.
- Vinaccia S, Fernández H, Sierra F, Monsalve M, Quiceno J (2007) Diseño de un cuestionario psicométrico para evaluar creencias, actitudes y conocimientos asociados a la hiperplasia prostática benigna. Suma Psicológica 14(1): 73-92.
- Wein K, Novick P (2009) Campbell -Walsh Urologia. (9th edn), Argentina: Editorial Medica, USA.
- Martha BZ, Carvajal Errol (2006) Hipertrofia Prostática. Rev Paceña MedFam 3(4): 74-77.






























