Prevention of the Development of Diabetes by Early Intervention
Vinod C Tawar*
Manchanda Medical Clinic, Surrey, British Columbia, Canada
Submission: March 11, 2017; Published: April 04, 2017
*Corresponding author: Vinod C Tawar, Department of Pharmaceuticals, Manchanda Medical Clini, Canada, Email : tawar.vinod@yahoo.com
How to cite this article: Vinod C T. Prevention of the Development of Diabetes by Early Intervention. JOJ uro & nephron. 2017; 2(3): 555587.DOI:10.19080/JOJUN.2017.2.555587
Abstract
The current research, a retrospective study on early stage intervention on the development of diabetes is based on a concept discussed in 2011 by Ralph A De Fronzo and Muhammad Abdul-Ghani in a publication by American Diabetes Association.
The Research comprises of early recognition of the patients at the stage of developing IGT and initiation of treatments with oral hypoglycaemic agents in order to reach a normal HbA1C. The overall number of patients in practice were 5000. And those with IGT were 26. The research was started 7 years ago and has resulted in these patients reaching a HbA1C of 5.2. The target of treatment was maintaining lower than 5.2.
Metformin has been mostly effective in patients reaching the target value. However, in rare cases Gliclazide was needed. In one Case Acto's and Insulin treatment was essential for a female patient with Polycystic Ovarian Syndrome. The current success has resulted in preventing further complications from diabetes.
In earlier years clinical were advised to start oral hypoglycaemic agents, once the patients had shown a HbA1C of 7.5. However, the evidences have shown that by this stage many complications from diabetes would have occurred.
Keywords: Oral hypoglycaemic agents; Pre-Diabetics; Metformin
Introduction
There has been a dilemma among clinicians as to when to initiate the oral hypoglycaemic agents (OHA) following non pharmacological approaches e.g. diet, exercise and weight loss. Earlier understand was that the medications can be started after the patient had reached a HbA1C value of 7.5. Current Canadian Guideline are HbA1C of 6.1 being in normal range and those with HbA1C of 6.2-6.5 are considered "Pre-Diabetics" or with IGT. As explained in the article by De Fronzo, et al. [1]. Initiation of treatment with appropriate OHA prevents the development of a full blown diabetes. If the clinicians wait until the patient reaches the HbA1C of 7.5, many complications from diabetes already are existing. My experience dates back to approximately 10 years when a patient of mine with HbA1C of 6.9 was started on metformin and subsequently switched to Gliclazide for effective prevention.
Past Investigations
De Fronzo, et al. [1] had established a link between insulin resistance, diabetes, obesity, hypertension, dyslipidaemia and ASSCVD in 1991. Cusi in collaboration with De Fronzo reviewed the metabolic effects of metformin in 1998 [2].
Subsequently, UKPDS Group had focussed on the intensive glucose control with sulfonylurea or insulin and the risk of complications in the patients with Type 2 diabetes in 1998 [3,4]. Later, UKPDS group advanced their research to metformin use with similar objectives. Turner, et al. [5] in 1999 investigated the role of diet, sulfonylurea, metformin or insulin treatment in patients with Type 2 diabetes in conjunction with UKPDS [4,5].
Knowler, et al. [6] in 2002 emphasized on the reduction in the incidence of Type 2 DM with life-style interventions. Abdul-Ghani in 2006 studied the risk of progression to DM by establishing a relationship between post-load plasma glucose and fasting plasma glucose [7]. Holman, et al. [8] reviewed a 10 year follow-up study with intensive glucose control in Type 2 DM. Eriksson, et al. [9] in 2008 emphasized on the significance of diet and exercise in the prevention of Type 2 diabetes. Lastly, Vendetti, et al. [10] in 2008 investigated the role of lifestyle interventions and weight loss.
Method
My current study of diabetes prevention is based on identification of PRE-DIABETICS among a population of 5000 patients. These patients with HbA1C of more than 6.2 were given a starting does of Metformin of 250mg after their evening meal. There was an equal proportion males and females. A total number of 29 patients were identified in the "pre-diabetics" group. They were offered counselling for the diet, lifestyle interventions and followed by lab investigation after one month. If there was no change in HbA1C the patient was offered Gliclazide 15mg with their evening meal and lab monitoring was continued. The patient identified 10 years ago has a history of sinus arrhythmia and suffers from hypercholesterolemia. He has been maintaining a normal HbA1C like other 28 patients with a low dose of OHA and controlled heart disease. It was commonly observed that one to two months of OHA was sufficient for the patient to reach HbA1C of 6.2 or less, provided the treatment was continued. This approach showed the prevention of further complications from diabetes e.g. hyperlipidemia or renal dysfunction.
