“Triple-Rule-Out” in Investigating Cases of Acute Chest Pain (Saudi Experience)
Zizi saad1*, Ragab H Donkol2, Mohamed Elrawy1, Sami Boughattas3 and Adel M Khedrah3
1Department of cardiology, Zagazig university, Egypt
2Department of Radiology, Cairo university, Egypt
3Department of Radiology, Aseer central hospital, Saudi Arabia
Submission: October 26, 2018; Published:November 28, 2018
*Corresponding author: Zizi saad, Department of cardiology, Zagazig university, Aseer -Abha- KSA, Egypt.
How to cite this article: Zizi s, Ragab H D, Mohamed E, Sami B, Adel M K. “Triple-Rule-Out” in Investigating Cases of Acute Chest Pain (Saudi Experience). J Cardiol & Cardiovasc Ther. 2018; 12(4): 555842. DOI: 10.19080/JOCCT.2018.12.555842
Abstract
Objective: Triple Rule-Out (TRO) is a recent Technique for evaluating Emergency Department (ED) acute Chest Pain Patients. The aim of this study is to assess the effectiveness of TRO in identifying the cause of acute chest in emergency department.
Materials and Methods:This is a prospective study done in Kingdom of Saudi Arabia (KSA) tertiary referral hospital during the period between March 2014 and June 2017. 237 patients who fulfill the inclusion criteria and continue all follow up visits for six months were included. They were presented to ED with acute chest pain suspected to be acute coronary syndrome. Their ages ranged between 29 and 72 years old with the mean age of 42.8 years. 164 patients were males and the rest were females. TRO was performed to all of them using a 64 and 128 Multi-Detector Computed Tomography (MDCT) scanners.
Results: According to the results of TRO, the patients had fallen into one of the three groups: (1) Patients with coronary artery disease including 62 patients (26.2%) and were classified according to the severity of the coronary artery stenosis into mild, moderate, and severe stenosis subgroups. (2) Patients with extra-coronary diseases that explain patient’s complaints including 94 patients (39.7%). (3) Patients without obvious disease which can explain patient’s complaints including 81 patients (34.1%). Additional 136 extra-coronary incidental findings which are not related to the presenting complaints were reported and were treated accordingly.
Conclusion: TRO examination is a fast and useful technique in mak¬ing a quick and accurate diagnosis in patients presented to ED with acute non-traumatic chest pain. It allows imaging of the coronary arteries, entire chest, and upper abdominal organs with rapid acquisition and data reconstruction to provide prompt and accurate diagnosis. It is also used to identify many of clinically significant non-cardiac findings that may have an impact on the management of those patients.
Keywords: Triple-rule out; Coronary computed tomography angiography; Coronary artery Disease
Abbrevations: TRO: Triple Rule-Out; ED: Emergency Department; MDCT: Multi-Detector Computed Tomography; ECG: Electrocardiogram; ACS: Acute Coronary Syndrome; IHD: Ischemic Heart Disease; PE: Pulmonary Embolism; CCTA: Coronary Computed Tomography Angiography; HF: Heart Failure; OPD: Outpatient Department; LAD: Left Anterior Descending; CX: Left Circumflex; RCA: Right Coronary
Introduction
Chest pain is one of the most common symptoms in patients presented to Emergency Department (ED). Various differential diagnoses have to be considered, some of them are potentially life-threatening. Some of these patients were having high risk factors of coronary artery diseases, and are presented with typical chest pain, along with Electrocardiogram (ECG) changes suggestive Acute Coronary Syndrome (ACS). However, many others are present with a typical chest pain with some ECG changes which cannot confirm or exclude myocardial ischemia. Some other diseases can present with clinical picture which can mimic Ischemic Heart Disease (IHD) such as Pulmonary Embolism (PE) aortic dissection [1-3] as well as Pulmonary, Pleural or osseous lesions, that must be taken into account [4]. The diagnosis of the cause of chest pain is a true challenge for ED physicians. The uncertainty of the diagnosis of these cases results in the practice of defensive medicine and consequent un-necessary admissions which costs too much [5-8].
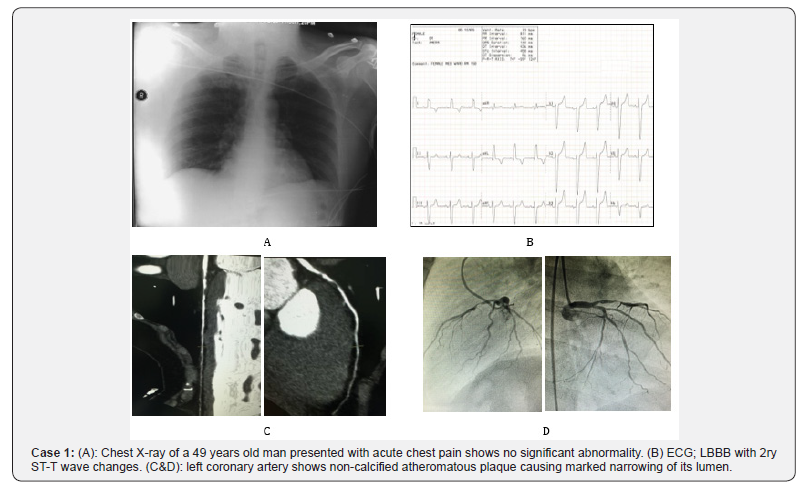
ECG and chest radiography were the first line of investigation of those patients after a good clinical assessment; however, they are of limited value with respect to most of the cases (Case 1). Nowadays, contrast enhanced Multi-Detector computed Tomography (MDCT) is an indispensable diagnostic imaging technique whose use and range of applications has increased dramatically, especially with its recent technical advances [9]. On the other hand the prognostic utility of Coronary Computed Tomography Angiography (CCTA) in evaluation of acute chest pain with low to intermediate risk of ACS is increasingly being established with negative predictive value nearly 100% [10].
