Late, but Before Schedule-A Bigeminal Rhythm with Blocked Premature Junctional Beats
Daniel Manna1, Thomas Lindow1,2* and Olle Pahlm2
1 Department of Clinical Physiology, Växjö Central Hospital, Växjö, Sweden
2 Department of Clinical Sciences Lund, Lund University & Clinical Physiology, Skåne University Hospital, Lund, Sweden
Submission: June 12, 2019; Published: July 05, 2019
*Corresponding author: Daniel Manna, Department of Clinical Physiology, Växjö Central Hospital, Växjö, Sweden
How to cite this article:Daniel M, Thomas L, Olle Pahlm. Late, but Before Schedule-A Bigeminal Rhythm with Blocked Premature Junctional Beats. J Cardiol & Cardiovasc Ther. 2019; 14(1): 555880. DOI: 10.19080/JOCCT.2019.14.555880
Abstract
Premature supraventricular ectopic beats are common findings in ambulatory ECG monitoring. Blocked ectopic beats may occur if the premature beat coincides with the refractory period of the downstream conductive tissues. We report of an uncommon, symptomatic bigeminal rhythm which resulted in an abrupt decrease of the heart rate because of blocked P waves. The blocked P waves appeared uncommonly late in the cardiac cycle because of a very His-near activation site. For anatomic reasons treatment was difficult and the patient received a pacemaker.
Keywords: ECG; Blocked extrasystoles; Bradycardia; Ambulatory ECG monitoring
Abbrevations: PJCs: Premature Junctional Contractions; PACs: Premature Atrial Contractions; EPS: Electrophysiological Study
Learning Objective
Blocked premature junctional or atrial beats can result in symptomatic bradycardia. A blocked P wave beyond the refractory period of the ventricular conduction tissue may suggest an AV-nodal or His-near activation site.
Background
Premature supraventricular ectopic beats are common findings in ambulatory ECG monitoring. Blocked ectopic beats occur when the premature beat appears during the refractory period of the downstream conductive tissues. We describe a rarely occurring bigeminal rhythm which resulted in an abrupt decrease of the heart rate because of blocked P waves, which appeared late in the cardiac cycle, but were still not conducted.
Case Presentation
A 63-year old lady was referred for ambulatory ECG monitoring by her general practitioner. She had no history of cardiac disease but since several months she was experiencing palpitations. A beta blocking agent had been tried but was discontinued due to symptomatic bradycardia. Lately she had also experienced dizziness, in addition to palpitations, especially at rest. Most of her symptoms were alleviated during light exercise such as walking.
ECG analysis
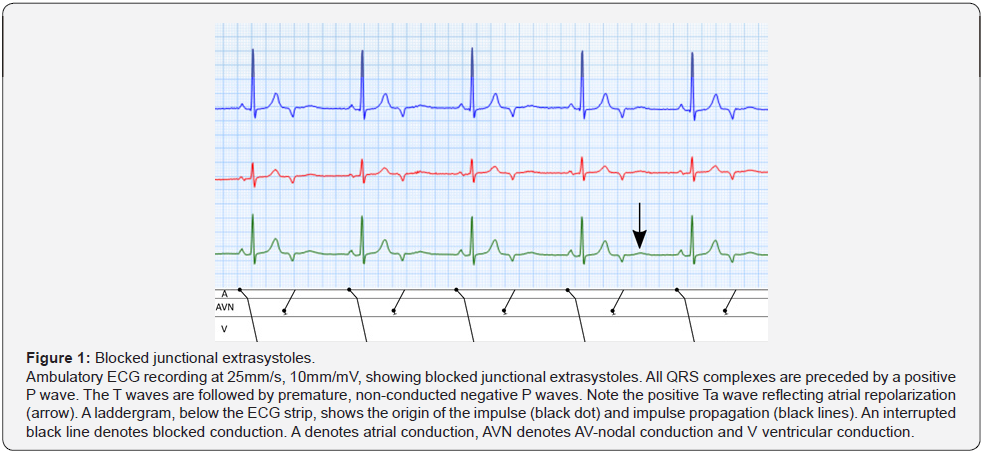
Resting ECG at the time of ambulatory ECG monitoring was normal. The 48-hour ambulatory ECG recording showed a large number of supraventricular (~17%) and ventricular (~5%) extrasystoles. Most of the supraventricular extrasystoles had similar P-wave morphology, suggesting a single origin. At night and during rest, multiple episodes (~15 seconds each) of decreased heart rate were noticed, with sudden changes from ~70/min to ~40/min. During these episodes, a normal sinus beat, conducted to the ventricle with a positive P wave (Figure 1), was followed by a non-conducted negative P wave. The negative P waves appeared about 140ms from the end of the T wave and a distinct, low-amplitude, positive Ta wave was noted.
