Comparison of the Effects of Clonidine, Promethazine, and Morphine on Bleeding During Rhinoplasty Surgery: A Triple-blind Clinical Trial Study
Amirsadra Zangouei1, Seyed Ali Hossein Zahraei2, Seyyed Hasan Karbasy2, Maryam Rahmanifar2 and Malihe Zangoue2*
11Faculty of Medicine, Mashhad University of Medical Sciences, Iran
22Department of Anesthesiology, Birjand University of Medical Sciences, Iran
Submission: May 02, 2019; Published: May 31, 2019
*Corresponding author: Malihe Zangouei, Assistant Professor, Department of Anesthesiology, Faculty of Medicine, Birjand University of Medical Sciences, Birjand, Iran
How to cite this article: Amirsadra Zangouei, Seyed Ali Hossein Zahraei, Malihe Zangoue, et al. Comparison of the Effects of Clonidine, Promethazine, and Morphine on Bleeding During Rhinoplasty Surgery: A Triple-blind Clinical Trial Study. J Anest & Inten Care Med. 2019; 9(1): 555752. DOI: 10.19080/JAICM.2019.09.555752
Abstract
Introduction: Intraoperative bleeding is a complication of rhinoplasty which directly affects the outcome of the surgery and the hemodynamic indices of the patient. Different approaches like administration of premedication’s, head elevation, and use of vasoconstrictor agents like phenylephrine and epinephrine and have been used to minimize the amount of blood loss. Objective: To compare the impact of clonidine, promethazine, and morphine drugs used as premedication on bleeding during rhinoplasty. Methods: In this clinical trial study, 60 patients of those referred to ENT clinic of Vali-e-Asr Hospital for rhinoplasty and met the inclusion criteria, were chosen by convenience sampling and were divided into three groups, 20 patients in each, by permuted block randomization. Anesthesia method was the same in these groups. One hour before the surgery, patients in the clonidine and promethazine groups received 300μg clonidine and 25mg promethazine orally, respectively, and patients in the morphine group received 0.1mg/Kg of morphine intramuscularly. Data were analyzed by SPSS software version 15 using One-way ANOVA, Tukey, Kruskal-Wallis, and Mann-Whitney U tests. A P-value less than 0.05 was considered statistically significant. Results: This study showed that the mean amount of bleeding during surgery was less in the clonidine group compared with other groups, but this difference was not significant (P=0.07). Systolic blood pressure, heart rate per minute, and erythrocyte saturation rate immediately after intubation, 0.5, 1, 1.5, and 2 hours after intubation showed no considerable difference between the groups (P>0.05). The surgeon’s satisfaction with the surgery was significantly higher in the clonidine group patients (P=0.04). Conclusion: Average bleeding in the clonidine group patients was less than other patients and that the result is not statistically significant may be due to small sample size. With regard to higher satisfaction of the surgeon with clonidine, we suggest it is used as a premedication in rhinoplasties.
Keywords: Clonidine; Promethazine; Morphine; Bleeding; Rhinoplasty
Introduction
Rhinoplasty is a plastic surgery of the nose for reconstructing and correcting its form, improving its function or for esthetic reasons [1]. It is the most common plastic surgery in Iran [2]. The rate of rhinoplasty in Iran is 180 per 100,000 populations [3], which is amongst the world highest rate of this surgery [4]. Bleeding is a critical complication of rhinoplasties [5] like other surgical procedures [6], which causes a major challenge for the surgeons and the anesthesiologists. Mortality rate may increase up to 20% due to severe blood loss; however, it is low (ranging from 0.1% to 8 %) for most surgical operations [7]. Furthermore, a large amount of blood loss results in prolongation of the time of surgery, an increased possibility of further complications and sometimes may lead to a faulty surgical operation [8]. The surgical area of rhinoplasty is highly vascular and damage to the wall of great vessels like the Angular artery or small vessels such as capillary leads to hemorrhage during the rhinoplasty [9]. There are various approaches to limit and stop intraoperative and postoperative blood loss in surgery such as 60-degree head elevation over the trunk [10], the formation of controlled hypotension [11], use of local vasoconstrictor agents like epinephrine and phenylephrine [12], and use of premeditations [13]. Clonidine is an alpha-2 adrenergic agonist [14] and an antihypertensive agent which plays its role mainly by suppressing sympathetic activity [15], and causes central regulation of vasoconstrictor tone [16]. Studies have approved the effect of clonidine premedication before anesthesia in reducing bleeding in otolaryngology surgeries [17,18]. Moreover, Cormack JR et al. [17] showed that alpha-2 agonists like clonidine are beneficial adjuncts of neurosurgeries because of their benefits like blood pressure stabilization, analgesia, and sedation without any significant respiratory side effect [17]. Promethazine and morphine are other premedication’s that have been used to induce pain relief, reduce preoperative anxiety and prevent postoperative physiological changes [19,20]. There have been several studies showing the efficacy of clonidine as a premedication in reducing complications such as blood loss during surgeries, postoperative shivering, and agitation [21], and inducing sedative and analgesic impacts [22,23]; however, there is little evidence comparing the influence of promethazine and morphine with clonidine on the bleeding in rhinoplasty. In this study, we aimed to compare the impact of clonidine, promethazine, and morphine as premedication on blood loss during rhinoplasty and hemodynamic indices like blood pressure, systolic and diastolic pressure, heart rate and erythrocyte saturation rate.