Despite its improved diagnostic efficacy over traditional acute chest pain, evaluating protocols CCTA allows only limited assessment of pulmonary vasculature and aortic arch [11]. A recent technique has been introduced into clinical practice which is the Triple Rule Out study (TRO). This technique permits the diagnosis of many other conditions that can cause acute chest pain. It allows the detection of the pulmonary arteries, thoracic aorta and coronary arteries within a single examination. This can be accomplished through the use of a dedicated contrast media administration regimen [12]. Although TRO scans provide simultaneous evaluation of Coronary Artery Disease (CAD), Pulmonary Embolism (PE) and Aortic Disease (AD), their use still not well-defined regarding validity and efficacy [11].
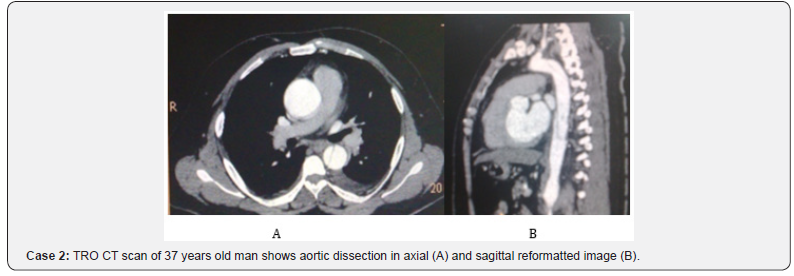
The aim of this study is to evaluate the effectiveness of TRO in investigating cases with acute chest pain that are presented to emergency department in a Saudi tertiary care hospital to identify the cause of the chest pain and take the necessary clinical decision according to the severity of the findings (Case 2).
Materials and Methods
This is a prospective study including all patients presented to emergency departments in a tertiary care hospital during the period between March 2014 and June2017. The study was approved by the hospital review board. Two-hundred and thirty-seven patients who presented with acute chest pain were included in this study. Their ages ranged between 29 and 72 years old with the mean age is 42.8 years. 164 patients were males and the rest were females. The standard care was performed to all patients included in this study according to management and procedures protocols applied in these hospitals. This includes taking full clinical history and immediate clinical assessment by the attending ED physician. ECG and chest radiography were performed immediately, and cardiac biomarkers were requested, followed by immediate consultation to cardiology and pulmonology and cardiothoracic surgery consultants on call. Some emergency medications can be applied to these patients and these do not affect inclusion or exclusion criteria. All patients who fulfilled the inclusion criteria and continue all follow up visits for six months were included. An informed written consent from the patient was considered mandatory to be included in this study.
Patient Selection
All patients presented to ED in these hospitals during the study period were considered eligible for this study if they are above 20 years old and have no history of previous coronary artery disease. The inclusion criteria include:
1. Acute chest pain which may be referred to neck, shoulder, or arm and should not appear to be of musculoskeletal origin.
2. ECG changes should not be conclusive for Acute Coronary Syndrome (ACS).
3. Negative myoglobin and troponin I.
4. Normal serum creatinine or regular dialysis.
5. Sinus Heart Rhythm.
6. Low to Moderate Risk of CAD.
7. Able to hold breathing for accepted time 20-30 sec.
Exclusion criteria included:
1. History of previous cardiac or coronary artery diseases.
2. Cases of traumatic injury.
3. ECG changes or cardiac enzymes diagnostic for ACS.
4. Severe hypotension or Heart Failure (HF).
5. Clinically unfit patient
6. Any contra-indication for contrast administration including contrast allergy or renal insufficiency.
7. Contraindication to radiation exposure i.e. pregnancy
8. Aggressive Calcium scoring above 1000
Study Protocol
According to the results of TRO, the researchers divided the patients into three groups:
1. Patients with suspected acute coronary syndrome (ACS).
2. Patients with extra-coronary diseases that explain patient’s complaints.
3. Patients without obvious disease which can explain patient’s complains.
Additional extra-coronary findings which are not related to the presenting complaints were reported and tabulated. These findings are considered as incidental findings and were managed accordingly and did not affect the patients’ classification. Also, if patients were admitted in the hospital because of these findings alone, they were included in group three.
Group three patients were managed conservatively and immediately discharged after taking near appointment within one week in Outpatient Department (OPD) for further management. Those patients were instructed if they develop any other severe attack of chest pain, hypotension, or tachycardia should come immediately to ED again.
Group two patients were managed according to their diagnoses, and intra-hospital consultations were requested on clinical base until discharge. However, none of these patients develop any MI during their hospital stay.
Group one patients were further classified into two smaller subgroups:
• Patients with non-significant coronary atherosclerotic disease and were managed as group three patients.
• Patients with significant coronary stenosis (>50% lumen narrowing) Admitted immediately to coronary care unit for proper noninvasive/ Invasive management of the coronary arteries accordingly.
