Perioperative Management of Wounds in Combat Area
Barboza Denis1*, Sow O2, Diedhiou M4, Diagne Lo S2, Gaye I1, Diop NS2, Ndiaye B2, Diouf E3
1Anesthesia & Resuscitation Department, Peace Hospital, Faculty of Health Sciences, Assane SECK University, Ziguinchor, Senegal
2Inter Army Medical Center of Ziguinchor, Senegal
3Anesthesia and Resuscitation Department, Aristide Le Dantec Hospital, Cheikh Anta Diop University, Dakar, Senegal
4 Anesthesia and Resuscitation Department, Regional Hospital of Saint Louis, Faculty of Health Sciences, Gaston BERGER University, Saint Louis, Senegal
Submission: June 11, 2018; Published: July 12, 2018
*Corresponding author: Barboza Denis, Anesthesia & Resuscitation Department, Peace Hospital, Faculty of Health Sciences, Assane SECK University, Ziguinchor, Senegal.
How to cite this article: Barboza Denis, Sow O, Diédhiou M, Diagne Lô S, Gaye I, et al. Perioperative Management of Wounds in Combat Area. J Anest & Inten Care Med. 2018; 7(1): 555705. DOI: 10.19080/JAICM.2018.07.555705
Abstract
Gunshot wounds are among the most traumatic injuries. It is difficult to assess the extent of damages caused by a bullet and these are usually far too serious to be treated with a first aid kit. That’s why the best option is to bring the victim to the hospital as soon as possible. Our study focuses on the victims during the raking operation in the southern zone. This was a retrospective and descriptive study ranging from the period of 7th of January 2018 to April 8th 2018. Were included all patients with gunshot wounds. The following parameters were studied: age, type of injury, delay of transfer, clinical and paraclinical data, perioperative management and short-term evolution. In total there were four victims, whose care was taken in the Inter-army Medical Center of Ziguinchor. There were two casualties by 12.7mm caliber firearms incidents and the others were injured by AK 47. The injuries were located in the lower limb for three of the victims and in the head for the fourth who had died in the field. Two patients had undergone surgery preceded by preoperative preparation. One patient was severely injured and had several transfusions. The medical evacuation by air was made as soon as possible to the level III hospital.
Keywords: Anesthesia; Wounds; Combat area; Ziguinchor
Background
Gunshot wounds are among the most traumatic injuries. It is difficult to assess the extent of damages caused by a bullet and these are usually too serious to be treated with a first aid kit. The protective items of the fighter, Kevlar helmet, vests, have shown their effectiveness in transforming the nature of combat injuries [1]. The health services of the armed forces have organized several levels of care for the war wounded in operations. The best option is to bring the victim to the hospital as soon as possible. Hemorrhage is the leading cause of death, representing a significant rate of “preventable” deaths. While there is consensus on intraoperative resuscitation of the bleeding hemorrhagic patient, the preoperative strategy is not unambiguous [2]. We considered it necessary to have accurate data on the mechanisms and severity of the injuries, the diagnostic and therapeutic difficulties encountered, the morbidity and the mortality of the wounded in order to better guide the research programs and to improve the prevention of injuries and their treatment. Considering the early death cases, the evacuation time is of fundamental importance, partly conditioning the mortality on the battlefield. However, final care takes place in the structures of the back. Our study focused on the care of victims during search operations of the Senegalese army (Casamance).
Equipment and Methods
This was a retrospective and descriptive study ranging from the period of 7th of January 2018 to April 8th 2018. All patients with gunshot wounds were included. The management strategy was to transfer casualties from the battlefield to the advanced command post. Then they were evacuated to the medical center for the first surgical procedures including hemodynamic stabilization and finally evacuated to the level III hospital by air. The team of the battalion’s medical and surgical center consisted of an anesthetist-intensive care physician, senior technicians in anesthesia, surgeons and block nurses. The center has been operational since 2015. It houses two operating rooms each with an anesthesia machine, a multiparameter scope, a surgical table and anesthesia drugs. It also has a chop room, with a cart containing emergency drugs, an X-ray room and an ultrasound machine. The parameters studied were age, type of injury, transfer delay, clinical and paraclinical data, perioperative management and short-term evolution.