The likely contribution factors to IGT indentified were family history, obesity, pancreatitis, alcoholism, gestational diabetes or viral diseases. The age of onset was observe between 40 and 50 years.
Results
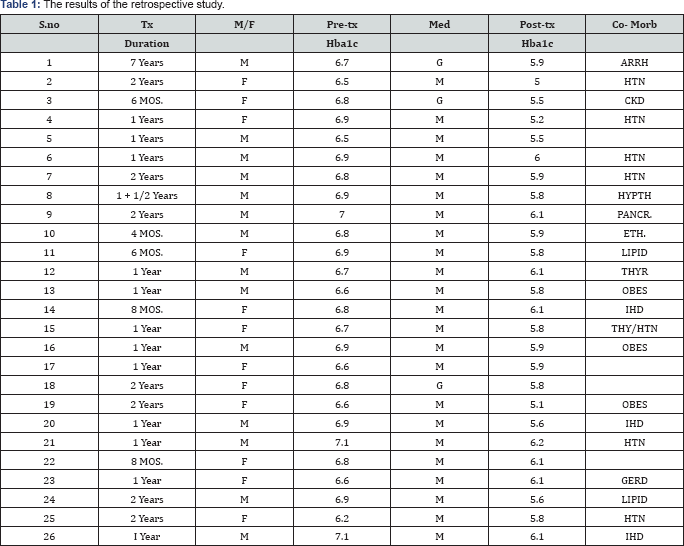
The results of the retrospective study are listed in the enclosed Table 1.
Conclusion
Early prevention of patients from developing diabetes was achieved by commencing treatment with either Metformin or Gliclazide. Two of my patients observed having a normal HbA1C in the absence of and OHA after a short term initial medical management while others maintained a normal HbA1C with a small dose of OHA with continuation. The patients have been free of any other co-morbidities e.g. CKD or CVD.
References
- De Fronzo RA, Ferranini E (1991) Insulin resistance a multifaceted syndrome responsible for NIDDM, Obesity, Hypertension, Dyslipidemia and ASCVD. Diabetes Care 14(3): 173-194.
- Cusi K, De Fronzo RA (1998) Metformin: A review of it's metabolic effects. Diabetes Res 6: 98-131.
- 3. UKPDS group (1998) Intensive glucose control with Sulfonylurea or Insulin compared with conventional treatment and risk of?complications in patients with Type 2 Diabetes. Lancet 352(9131): 837-853
- UKPDS group (1998) Effect of intensive blood control with Metformin on complications in patients with Type 2 DM (UKPFD34). Lancet 352(9131): 854-865.
- Turner RC, Cull CA, Frighi V, Holman RR (1999) Glycermic control with diet Sulfonylurea, Metformin or Insulin in patients with Type 2 DM. JAMA 281(21): 2005-2012.
- Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, et al. (2002) Reduction in the incidence of Type 2 DM with life style intervention or metformin. N Engl J Med 346(6): 393-403.
- Ghani A, Williams K, DeFronzo R, Stern M (2006) Risk of progression to DM on relationship between post load plasma glucose and fasting plasma glucose. Diabetes Care 29(7): 1613-1618.
- Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA (2008) 10 year follow-up of Intensive glucose control in Type 2 DM. N Engl J Med 359(15): 1577-1589.
- Eriksson KF, Lindgarde F (1991) Prevention of Type II DM by diet and exercise" The 6 year Malmo feasibility study. Diabetelogia 34(12): 891898.
- Vendetti EM, Bray GA, Carrion-Petersen ML, Delahanty LM, Edelstein SL, et al. (2008) First versus repeat treatment with lifestyle intervention program: attendance and weight loss outcomes. Int J Obes 32(10): 1537-1544.






