Triple Rule-Out Protocol
TRO was performed to all patients included in this study using A 128-MDCT (somatom Di Fintion Flash Siemens Health Care Forchheim, Germany), and64-MDCT (Brilliance Pro, Philips Healthcare). An anti-cubital 18G IV line was inserted and secured prior to the study. The heart rate was controlled below 70b/ min. Some premedication to control the heart rate were given to the patients by order of attending cardiology consultant if no contraindication. ECG leads were connected before taking scout view. Oxygen mask was applied to all patients, and breath-hold training was practiced before taking scout view. The patient was instructed to take breath and to hold up breathing completely during the whole study. A scout view of the chest was obtained to determine the proper location and extent for the triple ruleout scan. Data Acquisition starts from the level of the medial end of the clavicles to the lower border of the heart in cranio-caudal direction. It extends to the upper Abdomen in some cases. Calcium scoring scan was performed to those patients above 45 years old or those with family history of atherosclerosis. A biphasic injection technique was used to image both the coronary arteries and the pulmonary arteries: 60-100 mL of Nonionic iodinated contrast agent Iohexol (Omnipaque; GE healthcare, Chalfont St Giles, England) was injected at 5 mL/s and was followed by a 30-mL injection of the same contrast material mixed with30 mL of saline; also, injected at 5 mL/s. Coronary CTA was initiated with a bolustracking technique 5 seconds after the contrast bolus reached the left atrium. This technique allows visualization of the coronary arteries with the undiluted contrast material from the first phase of the injection and simultaneous visualization of the pulmonary arteries with the dilute contrast material injected from the second phase. The standard scanning parameters for this study were set to {100-120 kvp (if body mass Index > 25kg/m2 (120kvp) but if body mass Index < 25 kg/m2 (100kvp)}.
An initial interpretation was performed while patient still on CT table to be sure of the sufficiency and quality of the study. Also, aortic dissection was looked for and a second complete examination of the whole aorta was performed to see the extent of dissection in case of aortic dissection (Case 3).

Image Interpretation
Interpretation of TRO CT studies includes evaluation of the coronary arteries, as well as of other vascular and nonvascular structures by two expert readers (cardiologist and radiologist with level III training and board certificate). Multiple different planar reformates were then performed for the evaluation of each coronary artery, pulmonary arteries, and aorta using extended diagnostic work station (Syngo MMWP VE 36A, Siemens), and (sun system 4.1-Fracnce). Coronary interpretation was usually made from reconstructed images in mid-diastole with individually optimized the reconstruction window level and width. Additional image reconstructions were performed at end-systole if required. Most of the non-coronary structures are evaluated with axial 3-5-mm-thick images. Thinner sections may be obtained when needed for further evaluation of abnormalities detected on the 3–5-mm sections. Grading of coronary stenosis was based mainly on visual estimation which is the most commonly performed coronary lumen assessment in clinical practice because of its easiness and speed, sometimes it is confirmed by automated assessment [13]. The coronary tree was evaluated using a 16segment model. Significant obstructive CAD was defined as coronary stenosis > 50% in major epicardial vessels (Lt main (LM), Left Anterior Descending (LAD), Left Circumflex (CX), and Right Coronary (RCA) arteries with their branches [11]. Each segment was interpreted visually for the degree of lumen narrowing and rated semi-quantitatively into normal (absence of plaque/no luminal stenosis) minimal (Plaque with < 25% stenosis), mild (25% - 49% stenosis), Moderate (50-69% stenosis), and severe (> 70% stenosis) [14].
Data Analysis
Final diagnoses were established according to the results of TRO and clinical course of each patient. The results of the patients underwent cardiac catheterization were considered as a gold standard. Patients who are treated conservatively the diagnosis was established according to the clinical course and outcome on follow up study for six months
Quantitative variables are presented as range (mean); dichotomous data are presented as frequency (percent), statistical analysis was performed using free trials of statistical soft wares.
Results
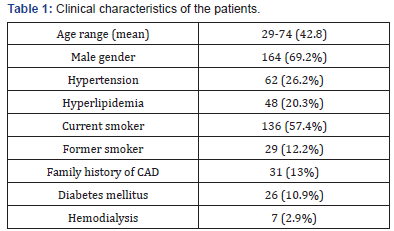
Two-hundred and thirty-seven patients who were presented with a typical acute chest pain were included in this study. Their ages ranged between 29 and 74 years old with the mean age is 42.8 years. 164 patients were males and the rest were females. TRO examination was performed to all these cases and was included in our study if it is complete and of good quality. Patients with incomplete study (23 exams) or with any significant technical faults (7 exams repeated later on) were excluded from this study. Some studies (13 exams 4.2%) with insignificant technical problems were also included, like those patients found to have severe stenosis of one coronary artery and poor opacification of a distal branch of other coronary artery. These small difficulties do not affect patient management, and all examinations were formally reported including hints about these difficulties. Baseline characteristics of those patients are shown in Table 1. An additional session of hemodialysis was arranged to those patients on regular hemodialysis after CT scan when they are clinically stabilized.
According to the results of TRO, the researchers divided the included patients into three groups:
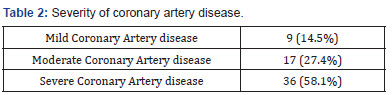
1. Patients with coronary artery disease including 62 patients (26.2%) who were classified according to the severity of the coronary artery stenosis Mild (25%-49% stenosis), Moderate (50% - 69% stenosis), and Severe (more than 70% stenosis) [14] shown in Table 2. Many of these patients were having more than one stenotic segment involving one or more of the coronary arteries. In this case, the patient was counted according to higher severity lesion as one patient. Table 3 shows the distribution along the involved coronary arteries.
