Osteitis Fibrosa Cystica (Brown Tumour) of the Cervical Spine in a Patient with Polycystic Kidney Disease Masquerading as Metastatic Malignant Bone Disease - Case Report
Amit Amit1, Atul Vats2*, Shabin Joshi1, Khaled Sherlala3 and Amjad Shad3
1Consultant Neurosurgeon, University hospital Coventry and Warwickshire, UK
2Clinical Fellow of Neurosurgery, University hospital Coventry and Warwickshire, UK
3Consultant Neuroradiologist, University hospital Coventry and Warwickshire, UK
Submission: March 13, 2018; Published: April 09, 2018
*Corresponding author: Atul Vats, Clinical Fellow of Neurosurgery, University hospital Coventry and Warwickshire, Coventry, CV22DX,Tel: 07448765620; Email: vatsatu17@gmail.com
How to cite this article: Amit A, Atul V, Shabin J, Khaled S, Amjad S. Osteitis Fibrosa Cystica (Brown Tumour) of the Cervical Spine in a Patient with Polycystic Kidney Disease Masquerading as Metastatic Malignant Bone Disease - Case Report. J Head Neck Spine Surg. 2018; 2(4): 555595. DOI: 10.19080/JHNSS.2018.02.555595
Abstract
Context: Osteitis fibrosa cystica (Brown Tumour) is a rare benign lesion of bone. It usually occurs in secondary hyperparathyroidism. Cervical spine involvement is very rare.
Findings: We present one such rare case of Brown tumour of cervical spine due to secondary hyperparathyroidism.
Conclusion: Brown tumour should be considered as a differential diagnosis in cases with multiple lytic lesions of the skeletal system.
Keywords: Osteitis fibrosa cystica (Brown Tumour); Secondary hyperparathyroidism; Cervical spine
Introduction
Brown tumor is a rare benign lesion of the bone. It results from disturbed bone remodeling due to long-standing increase in parathyroid hormone (PTH) level [1]. The incidence is less than 5% in primary hyperparathyroidism [2]. It is more common in secondary hyperparathyroidism, with a reported incidence of up to 13% of cases [3,4]. Bone involvement, usually focal lytic lesion, has a predilection for facial and mandibular bones, but can occur at any bone [5,6]. Spine involvement is very rare [7]. Cervical spine involvement is extremely rare [3,8]. There are only five cases of cervical spine involvement reported, three of which are of secondary hyperparathyroidism [1]. We report one such case of Brown tumor of cervical spine due to secondary hyperparathyroidism.
Case Report
A 55 year old lady presented with chronic axial neck pain and left sided global brachialgia. The neurological examination was unremarkable. She had a history of inherited polycystic kidney disease but was otherwise well.
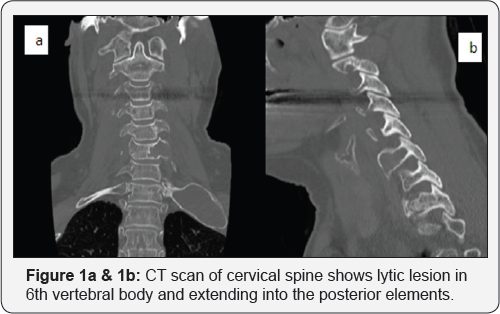
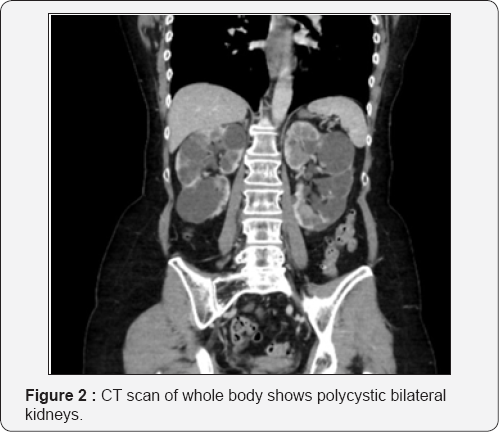
The CT of the Cervical Spine demonstrated a well delineated expansile lytic lesion in the 6th cervical vertebral body extending into the posterior elements (Figure 1a & 1b). There was no neural compression. A whole-body CT scan revealed another lesion in the Left 1st rib. The rib was similarly expanded and hollow in appearance. Multiple cysts were found in both kidneys and the liver (Figure 2). Serum calcium and PTH were raised.
A Neuroradiology MDT (Multidisciplanary Team) decided that the patient had multiple Osteitis fibrosa cystica/Brown tumour (OFC/BT) of the skeletal system. A decision not to offer biopsy or any other forms of curative surgery was taken. A routine follow up for clinical and radiological surveillance did A routine follow up for clinical and radiological surveillance did not show any further progression.