Discussion
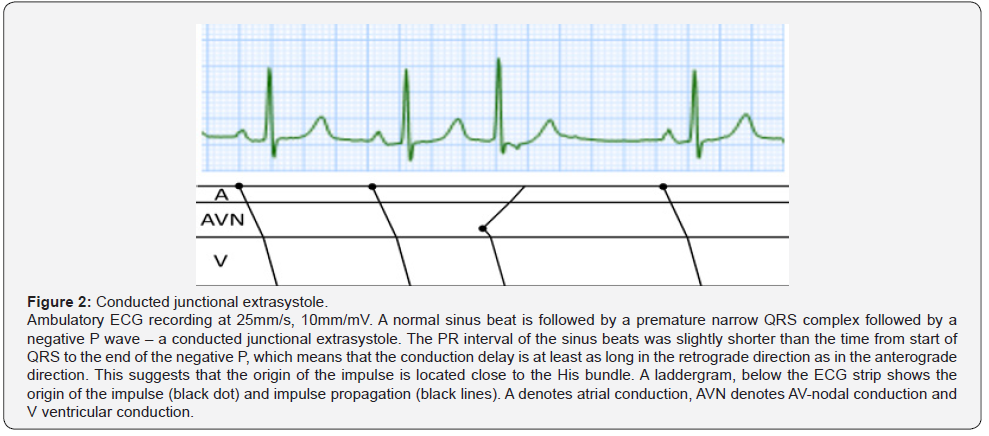
The bradyarrythmia was interpreted as blocked premature junctional contractions (PJCs) in bigeminy. Premature atrial contractions (PACs) are common and sometimes the premature atrial beat is not conducted through the AV node, giving rise to a blocked PAC [1,2]. This is most often due to the prematurity of the beat and not to a “diseased” AV node, i.e. the ventricular conduction system is still refractory [2]. Blocked PACs can be mis-interpreted as second-degree AV block [3]. In our case, the morphology of the non-conducted P wave was very different from that of the sinus P wave, and the risk of misinterpreting it as second-degree AV block was therefore minimal. The negative P wave was however, surprisingly late in relation to the refractory period of the preceding beat. Conduction to the ventricles was not possible due to a refractory distal conduction system, whereas retrograde depolarization of the atria was possible (the negative P wave). A premature beat with similar, negative P wave morphology (Figure 2), recorded when the patient was active and the heart rate was higher, showed slightly longer time from the start of QRS to the end of the negative P wave (190ms) than the PR interval of the preceding sinus beat (180ms), i.e. the conduction delay of the AV node was at least as long in the retrograde direction as in the anterograde direction. This suggests that the origin of the impulse was located either in the AV node or within the AV bundle. PJCs were common during the recording, but the pattern of blocked PJCs in bigeminy only appeared at rest with heart rates below 75/min, likely due to increased refractory periods of the ventricular conduction system, which can increase with increased cycle length of the preceding beat [4]. During exercise, blocked PJCs where uncommon and her symptoms were relieved.
A treatment attempt with flecainide was terminated due to adverse reactions. The interpretation from the surface ECG of blocked PJCs was later confirmed by an electrophysiological study (EPS). During EPS, supraventricular ectopic beats were seen, and they could be suppressed by isoprenaline but re-appeared when isoprenaline infusion was stopped. The earliest endocardial activation site was located above the coronary sinus ostium, very close to the bundle of His. After EPS the patient was in complete AV block. A pacemaker was implanted. On follow-up 3 month later, she had had no symptomatic episodes.
Conclusion
Blocked premature junctional or atrial beats can result in symptomatic bradycardia. In this case, an unexpectedly late, blocked supraventricular ectopy could be explained by a very Hisnear activation site, which made treatment difficult.
References
- Alper A, Gungor B, Turkkan C, Tekkesin A (2013) Symptomatic bradycardia caused by premature atrial contractions originating from right atrial appendage. Indian Pacing Electrophysiol J 13(3): 114-117.
- Wagner GS, Marriott HJL (2008) editors. Marriott’s practical electrocardiography. 11. ed. Philadelphia, Pa.: Wolters Kluwer Health/Lippincott Williams & Wilkins, USA, pp. 293-346.
- Gaudio C, Di Michele S, Ferri FM, Mirabelli F, Franchitto S, et al. (2004) A case of non-conducted atrial bigeminy simulating a second-degree atrioventricular block. A holter ECG diagnosis. Eur Rev Med Pharmacol Sci 8(4): 169-171.
- Denes P, Wu D, Dhingra R, Pietras RJ, Rosen KM (1974) The effects of cycle length on cardiac refractory periods in man. Circulation 49(1): 32-41.






