Results
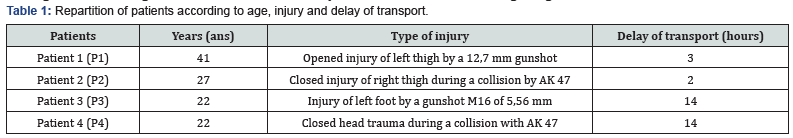
Four gunshot victims were taken care of at the center. There were three lower limb injuries: two per 12.7mm caliber and 5.56mm (M16) firearms and one by AK 47 firearm. The fourth victim had a head injury with an AK 47 weapon (Table 1). Patient P1 arrived three hours after the incident. He was conscious and hemodynamically unstable. He had a tourniquet and compressive bandage in the left thigh, which had been removed by ablation with muscle and bone lesions (Figure 1). Sensitivity and motor skills were abolished. Blood tests found anemia (Table 2). The X-ray showed a bifocal fracture common to the union of the upper and middle thirds of the thigh. The patient was admitted to the block for trimming and glued traction.

Patient P2 was received two hours after injury. He was conscious and hemodynamically stable and had a tourniquet at the right thigh and a compressive bandage. At removal of the tourniquet and dressing, we noted an internal punctiform inlet port and an external outlet of two centimeters with perceived peripheral pulses and without impairing sensitivity or motor skills (Figure 2). The preoperative assessment was normal (Table 2) and the X-ray found a displaced fracture of the middle third of the right femur. He was admitted to the block for trimming and glued traction.


Pl: Platelets; WBC: White Blood Cells; Hg: Haemoglobin; AP: Arterial Tension; PS: Physiological Saline; Creat: Creatininemia; PT: Prothrombine Time; HR: Heart Rate; BPM: Beats Per Minute.
Patient P3 had trauma to the right foot per shooting incident. At admission, the patient was conscious and presented a dorsal, linear, three centimeter regular-edged wound and a punctiform outlet on the plantar surface (Figure 3). There were no sensory or mobility disorders. The X-ray revealed an incomplete fracture of the base of the second phalanx of the second toe. Wound trimming and suture had been performed. Patient P4 had died with a parietal bullet wound with irregular edges caused by a bullet. All three patients received antitetanus serum. P1 and P2 had undergone preoperative preparation (Table 2). The evolution was favorable in two patients (P2 and P3). However, one patient (P1) presented a severe anemia requiring postoperative transfusion. The medical evacuation by air was made for the two thigh wounded to a level III hospital within four hours.

Discussion
Ballistic trauma is a transfer of energy between a moving projectile and the body. Several tissue factors play an important role in the morphology of the injuries observed, particularly the density and elasticity of the tissues involved in the trauma. The higher the tissue density and the lower their elasticity, the greater the energy transfer is. However, the severity of the injury will depend more on the affected organ than the type of wounding projectile. In our study, three of the received victims had lower limb injuries. They are the most frequent locations [3,4]. The functional prognosis is mainly related to the risk of amputation, which is 28% [4], related to osteoarticular lesions. Vascular lesions occur in 2.5% of cases in limb trauma. These lesions are not assessable in the field whence the interest of an evacuation in the shortest time. The transfer delay for the two seriously injured (P1 and P2) with the tourniquet was 3 hours and 2 hours, respectively. This long delay is explained by the fact that the evacuations were carried out during a war that is characterized by long periods of evacuation. The tourniquet can cause ischemia. Similarly it can kill the wounded by the revascularization syndrome of Cormier and Legrain or Bywatters and Beall [5]. Thus a wounded with a tourniquet is a casualty of extreme urgency (Figure 4).

The use of the tourniquet requires a balance between the vital prognosis and the functional prognosis because the tourniquet has saved more life, said Leriche, that it has cost of limb. The severity of a ballistic injury depends on its clinical impact, the site of the lesion or the mechanism of injury. For example, unstable hemodynamic injuries, injuries to the neck, trunk and in particular the heart area, the groin area, as well as injuries sustained by high-velocity bullets or hunting guns at short distance, must be transported as quickly as possible to the operating room for a prospective surgical procedure while continuing resuscitation. Perioperative management has allowed us to do hemodynamic stabilization, haemostasis and medical evacuation in the shortest possible time for our patients. Emergency surgical procedures often require filling and massive transfusions, which are of great importance in ballistic trauma [6,7]. It is thus necessary to be able to dispose rapidly of erythrocyte concentrates, then secondarily of platelets and fresh frozen plasma.
