Epiglottitis and Complicated Epiglottitis – A Narrative Review
Joe Jabbour1*, Sarah Lorger1, Chris Milross2, Ranga Sirigiri1 and Hayder Ridha1
1Department of ENT, Dubbo Base Hospital, Australia
2Central Clinical School, University of Sydney, Australia
Submission: February 05, 2021;Published: February 22, 2021
*Corresponding author: Joe Jabbour, Department of ENT, Dubbo Base Hospital, Dubbo, NSW, 2830, Australia
How to cite this article: Joe J, Sarah L, Chris M, Ranga S, Hayder R. Epiglottitis and Complicated Epiglottitis – A Narrative Review. Glob J Oto, 2021; 24 (1): 556130. DOI: 10.19080/GJO.2021.24.556130
Abstract
Epiglottitis is a life-threatening emergency if not diagnosed early and managed by a multi-disciplinary approach. Early symptoms and signs are used to diagnose epiglottitis. Imaging can be helpful if clinically safe to perform and supported by close monitoring. Imaging is an adjunct if the airway is patent and with close monitoring. Despite decreasing incidence of epiglottitis in children secondary to vaccination, there is an increasing incidence of epiglottitis and epiglottic abscess formation in adults over the last two decades. Management involves establishing an airway, broad spectrum antibiotics and possible surgical management of complicated epiglottic abscess. We aimed to systematically review the literature to provide a succinct overview on workup and treatment of epiglottitis and its complications.
Keywords: Epiglottitis; Epiglottis abscess; Airway management; Antibiotics
Methods
A systematic search of Medline Ovid, PsychINFO and CINAHL databases was conducted for the period January 1946 to October 2020. Mesh terms used were “epiglottitis” AND “complications”. Article titles and abstracts were independently screened for inclusion by one author.
Definition
Epiglottitis is cellulitis and/or infection of the epiglottis and surrounding nearby structures like the arytenoids, aryepiglottic folds and vallecula. It is more correctly called supraglottitis. Complicated epiglottitis usually involves a coalescent abscess containing pus in the supraglottic region in the oropharynx [1]. Other rare and uncommon complications of epiglottitis include descending necrotizing mediastinitis [2].
Aetiology
Epiglottitis can be infectious, or noninfectious. Infectious causes can be bacterial, viral, or fungal. The most common cause is Haemophilus influenzae type B (HIB), although the incidence of epiglottitis has dropped significantly due to the introduction of the HIB vaccine in many countries [3-7]. In children, HIB is a common organism, however in adults’ other pathogenic bacteria include Klebsiella pneumoniae, Streptococcus pneumoniae and Staphylococcus aureus [8]. Immunocompromised patients are susceptible to Pseudomonas aeruginosa and Candida. Noninfectious causes are mainly traumatic such as corrosive, thermal or foreign body ingestion [9-11].
Epidemiology
Epiglottitis usually affects children under the age of 6, however currently there is an increasing incidence in adults [12]. The introduction of the HIB vaccination in 1985 has resulted in decreased annual incidence in children over the last decades to less than one case per 100, 000 from 59 cases per 100, 000 [6,13]. In adults the incidence has increased from 0.88 (from 1986-1990) to 3.1 (from 1996-2000) per 100, 000 [8]. Concomitantly the number of epiglottic abscesses or complicated epiglottitis has increased with incidence of epiglottitis. The mortality rate in adults has been reported as 7.1% [7]. Moreover, the age of children with epiglottitis has increased from 3 years of age to 6-12 years old post vaccination schedules [14]. In adults the age of presentation of epiglottitis is in the 4th decade of life with a male predilection of 2.5:1 [15].
Pathophysiology
The anatomy of the airway and physiological differences between children and adults may explain the difference in pathology presentation. In children anatomically, the epiglottis is located anteriorly and superiorly with an oblique angle to the trachea. The cartilage of the epiglottis in children is composed of pliant cartilage compared to the rigid cartilage of the adult. Thus, in children, oedema and swelling of the epiglottis caused by bacterial infection leads to an increase in the weight and mass of the epiglottis causing an oedematous epiglottis to cover the laryngeal airway on inspiration (ball-valve effect) causing symptoms. In comparison, a rigid and stiffer epiglottis and laryngeal cartilages in adults may resist the increase in epiglottic mass due to infection, however surrounding supraglottic oedema can manifest in symptoms and an unstable airway. The most common bacterial organism causing oedema of the epiglottis is HIB in children and adults leading to symptoms of airway obstruction. Other organisms such as S. pneumoniae, S. aureus and beta-hemolytic Streptococcus sp. are important pathogens in adults.