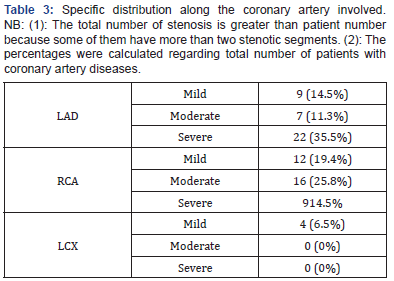
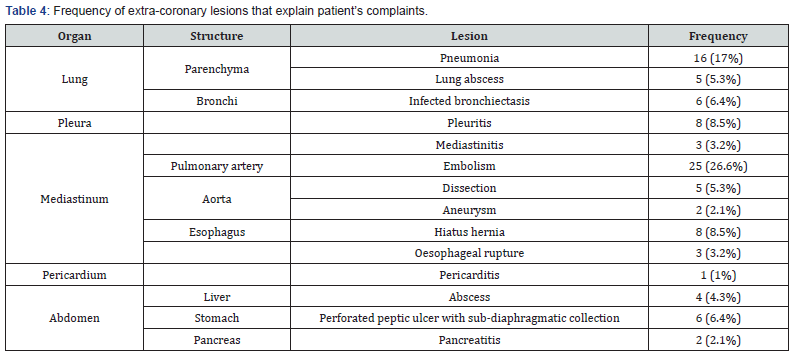
2. Patients with extra-coronary diseases that explain patients’ complaints including 94 patients (39.7%) and were shown in Table 4. Some of these patients were having another lesion/s which was not related to the presenting complaints. In this case, they were counted as incidental findings except if it is related to the same disease process, for example a case with hepatic abscess with mild pleural effusion.
3. Patients without obvious disease which can explain patients’ complaints including 81 patients (34.1%). All these patients were clinically reassured. Non-specific medications were given to some of them, and then they were discharged immediately from ED after taking appointment in OPD clinics.
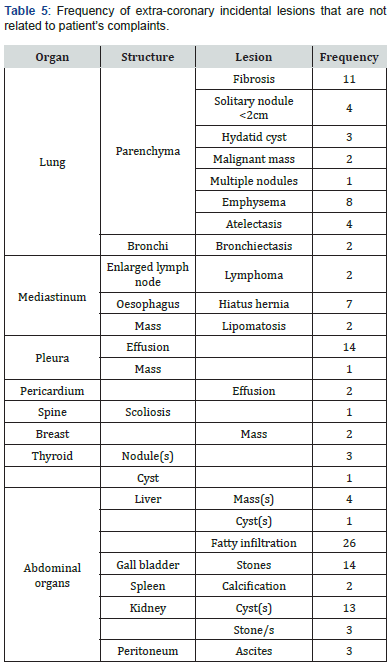
Additional 136 extra-coronary incidental findings that are not related to the presenting complaints were reported and shown in Table 5. These findings were managed accordingly and did not affect patients’ management. Many of these lesions are noted in the previous three groups’ patients and were counted separately if they are of different pathology. Lesions of the same pathology like cases with bilateral simple renal cortical cysts were counted as single lesion. However, if the lesions are of the same pathology but involving more than one organ like hydatid disease in lung and liver, then they were counted as two separate lesions.
Discussion
Chest pain is one of the most common complaints of patients presented to emergency department. Evaluating the causes of chest pain is considered the most difficult challenging to ED physicians, because of the long list of differential diagnoses have to be considered, some of them are potentially life-threatening. The identification of patients with serious diagnoses is sometimes difficult and demands a lot of work-up which may last for several days. The uncertainty of the diagnosis of these cases results in the practice of defensive medicine and consequent un-necessary admissions which costs too much and is considered a burden to the healthcare provider [5,6,15-17]. With the present focus on emergency department congestion and cost containment, any method which can reduce length of stay and charges is essential. Many of the recent studies have shown the efficacy of CCTA in identification of patients with acute coronary artery syndrome [2,16,18-20]. However, some other diseases can present with clinical picture which can mimic ACS like aortic dissection cannot be excluded by CCTA. Those were the targeted people by our study (TRO) which is tailored to widen the benefit of the CT scan to identify other causes of acute chest pain when IHD is excluded by CCTA..
Some studies have demonstrated the application of a triple rule-out protocol with16 and 320 multi-detector CT technology in the ED [3,21-25]. In this study the researchers utilized was a 128- MDCT (somatom Di Fintion Flash Siemens Health Care Forchheim, Germany), and 64-MDCT (Brilliance Pro, Philips Healthcare), both machines are available in the study setting. The usage of this fast CT machine has improved assessment of coronary artery disease in a faster, and more effective way with fewer artifacts which lower the sensitivity of older studies. Also, the researchers demonstrated that it facilitates the diagnosis of other causes of acute chest pain without further diagnostic testing.