Material and Methods
Design and data collection
This clinical trial was conducted at Vali-e-Asr Hospital affiliated with Birjand University of Medical Sciences in 2017. This study was triple-blind, and the intervention was unknown to the participants, individuals who administered the intervention, and the person who assessed the outcome. According to Jabalameli et al. [24] study, the minimum sample size for each group was determined 18 with 95% level of confidence, and in this study was considered 20 for each group. Out of those who referred to ENT clinic of Vali-e-Asr Hospital for rhinoplasty and met the inclusion criteria, 60 patients were chosen by convenience sampling. Demographic checklists were used to obtain patients’ ages and genders. Patients were divided into three groups, clonidine, promethazine, and morphine groups (20 each) by permuted block randomization.
Inclusion and exclusion criteria
Individuals aged 18 to 60, with no history of the cardiac, renal, and hepatic disease or severe mental disorders, and with no record of anti-depression or anticoagulant drugs or monoamine oxidase inhibitors intake were eligible to enter the study. Individuals were excluded from the study on the basis of having systolic and diastolic pressures above 160 and 90mmHg respectively, heart rate less than 50 per minute, and developing bleeding disorders like hemophilia, thalassemia or leukemia
Ethics
This study was approved by the ethics committee of Birjand University of Medical Sciences (code: Ir.bums.REC.1396.65) and was registered with IRCT20140519017756N36 code at the Iranian Registry of Clinical Trials. At the beginning of the study, all participants were informed about the aim of the study and written informed consent was obtained from each of them. Moreover, they have ensured that their information remains confidential throughout the study.
Study procedure
Patients in the clonidine and promethazine groups received 300μg clonidine and 25mg promethazine orally, respectively, one hour prior to the surgery. Patients in the morphine group received 0.1mg/Kg morphine one hour before inducing anesthesia, intramuscularly. For inducing anesthesia, fentanyl with the dose of 100μg/Kg, propofol with the dose of 100μg/Kg, and atracurium with the dose of 100μg/Kg were used, and after reaching the adequate depth of anesthesia, intubation was done using a proper tube. Patients also received 100μg/Kg/minute for maintenance of the anesthesia. Furthermore, controlled hypotension was archived through the injection of 0.1μg/Kg/minute of fentanyl. For all patients, the pharyngeal tampon was placed to absorb blood and measure the amount of blood entering the digestive tract. Systolic and diastolic pressures Mean Arterial Pressure (MAP), heart rate, and erythrocyte saturation rate were measured before anesthesia, after intubation, and every 30 minutes after the start of the surgery, using Saadat monitoring device. The amount of bleeding during the surgery was determined by measuring the blood volume in the suction, and the weight difference of the gauzes used (regarding that the density of blood (1.04), 1gr of blood was considered equal to 1cc of it).