Symptoms and Signs
Symptoms initially appear very mild for a period of hours to days then rapidly worsen to a sudden onset of symptoms. In children, they usually present with a generalized toxemia of a fever (temperature above 38.5 degrees Celsius), dysphagia, difficulty moving the neck downward and stridor (usually inspiratory). As the infection progresses the child may sit upright leaning forward in a tripod position with their mouth open, tachypnoea and drooling as they are unable to swallow their saliva secondary to difficulty or pain [12]. Sometimes other subtle respiratory symptoms may include orthopnoea and a muffled voice. Croup may also present with fevers, stridor and dyspnoea. However, croup is usually associated with a gradual increase in symptoms over a couple of days in addition to a cough described as “barking” usually without the development of drooling [16]. In adults, supraglottitis usually presents predominately with symptoms of odynophagia (100%), dysphagia (85%) and dysphonia (74%) [17].
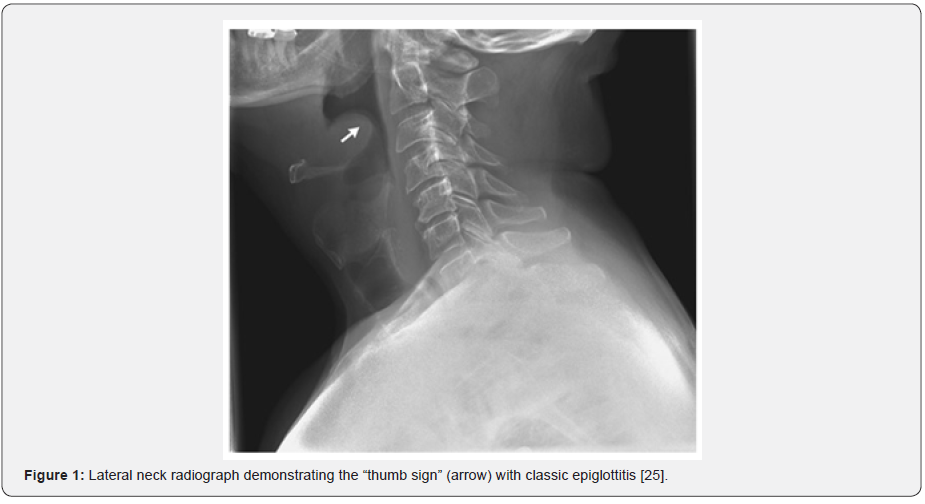
Diagnosis
The diagnosis of epiglottitis is primarily a clinical diagnosis. Avoiding instrumenting the oropharynx during examination will reduce progression of epiglottic oedema leading to potential airway disaster. A lateral neck radiograph may show swelling of the epiglottis due to epiglottic fold oedema called “thumb sign” (Figure 1) [18]. The radiograph is not necessary, although can be used to eliminate differential diagnoses (epiglottic abscess, parapharyngeal abscess, or retropharyngeal abscess). Imaging is performed in hemodynamically stable and cooperative patients. Adults may have obliteration of the vallecula known as the “vallecula sign” from an oedematous epiglottis [19]. Flexible laryngoscopy is best completed in a safe and controlled setting such as the operating theatre as there may be a risk of laryngospasm and imminent airway obstruction. Once a clinical diagnosis of epiglottitis is made, the patient needs to be transferred to the operating room for airway examination. In an adult, indirect, direct, and flexible laryngoscopies are accurate, safe and have not been demonstrated to exacerbate airway obstruction [18].