However, the beneficial effect in terms of survival of preoperative massive filling by crystalloid or colloid solutions before surgical hemostasis is controversial. Some authors [8] recommend initial contributions limited to the maintenance of a minimum hemodynamic balance before the passage in the operating room. The filling was limited because our patients had benefited from the installation of a tourniquet and a compressive bandage from the place of the incident. On the anesthetic level there is no ideal agent. As with closed trauma, the choice will depend on the clinical condition of the injured person, the site of the injury, the urgency of the situation and the type of intervention. Both P1 and P2 patients had spinal anesthesia. Management of arterial hypotension, hemostasis disorders, bleeding, hypothermia and their consequences are the main tasks of the anesthetist [2].
In our study both patients had benefited from vascular filling. But only P1 patient with peri-operative hemorrhagic shock was transfused. The vital prognosis is function of exsanguination but also of the seat of the lesion. Injuries to the feet or hands are usually less life-threatening. The fourth victim died instantly because he had received a bullet at the skull. Head injuries caused by firearms are serious, life-threatening injuries. In fact, cephalic lesions have a heavy mortality of more than 80% [9]. Both P1 and P2 patients received third-generation cephalosporin antibiotic prophylaxis. Prevention of infection is a key element in the management of ballistic trauma. Although early mortality has greatly decreased thanks to optimization of initial care (resuscitation, surgery), infection remains the leading cause of secondary mortality [2]. The optimal care should go through the improvement of the tools of protection, the good control and better handling of the weapons, the reduction of the time of evacuation by the availability of adequate logistical means, the reinforcement in human and material resources, in particular: scanner , MRI, blood bank with availability of labile blood products, external fixator and resuscitation equipment.
Conclusion
Quote from France’s 2008 White Paper on Defense and National Security: Protecting the Forces is not only a human imperative, but also a strategic necessity to maintain adherence and tactics to ensure success. Health support is a moral obligation that the State undertakes with respect to its nationals, especially when faced with increased risk.
References
- Pasquier P, De Rudnicki S, Donat N (2011) Epidemiology of war injuries, about two conflicts: Iraq and Afghanistan. Ann Fr Anesth Reanim 30(11): 819-827.
- Rouvier B, Lenoir B, Rigal SL (1997) Ballistics traumas. Elsevier Actualisation Conferences, Paris pp. 703-716.
- Haus Cheymola R, Bouguerra C, Mayorga E (2011) Blessures par arme à feu et engins explosifs dans les armées. Résultats de la surveillance épidémiologique de 2004 à 2008. Gunshor injuries in french military population : results of the 2004-2008 public health surveillance. Medicine and army 39(1): 89-96.
- Crey ME (1996) Analysis of wounds incurred by US Army Seventh Corps Personnel treated in Corps hospital during Operation Desert Storm, February 20 to March 10, 1991. J Trauma 40(3): 165-169.
- Larcan A, Mathieu P, Helmer J (1973) Proceedings: Severe metabolic changes following delayed revascularization: Legrain-Cormier syndrome. The Journal of cardiovascular surgery 14(6): 609-614.
- Shanin IN, Shanin VI (1993) Anesthesia in severe combined gunshot and mine blast injuries. Vestn Khir Im II Grek 150(3-4): 65-68.
- Takauchi Y, Abe K, Demizu A (1994) Anesthetic management for emergency operation in seven patients with gunshot injury. Masui 43(1): 111-115.
- Bickell WA, Wall MJ, Pepe PE, Martin RR, Ginger VF, et al. (1994) Immediate versus delayed fluid, resuscitation for hypotensive patients with penetrating torso injuries. N Engl J Med 331: 1105-1109
- Parsons TW, Laverman WC, Ethier DB, Gormley W, Cain JE, et al. (1993) Spine injuries in combat troop Panama, 1989. Mil Med 158(7): 501- 502.






