Statistical analysis
Statistical analysis was performed by SPSS for Windows version 15 (SPSS Inc. Chicago, IL). The Kolmogorov-Smirnov test was used to examine normal distribution. For variables like systolic and diastolic blood pressures, and the alteration of diastolic blood pressure, which were normally distributed One-way ANOVA test was used. Tukey test was performed to compare the alterations in the diastolic pressure among the groups. For non-normally distributed variables such as the amount of bleeding, the MAP and its alteration, and the erythrocyte saturation, Kruskal-Wallis and Mann-Whitney U tests were performed. A p value<0.05 was considered statistically significant in all analyses.
Results
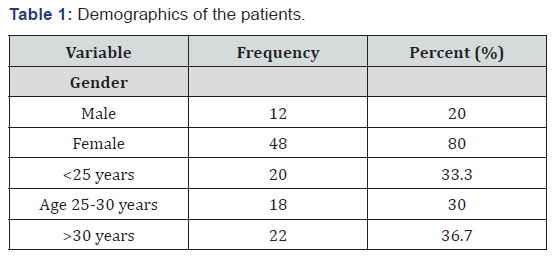
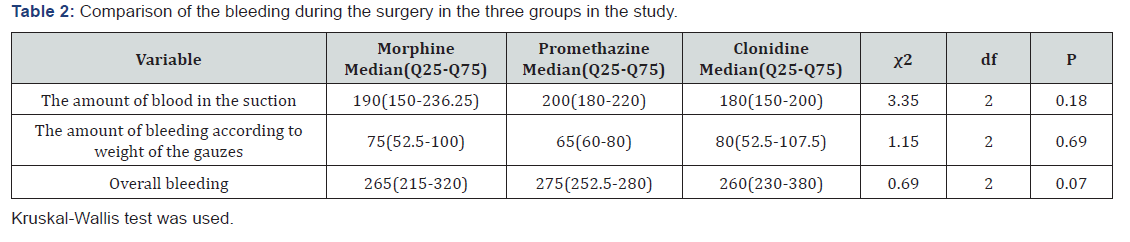
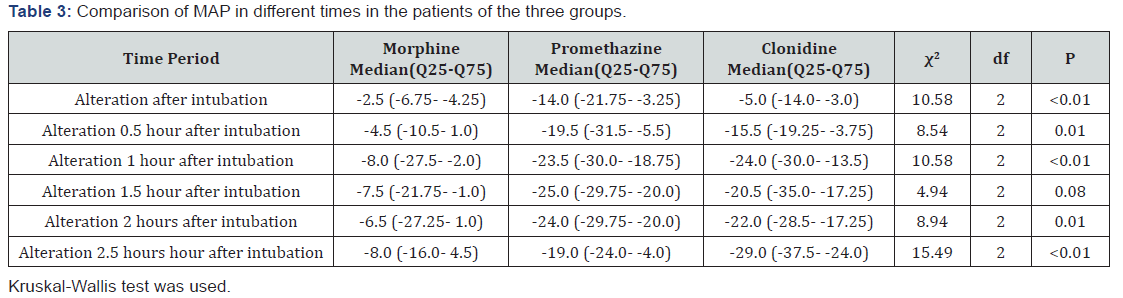
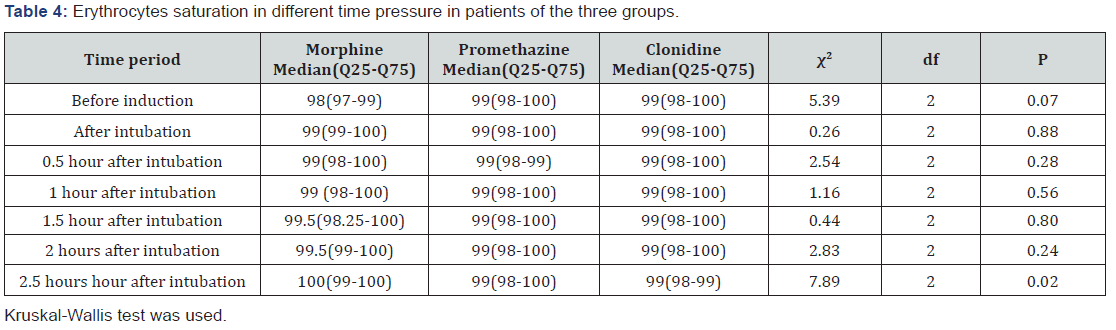
This study was performed on 60 patients with mean age=28.10 (SD=7.31). Demographics of the patients are shown in Table 1. Patients were divided into three groups, clonidine, promethazine, and morphine groups (20 each) with mean ages of 29.25±8.08, 28.60±7.95, and 26.45±5.74, respectively; however this difference did not reach meaningfulness level (P=0.46). Furthermore, Distribution of the age and genders of the patients in the three groups showed no significant difference (P=0.35 and P=0.99 respectively). Table 2 shows the amount of bleeding in the different groups. Although the blood loss is less in the clonidine group as compared with other groups, it was not statistically significant (P=0.07). One-way ANOVA test demonstrated that the mean of systolic blood pressures before induction, immediately after intubation, 0.5, 1, 2, and 2.5 hours after that in the patients of the three groups, showed no significant difference (P>0.05). The diastolic blood pressures before induction showed a significant difference among the groups (P=0.03), so evaluations were conducted on the alterations of the diastolic blood pressures. One-way ANOVA test showed that the alterations of diastolic blood pressures immediately after intubation, 0.5, 1, and 2 hours after that in the three groups marked no considerable difference (P>0.05). However, the alteration of diastolic blood pressures 1.5 and 2.5 hours after intubation in at least two of the three groups was statistically significant (P<0.05). The Tukey test showed that at 2.5 hours after the intubation, the decrease level of diastolic blood pressure in the administration of clonidine was significantly more than the administration of morphine (P<0.01). Nevertheless, no meaningful difference was observed between the alterations of diastolic blood pressure between any 2 groups, 1.5 hours after intubation. MAP of the patients showed a significant difference before induction in the three groups (P=0.02); therefore, alterations of the MAP was compared between groups (Table 3). Furthermore, heart rates of the patients in different groups showed no significant difference (P=0.07). (Table 4) demonstrates the erythrocyte saturation rate in study groups. This table shows that the erythrocyte saturation rate in the groups 2.5 hours after intubation marks a significant difference (P=0.02). Further examination with Mann-Whitney U showed that erythrocyte saturation rate 2.5 hours after intubation in patients of the morphine group was considerably higher as compared with those in the clonidine group (P=0.02). Our results also mention that surgeon satisfaction in 10% of morphine and promethazine and 40% of clonidine groups was at the excellence level, and this difference was statistically significant (P=0.04).