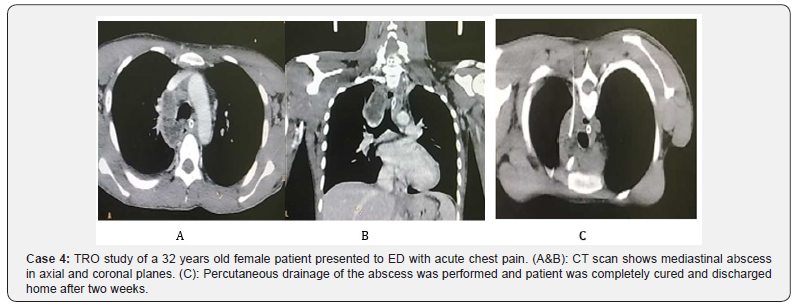
Many studies considered coronary angiography is the gold standard in context of coronary artery diseases and compared its results with the CCTA findings [2,18,26-28]. This study differs from other studies as we did not perform coronary angiography except in cases with significant stenosis. We considered that good quality CCTA is having a reliable negative predictive value (99.4%) [24] and we can exclude the presence of significant coronary artery obstruction with high degree of confidence. This agrees with many studies which demonstrated that a normal CCTA allows the clinician to rule out the presence of significant coronary artery stenosis with a high degree of reliability, and that no further work-up is required to demonstrate the absence of coronary disease [2,18,26,29]. We classified our coronary cases into two subgroups according to the result of and are managed according to degree of stenosis detected by TRO technique. This is different from other studies considering that coronary angiography is mandatory for grading coronary stenosis [30-32]. Moreover, the grading of coronary stenosis by conventional angiography is limited by geometric factors that may result in underestimation or overestimation of the degree of coronary stenosis in over onethird of patients [33]. This was confirmed by the clinical outcome and follow up of our cases (Case 4).
The total number of those patients found to have coronary stenosis was relatively low (26.2% of our population). This might be related to the fact we did not put age limitation for the selected group. Also, we did not take risk factors for coronary artery disease into consideration when selecting those cases. This might be a drawback of our study but our aim was to check the sensitivity of TRO to detect the cause of chest pain, and to check if we can use its result to select those cases that can be discharged early from ED. In this context, our results agree with Kevin M et al. [34], who found that the majority of patients in their study were found to have normal coronary arteries or no more than mild coronary disease (89%, 175 of 197). On the basis of our study we can state that TRO is as effective as CCTA in identifying cases with coronary artery diseases in ED and is excellent modality in selecting cases which can be discharged early. The grading of the coronary artery stenosis we used in our study fits perfectly with the findings of coronary angiography, except in two cases with dense calcific plaques which casts artifacts and overestimate the degree of stenosis in CCTA. This does not affect the total sensitivity of TRO in selecting the patients for further work-up. No-one case reported of having normal coronary arteries were found to have any other significant changes in further studies including trans-thoracic echocardiography and electrocardiogram. No further attacks of chest pain related to coronary artery diseases on clinical follow up for six months reported in this group. This agrees with the results of Kevin M et al. [34], who followed up their cases only for 30 days. Thus, it can be decided that the use of CT imaging permits one to reliably identify patients who do not need revascularization despite the symptoms. Although we did not include cost effectiveness of early discharge of patients with negative TRO results in this study, based on a three small randomized controlled trials with actual patient experience data, each has suggested decreased length of stay with decreased cost from adding coronary CTA to the evaluation of acute chest pain in the emergency department [27,35-37].This study results tend to agree with these articles. Also, we agree with other published series reported that patients discharged from the emergency department on the basis of a negative initial evaluation and negative coronary CTA had no subsequent major adverse cardiac events at the 1-month follow-up [16,23,38,39].
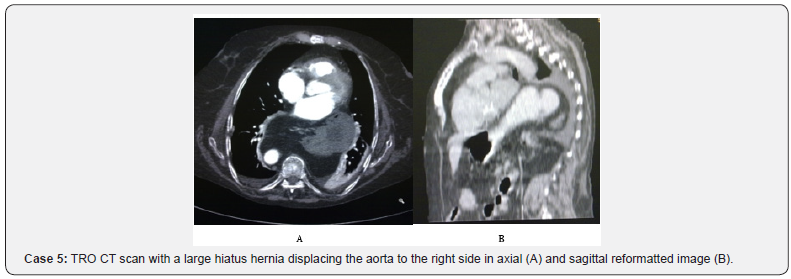
The main value of TRO is its ability to identify the cause of the chest pain in most of the cases. This is obvious from the results of the current study. We identified 39.7% of extra-cardiac causes of acute chest pain in this patient group. Further 136 of non-cardiac incidental lesions were also detected and are not related to the presenting complaint of the patient. The total number of patients with extra-cardiac lesions detected by TRO was 117 patients (49.4%). The true cause of the chest pain was identified as it can explain the patient symptoms after excluding coronary artery disease. The clinical work up done for the patient should support this diagnosis. TRO help us to reach this diagnosis very fast and relatively in an easier way. This diagnosis was not an easy target to reach before TRO study except after performing long list of diagnostic tests which may delay the start of treatment (Case 5).
Our results are lower than the results of other studies examining the prevalence of non-cardiac findings in CCTA. Hunold et al. [40], found extra-coronary abnormalities in 53% of 1,812patients who underwent CCTA for the assessment of coronary artery calcification, whereas Onuma et al. [41] reported that 58% of 503 patients who underwent MDCT of the heart had new, non-cardiac pathology. This high incidence of detection of extra-cardiac lesions may be related to relatively wide inclusion criteria of our patients. Also, we did not include any risk factor for any specific problem including coronary or non-coronary lesions as a selection criterion in our study.