Discussion
OFC is also called Von Recklinghausen's disease of bone and it was first described by Friedrich Daniel von Recklinghausen in 1890. OFC is a form of renal osteodystrophy, which is a skeletal complications of end stage renal disease [9]. The chronic kidney dysfunction due to polycystic disease caused the kidneys to produce less calcitriol which led to high parathyroid hormone levels, halting the storage of calcium. This leads to high levels of calcium, parathyroid hormone and alkaline phosphatase.
Conventional radiographs have been historically used to diagnose the disease. Usual findings are extremely resorbed, thin bones which are sometimes deformed or fractured. CT scan characteristics of brown tumor are expansile lytic lesions, with various amounts of bone destruction and thinning of trabeculae [8,10].
Brown tumor should be differentiated from aneurysmal bone cyst, giant cell tumor, myeloma, Paget's disease [11], Langerhans cell histiocytosis, multiple myeloma [8] and metastasis [12,13]. Medical management of OFC consists of Vitamin D treatment which in some cases has resulted in regression of these tumours [10,14]. Brown tumours are long standing and slowly progressing bone conditions driven by the underlying condition which can range from conservative and supportive care to surgical intervention. If part of a generalised bone disease then treatment should be directed to underlying condition.
Occasionally brown tumours of the spine require surgical intervention if causing instability or neurological compression [11]. In severe cases of OFC, partial or total parathyroidectomy has been shown to result in the reversal of bone resorption and the complete regression of brown tumours. Pre-emptive surgical intervention was not offered in this case as the patient had no neurological signs or symptoms.
Conclusion
OFC should be considered as a differential diagnosis in cases with multiple lytic lesions of the skeletal system. This can avoid unnecessary anxiety and possible unwarranted intervention both for the treating physician and the patients.
Patient Consent
Informed consent was obtained from the patient included in this case report.
References
- Hoshi M, Takami M, Kajikawa M, Teramura K, Okamoto T, et al. (2008) A case of multiple skeletal lesions of brown tumors, mimicking carcinoma metastases. Arch Orthop Trauma Surg 128(2): 149-154.
- Haddad FH, Malkawi OM, Sharbaji AA, Jbara IF, Rihani HR (2007) Primary hyperparathyroidism. A rare cause of spinal cord compression. Saudi Med J 28(5): 783-786.
- Jackson W, Sethi A, Carp J, Talpos G, Vaidya R (2007) Unusual spinal manifestation in secondary hyperparathyroidism: a case report. Spine (Phila Pa 1976) 32(19): E557-E560.
- Mustonen AO, Kiuru MJ, Stahls A, Bohling T, Kivioja A, et al. (2004) Radicular lower extremity pain as the first symptom of primary hyperparathyroidism. Skeletal Radiol 33(8): 467-472.
- Altan L, Kurtoglu Z, Yalcinkaya U, Aydinli U, Erturk E (2007) Brown tumor of the sacral spine in a patient with low-back pain. Rheumatol Int 28(1): 77-81.
- Maddison PJ, Isenberg DA, Woo P, Glass DN (1998) Oxford textbook of rheumatology. Oxford: Oxford University Press, pp. 277-278.
- Azria A, Beaudreuil J, Juquel JP, Quillard A, Bardin T (1998) The endocrine system, clinical presentation of rheumatic disease. Brown tumor of the spine revealing secondary hyperparathyroidism. Report of a case. Joint Bone Spine 67: 230-233.
- Mateo L, Massuet A, Sola M, Perez Andres R, Musulen E, et al. (2011) Brown tumor of the cervical spine: a case report and review of the literature. Clin Rheumatol 30(3): 419-424.
- Turner RH, Farber E, Hopkins JV (1952) Clinicopathologic conference; polycystic kidneys with generalized osteitis fibrosa cystica and parathyroid hyperplasia.
- Mak KC, Wong YW, Luk KD (2009) Spinal cord compression secondary to brown tumour in a patient on long-term haemodialysis: a case report. J Orthop Surg (Hong Kong) 17(1): 90-95.
- Fineman I, Johnson JP, Di-Patre PL, Sandhu H (1999) Chronic renal failure causing brown tumors and myelopathy. Case report and review of pathophysiology and treatment. J Neurosurg 90(2 Suppl): 242-246.
- Kaya RA, Cavusoglu H, Tanik C, Kahyaoglu O, Dilbaz S, et al. (2007) Spinal cord compression caused by a brown tumor at the cervicothoracic junction. Spine J 7(6): 728-732.
- Chew FS, Hellinger FH (1993) Brown tumor. AJR Am J Roentgenol 160: 752.
- Arabi A, Khoury N, Zahed L, Birbari A, El-Hajj Fuleihan G (2006) Regression of skeletal manifestations of hyperparathyroidism with oral vitamin D. J Clin Endocrinol Metab 91(7): 2480-2483.






