Discussion
Bleeding during rhinoplasty remains a major challenge for anesthetists and surgeons, which directly affects the duration and outcome of the operation. Premedication’s like clonidine have been used to decrease intraoperative blood loss and induce hemodynamic stability. Perioperative use of clonidine has been shown to have antihypertensive effect. Promethazine is a premedication used to reduce postoperative nausea and vomiting [25]. Morphine is another premedication which is utilized to provide postoperative pain relief for the patients [26]. Although there have been several studies confirming the antihypertensive effect of clonidine and its impact on reducing blood loss during surgeries like endoscopic sinus surgery [27], laparoscopic cholecystectomy [28], and aortic [29] surgeries, there is little evidence concerning the role of other premedication’s like promethazine and morphine on blood pressure and bleeding during the surgery. In this study we compared the effects of clonidine, promethazine, and morphine on the intraoperative bleeding and hemodynamic factors like MAP, systolic and diastolic pressures, and heart rate, which to the best of our knowledge is the first study to do so. In our study, we found that intraoperative blood loss was less in clonidine group which we believe is due to its inhibitor effect on alpha-2 receptors in central nervous system leading to constriction of blood vessels and hypotension [30]. However, this difference did not reach significance level maybe because of small sample size. Ghazipour et al. [31] showed in their study that the mean amount of bleeding in the patients undergoing rhinoplasty who received oral clonidine prior to anesthesia was significantly less than those who received placebo [31]. Providing intraoperative hypotension reduces blood loss and leads to better surgical sight vision for the surgeon which in turn affects the operation result. Our study showed that MAP 2.5 hours after intubation was significantly less in clonidine group as compared with the promethazine and morphine groups. Confirming our results, Woodcock et al. [32] showed that the use of clonidine has significant effect in inducing hypotension in surgery [32]. In this study, we took surgeon’s satisfaction of the operation into account and found out that surgeon’s satisfaction in the surgery of clonidine group patients was significantly higher, which may due to its hypotensive effect which reduces bleeding and provides a bloodless field for the surgeon. Surgeon’s skill is a key factor in the amount of bleeding and the result of the operation; therefore, to minimize the impact of the skill of the surgeon, all the rhinoplasties were conducted by one surgeon. Body and environment temperatures, bleeding and coagulation time are other factors affecting the amount of bleeding, which we hope that will be considered in the future studies. We also suggest that likewise studies be performed with a control group and bigger sample size to stabilize our results and provide us with more evidence on the effects of premedication on intraoperative bleeding and hemodynamic indices.