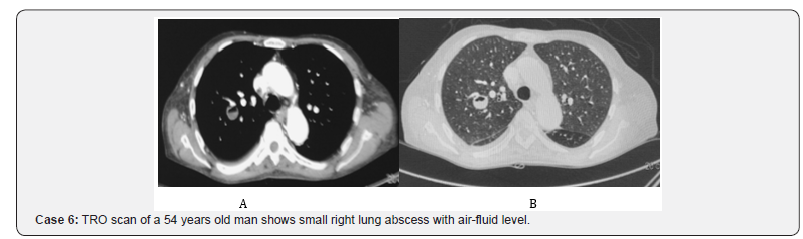
This study results contrast the results of the studies done by Haller et al. [26], Hunold et al. [40] and Onuma et al. [41], Schragin et al. [42], Dewey et al. [43], Horton et al. [44], who reported a prevalence of significant non-cardiac pathology on CCTA of 4.2%, 4.8%, 5%, 7.8%, 11%, and 22.7% respectively. Their cardiac imaging, FOV was confined to be as small as possible included little of the lung or the other chest organs, although all chest organs were irradiated aiming to achieve best resolution. However, in our study because researchers were aiming to find the cause of the chest pain not only to exclude coronary artery diseases, they extended the field of examination to include the whole chest and upper abdomen in some cases. Many of the lesions of these areas may be presented with acute chest pain mimicking that of anginal symptoms (Case 6).
The higher prevalence of non-cardiac findings in our study as compared with those in Cardiac MRI (CMR) in the study done by Becker CR [45], might be explained by the fact that the reporting of benign non-cardiac findings may have been influenced by a given reader’s decision to include (or not include) findings that would not impact the patient’s care in MRI. CT has greater spatial resolution [46,47] and is generally considered to be superior to CMR in detecting pulmonary pathology. Unlike TRO, the CMR examination does not capture the entire chest, and CMR sequences are not optimized for non-cardiac pathology [48].
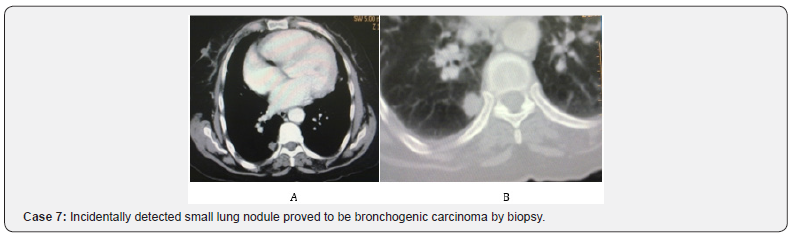
Few reports of extra-coronary findings are available in the triple rule-out literature [19, 34, 41-43, 49]. A study of 69 patients evaluated for chest pain demonstrated three patients with non-coronary diagnoses, including pericarditis, pneumonia, and pulmonary embolism [1]. Another study [50] that used a 64-section triple rule-out protocol in 23 patients who were presented with acute chest pain found only two patients (9%) with pulmonary embolism. In the study done by Kevin M Takakuwa et al [21], they found a detection rate of 25% for extracardiac lesions, 11% of them is significant in explaining patient’s symptoms. The difference in our results with other TRO studies for the detection of extra-cardiac lesions resulted from inclusion of all lesions seen in all images including those appeared in the upper abdominal cuts (Case 7).
Study Limitation
TRO is associated with significantly higher radiation and contrast dose compared with coronary CTA that is because TRO study is 30-40% longer than CCTA. However, we believe that the benefits still outweigh its radiation hazards. Nevertheless, we advise to limit this study to those who cannot be diagnosed clinically, or with less radiation procedures like CCTA alone with second widened reformats to include the irradiated part of the chest. Also, it has been advised by the nice work done by Kevin M. Takakuwa et al. and Radkokkrissa k et al [51,52], ECG-based tube current modulation that it should be selectively used if the patient’s heart rate is sufficiently stable. On the other hand, a cost/efficacy analysis was not performed in the present study. A prospective, controlled study is necessary to elucidate cost/ efficacy of evaluating non-cardiac findings in cardiac MDCT.
However, unlike other studies [3,21,34], the follow up was relatively longer (6 months). The final diagnosis was reached in all cases and was supported by clinical course, and further work up studies done for those patients. Thirdly, the classification of relevant and irrelevant extra-cardiac findings was not subjective but reflects the final clinical diagnosis.
Conclusion
TRO examination is fast, widely available, and is highly helpful in mak¬ing a quick and accurate diagnosis in patients presented to ED with acute non-traumatic chest pain. It allows imaging of the coronary arteries, entire chest, and upper abdominal organs with rapid acquisition and data reconstruction to provide prompt, and accurate diagnosis and to identify many of clinically significant non-cardiac findings that may have an impact on management of those patients. Although many of these non-cardiac findings were not of major importance, some of them were important, including asymptomatic malignancies.
References
- White CS, Kuo D, Kelemen M, Jain V, Musk A, et al. (2005) Chest pain evaluation in the emergency department: can MDCT provide a comprehensive evaluation? AJR Am J Roentgenol 185(2): 533-540.
- Raff GL, Gallagher MJ, O’Neill WW, Goldstein JA (2005) Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol 46(3): 552-557.
- Gallagher MJ, Raff GL (2008) Use of multislice CT for the evaluation of emergency room patients with chest pain: the so-called “triple ruleout”. Catheter Cardiovasc Interv 71(1): 92-99.
- Stillman AE, Oudkerkm, Ackerman M, Becker CR, Buszman PE (2007) Use of multidetector computed tomography for assessment of acute chest pain: a consensus statement of the north American society of cardiac imaging and European society of cardiac radiology. Int J cardiovasc Imaging 23(4): 415-427.
- Karcz A, Korn R, Burke MC, Caggiano R, Doyle MJ, et al. (1996) Malpractice claims against emergency physicians in Massachusetts: 1975-1993. Am J Emerg Med 14(4): 341-345.