Conclusion
We concluded that clonidine was superior to promethazine and morphine in inducing hypertension, reducing blood loss, and providing better vision for the surgeons. Surgeon’s satisfaction was considerably higher when clonidine was used. Therefore, as all these factors have an impact on the overall outcome of the surgeries, we recommend that clonidine is used as a premedication in rhinoplasty
Acknowledgments
The authors would like to thank the staff of ENT clinic of Valie- Asr Hospital for their help toward conducting this study
References
- Rudy SF, Most SP (2017) Rhinoplasty. JAMA 318(14): 1406-1406.
- Motamedi MHK, Ebrahimi A, Shams A, Nejadsarvari N (2016) Health and social problems of rhinoplasty in Iran 5(1): 75-76.
- Akbari Sari A, Babashahy S, Olyaeimanesh A, Rashidian A (2012) Estimating the frequency and rate of first 50 common types of invasive procedures in iran healthcare system. Iranian journal of public health 41(10): 60-64.
- Rastmanesh R, Gluck ME, Shadman Z (2009) Comparison of body dissatisfaction and cosmetic rhinoplasty with levels of veil practicing in Islamic women. The International journal of eating disorders 42(4): 339-345.
- Tuncel U, Turan A, Bayraktar MA, Erkorkmaz U, Kostakoglu N (2013) Efficacy of dexamethasone with controlled hypotension on intraoperative bleeding, postoperative oedema and ecchymosis in rhinoplasty 41(2): 124-128.
- Ghadimi K, Levy J, Welsby IJ (2016) Perioperative management of the bleeding patient. Br J Anaesth 117(suppl_3): iii18-iii30.
- Marietta M, Facchini L, Pedrazzi P, Busani S, Torelli G (2006) Pathophysiology of bleeding in surgery. Transplantation proceedings 38(3): 812-814.
- Wormald PJ (2005) A three-dimensional reconstruction, techniques. The surgical field in endoscopic sinus surgery p. 7-12.
- Hunts JH, Patrinely JR, Stal S (1996) Orbital hemorrhage during rhinoplasty. Annals of plastic surgery 37(6): 618-623.
- Cochran CS, Landecker A (2008) Prevention and management of rhinoplasty complications. Plastic and reconstructive surgery 122(2): 60e-67e.
- Eftekharian HR, Rajabzadeh Z (2016) The Efficacy of Preoperative Oral Tranexamic Acid on Intraoperative Bleeding During Rhinoplasty. The Journal of craniofacial surgery 27(1): 97-100.
- Miller RD (2010) Anesthesia. 7th Philadelphia, US.
- Dakir A, Ramalingam B, Ebenezer V, Dhanavelu P (2014) Efficacy of Tranexamic Acid in Reducing Blood Loss during Maxillofacial Trauma Surgery-A Pilot Study. Journal of Clinical and Diagnostic Research: JCDR 8(5): ZC06-ZC08.
- Nishina K, Mikawa K, Uesugi T, Obara H, Maekawa M, et al. (2002) Efficacy of clonidine for prevention of perioperative myocardial ischemia: a critical appraisal and meta-analysis of the literature. Anesthesiology 96(2): 323-329.
- Patel J, Thosani R, Kothari J, Garg P, Pandya H (2016) Clonidine and ketamine for stable hemodynamics in off-pump coronary artery bypass. Asian cardiovascular & thoracic annals 24(7): 638-646.
- Lewis SR, Nicholson A, Smith AF, Alderson P (2015) Alpha-2 adrenergic agonists for the prevention of shivering following general anaesthesia. The Cochrane database of systematic reviews 8: Cd011107.
- Cormack JR, Orme RM, Costello TG (2005) The role of alpha2-agonists in neurosurgery. Journal of clinical neuroscience 12(4): 375-378.
- Welfringer P, Manel J, Garric J (1992) Clonidine premedication and isoflurane anesthesia to reduce bleeding in otologic surgery. Ann Fr Anesth Reanim 11(2): 125-131.
- El Hay O, Abo El Enin M, Hamada M, Ahmed A (2015) A comparative study between midazolam, promethazine, and chloral hydrate as oral premedication in pediatric patients. Ain-Shams J Anaesthesiol 8(1): 56-63.
- Cheah JW, Sing DC, Hansen EN, Aleshi P, Vail TP (2018) Does Intrathecal Morphine in Spinal Anesthesia Have a Role in Modern Multimodal Analgesia for Primary Total Joint Arthroplasty? The Journal of arthroplasty 33(6): 1693-1698.
- Ydemann M, Nielsen BN, Wetterslev J, Henneberg S, Lauritsen T, et al. Effect of clonidine to prevent agitation in children after sevoflurane anaesthesia: a randomised placebo controlled multicentre trial. Danish medical journal 63(6).
- Dahmani S, Brasher C, Stany I, Golmard J, Skhiri A, et al. (2010) Premedication with clonidine is superior to benzodiazepines. A meta-analysis of published studies. Acta anaesthesiologica Scandinavica 54(4): 397-402.
- Sung CS, Lin SH, Chan KH, Chang WK, Chow LH, et al. (2000) Effect of oral clonidine premedication on perioperative hemodynamic response and postoperative analgesic requirement for patients undergoing laparoscopic cholecystectomy 38(1): 23-30.
- Jabalameli M, Hashemi S, Soltani H, Hashemi SJJ (2005) Oral clonidine premedication decreases intraoperative bleeding in patients undergoing endoscopic sinus surgery. Journal of Research in Medical Sciences 10(1): 25-30.
- Oifa S, Sydoruk T, White I, Ekstein MP, Marouani N, et al. (2009) Effects of intravenous patient-controlled analgesia with buprenorphine and morphine alone and in combination during the first 12 postoperative hours: a randomized, double-blind, four-arm trial in adults undergoing abdominal surgery. Clin Ther 31(3): 527-541.
- Tarkkila P, Torn K, Tuominen M, Lindgren L (1995) Premedication with promethazine and transdermal scopolamine reduces the incidence of nausea and vomiting after intrathecal morphine. Acta anaesthesiologica Scandinavica 39(7): 983-986.
- Cardesin A, Pontes C, Rosell R, Escamilla Y, Marco J, et al. (2015) A randomized double-blind clinical trial to compare surgical field bleeding during endoscopic sinus surgery with clonidine-based or remifentanil-based hypotensive anaesthesia 53(2): 107-115.
- Masud M, Yeasmeen S, Haque A, Jahan S, Saha N (2017) Role of Oral Clonidine Premedication on Intra-operative Haemodynamics and PONV in Laparoscopic Cholecystectomy 26(4): 913-920.
- Engelman E, Lipszyc M, Gilbart E, Der Linden Van P, Bellens B, et al. (1989) Effects of clonidine on anesthetic drug requirements and hemodynamic response during aortic surgery. Anesthesiology 71(2): 178-187.
- Maze MJA (1991) Alpha-2 adrenoceptor agonists, Defining the role in clinical anesthesia. Anesthesiology 74(3): 581-605.
- Ghazipour A, Ahmadi K, Sarafraz M, Abshirini H, Akbari N (2013) Can clonidine as a pre-anaesthetic drug decrease bleeding during rhinoplasty surgery? Indian journal of otolaryngology and head and neck surgery 65(Suppl 2): 301-303.
- Woodcock T, Millard R, Dixon J, Prys Roberts C (1988) Clonidine premedication for isoflurane-induced hypotension: sympathoadrenal responses and a computer-controlled assessment of the vapour requirement. Br J Anaesth 60(4): 388-394.






