- Tosteson AN, Goldman L, Udvarhelyi IS, Lee TH (1996) Costeffectiveness of a coronary care unit versus an intermediate care unit for emergency department patients with chest pain. Circulation 94(2): 143-150.
- Pope JH, Aufderheide TP, Ruthazer R, Woolard RH, Feldman JA, et al. (2000) Missed diagnoses of acute cardiac ischemia in the emergency department. N Engl J Med 342(16): 1163-1170.
- Schull MJ, Vermeulen MJ, Stukel TA (2006) The risk of missed diagnosis of acute myocardial infarction associated with emergency department volume. Ann Emerg Med 48(6): 647-655.
- Lee TY, Chhem RK (2010) Impact of new Technologies on dose reduction in CT. Euro J Radiol 76(1): 28-35.
- Litt HI, Gatsonis C, Snyder B, Singh H, Miller CD, et al. (2012) CT Angiography for safe discharge of patients with possible acute coronary syndromes. N Engl J Med 366: 1393-1403.
- Burris AC 2nd, Boura JA, Raff GL, Chinnaiyan KM (2015) Triple Rule Out Versus Coronary CT Angiography in Patients with Acute Chest Pain: Results From the ACIC Consortium. JACC: Cardiovasc Imaging 8(7): 817-825.
- Savino G, Herzog C, Costello P, Schoepf UJ (2006) 64 slice cardiovascular CT in the emergency department: Concepts and first experiences. Radiol Med 111(4): 481-496.
- Arbab-Zadeh A, Texter J, Ostbye KM, Kitagawa K, Brinker J, et al. (2010) Quantification of lumen stenosis with known dimension by conventional angiography and computed tomography, implications for the use of angiography as a gold standard. Heart 96(17): 1358-1363
- Wu FZ, Wu MT (2015) 2014 SCCT guidelines for the interpretation and reporting of coronary CT angiography: A report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr 9(2): e3.
- Thomas J, Rideau AM, Paulson EK, Bisset GS 3rd (2008) Emergency department imaging: current practice. J Am Coll Radiol 5(7): 811-816.
- Ladapo JA, Hoffmann U, Bamberg F, Nagurney JT, Cutler DM, et al. (2008) Cost-effectiveness of coronary MDCT in the triage of patients with acute chest pain. AJR Am J Roentgenol 191(2): 455-463.
- Rusnak RA, Stair TO, Hansen K, Fastow JS (1989) Litigation against the emergency physician: common features in cases of missed myocardial infarction. Ann Emerg Med 18(10): 1029-1034.
- Vanhoenacker PK, Heijenbrok-Kal MH, Van Heste R, Decramer I, Van Hoe LR, et al. (2007) Diagnostic performance of multidetector CT angiography for assessment of coronary artery disease: meta-analysis. Radiology 244(2): 419-428.
- Vrachliotis TG, Bis KG, Haidary A, Kosuri R, Balasubramaniam M, et al. (2007) A typical chest pain: coronary, aortic, and pulmonary vasculature enhancement at biphasic single-injection 64-section CT angiography. Radiol 243(2): 368-376.
- Gruettner J, Fink C, Walter T, Meyer M, Apfaltrer P, et al. (2013) Coronary computed tomography and triple rule out CT in patients with acute chest pain and an intermediate cardiac risk profile. Part 1: Impact on patient management. Eur J Radiol 82(1): 100-105.
- Takakuwa KM, Halpern EJ (2008) Evaluation of a “triple rule-out” coronary CT angiography protocol: use of 64-section CT in low-tomoderate risk emergency department patients suspected of having acute coronary syndrome. Radiology 248(2): 438-446.
- Takakuwa KM, Halpern EJ, Gingold EL, Levin DC, Shofer FS (2009) Radiation dose in a “triple rule-out” coronary CT angiography protocol of emergency department patients using 64-MDCT: the impact of ECGbased tube current modulation on age, sex, and body mass index. AJR Am J Roentgenol 192(4): 866-872.
- Dodd JD, Kalva S, Pena A, Bamberg F, Shapiro MD, et al. (2008) Emergency cardiac CT for suspected acute coronary syndrome: qualitative and quantitative assessment of coronary, pulmonary, and aortic image quality. AJR Am J Roentgenol 191(3): 870-877.
- Soliman HH (2015) Value of triple rule-out CT in the emergency department. The Egypt Journal radiology and nuclear medicine 46(3): 621-627.
- Chae MK, Kim EK, Jung KY, Shin TG, Sim MS, et al. (2016) Triple ruleout computed tomography for risk stratification of patients with acute chest pain. Journal of Cardiovascular Computed Tomography 10(4): 291-300.
- Haller S, Kaiser C, Buser P, Bongartz G, Bremerich J (2006) Coronary artery imaging with contrast-enhanced MDCT: extracardiac findings AJR Am J Roentgenol 187: 105-110.
- Leschka S, Alkadhi H, Plass A, Desbiolles L, Grunenfelder J, et al. (2005) Accuracy of MSCT coronary angiography with 64-slice technology: first experience. Eur Heart J 26(15): 1482-1487.
- Ropers D, Rixe J, Anders K, Kuttner A, Baum U, et al. (2006) Usefulness of multidetector row spiral computed tomography with 64- x 0.6- mm collimation and 330-ms rotation for the noninvasive detection of significant coronary artery stenosis. Am J Cardiol 97(3): 343-348.
- Budoff MJ, Li D (2014) Coronary CT Angiography again results in better patient out-come. J Am Coll Cardio 64(7): 741-742.
- Nikolaou K, Flohr T, Knez A, Rist C, Wintersperger B, et al. (2004) Advances in cardiac CT imaging: 64-slice scanner. Int J Cardiovasc Imaging 20(6): 535-540.
- Nieman K, Cademartiri F, Lemos PA, Raaijmakers R, Pattynama PM, et al. (2002) Reliable noninvasive coronary angiography with fast submillimeter multislice spiral computed tomography. Circulation 106(16): 2051-2054.
- Ropers D, Baum U, Pohle K, Anders K, Ulzheimer S, et al. (2003) Detection of coronary artery stenosis with thin-slice multi-detector row spiral computed tomography and multiplanar reconstruction. Circulation 107(5): 664-666.
- Budoff MJ, Dowe D, Jollis JG, Gitter M, Sutherland J, et al. (2008) Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter accuracy (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol 52(21): 1724-1732.
- Takakuwa KM, Halpern EJ (2008) Evaluation of a “Triple Rule-Out” Coronary CT Angiography Protocol: Use of 64-Section CT in Low-to- Moderate Risk Emergency Department Patients suspected of Having Acute Coronary Syndrome. Radiology 248(2): 438-446.
- Rubinshtein R, Halon DA, Gaspar T, Jaffe R, Karkabi B, et al. (2007) Usefulness of 64-slice cardiac computed tomographic angiography for diagnosing acute coronary syndromes and predicting clinical outcome in emergency department patients with chest pain of uncertain origin. Circulation 115(13): 1762-1768.
- Mollet NR, Cademartiri F, van Mieghem CA, Runza G, McFadden EP, et al. (2005) High-resolution spiral computed tomography coronary angiography in patients referred for diagnostic conventional coronary angiography. Circulation 112(15): 2318-2323
- Frauenfelder T, Appenzeller P, Karlo C, Scheffel H, Desbiolles L, et al. (2009) Triple rule-out CT in emergency Department: Protocols and spectrum of Imaging Findings, Eur Radiol 19: 789-799.
- Miller JM, Rochitte CE, Dewey M, Arbab-Zadeh A, Niinuma H, et al. (2008) Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med 359(22): 2324-2336.
- Hulten AE, Carbonaro S, Petrillo SP, Mitchell JD, Villines TC (2011) Prognostic value of cardiac computed tomography angiography: a systematic review and meta-analysis. J Am coll cardiol 57(10): 1237- 1247.
- Hunold P, Schmermund A, Seibel RM, Gronemeyer DH, Erbel R (2001) Prevalence and clinical significance of accidental findings in electronbeam tomographic scans for coronary artery calcification. Eur Heart J 22(18): 1748-1758.
- Onuma Y, Tanabe K, Nakazawa G, Aoki J, Nakajima H, et al. (2006) Noncardiac findings in cardiac imaging with multidetector computed tomography. J Am Coll Cardiol (2006) 48(2): 402-406.
- Schragin JG, Weissfeld JL, Edmundowicz D, Strollo DC, Fuhrman CR (2004) Non-cardiac findings on coronary electron beam computed tomography scanning. J Thorac Imaging 19(2): 82-86.
- Dewey M, Schnapauff D, Teige F, Hamm B (2007) Non-cardiac findings on coronary computed tomography and magnetic resonance imaging. Eur Radiol 17(8): 2038-2043.
- Horton KM, Post WS, Blumenthal RS, Fishman EK (2002) Prevalence of significant noncardiac findings on electron-beam computed tomography coronary artery calcium screening examinations. Circulation 106(5): 532-534.
- Becker CR (2005) Coronary CT angiography in symptomatic patients. Eur Radiol suppl 2: B33-B41.
- Stacey RB, Hundley WG (2013) The role of Cardiovascular Magnetic Resonance (CMR) and computed Tomography (CCT) in facilitating heart failure management. Curr Treat Options Cardiovasc Med 15(4): 373-386.
- Whitaker J, Rajani R, Chubb H, Gabrawi M, Varela M, et al. (2016) The role of myocardial wall thickness in atrial arrhythmogenesis. Europace 18(12): 1758-1772.
- Chan PG, Smith MP, Hauser TH, Yeon SB, Appelbaum E, et al. (2009) Noncardiac Pathology on Clinical Cardiac Magnetic Resonance Imaging. JACC Cardiovasc imaging 2(8): 980-986.
- McKenna DA, Laxpati M, Colletti PM (2008) The prevalence of incidental findings at cardiac MRI. Open Cardiovasc Med J 2: 20-25.
- Savino G, Herzog C, Costello P, Schoepf UJ (2006) 64 slice cardiovascular CT in the emergency department: concepts and first experiences. Radiol Med 111(4): 481-496.
- Takakuwa KM, Halpern EJ, Gingold EL, Levin DC, Shofer FS (2009) Radiation Dose in a “Triple Rule-Out” Coronary CT Angiography Protocol of Emergency Department Patients Using 64-MDCT: The Impact of ECG-Based Tube Current Modulation on Age, Sex, and Body Mass Index. AJR Am J Roentgenol 192(4): 866-872.
- Krissa R, Henzler T, Prechel A, Reichert M, Gruettner J, et al. (2012) Triple-rule-out dual-source CT angiography of patients with acute chest pain: Dose reduction potential of 100 kV scanning. Eur J Radiol 81(12): 3691-3696.






