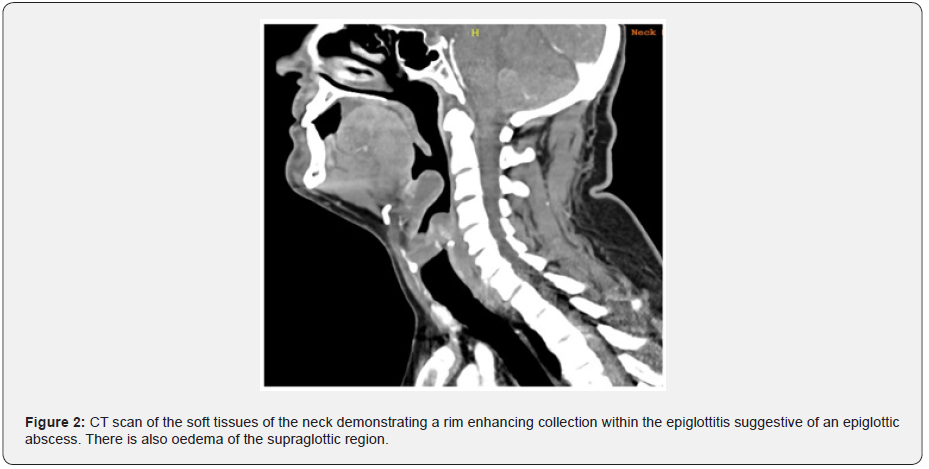
Complicated epiglottitis in the form of an epiglottic abscess may necessitate further CT scan of the soft tissues of the neck to investigate for a deep neck space abscess. The patient should be accompanied by an otolaryngologist or anesthetist to the radiology department to ensure airway monitoring and prevent a respiratory crisis. CT findings suggestive of an epiglottic abscess include a rim enhancing low density collection within the epiglottis (Figure 2). A complete blood count and differential, blood and throat cultures can be obtained once the airway is secured. Usually, blood and throat cultures are negative and rarely change clinical management. Ultrasonography has been described as a method to evaluate patients by visualizing an “alphabet P sign” in longitudinal view through the thyrohyoid membrane [20]. Although a stable clinical condition is advised prior to instrumentation of the ultrasound probe alongside the neck in children with suspected epiglottitis.
Management-anesthetic and surgical considerations
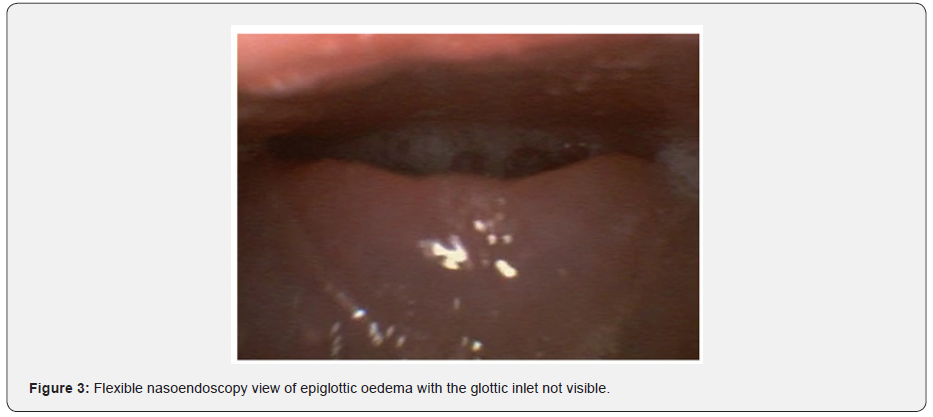
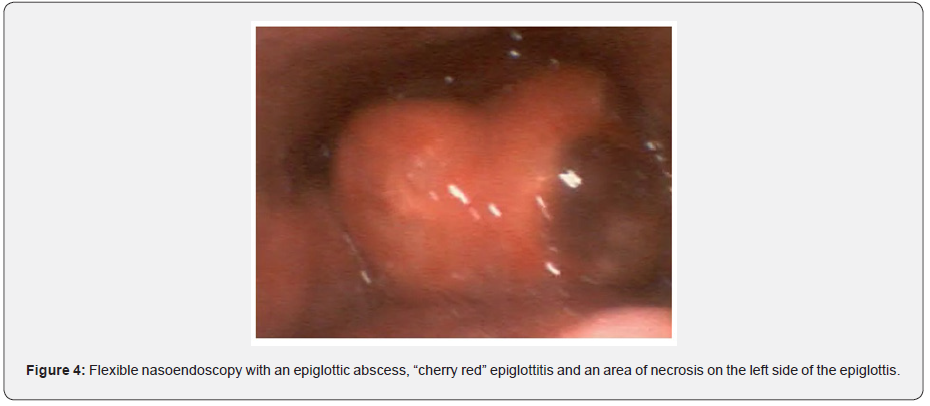
Securing the airway is the most important management of an epiglottitis in both children and adults. This needs to be performed by an experienced team including an anesthetist, otolaryngologist and intensivist because intubation may be a potentially difficult procedure (Figure 3) especially in complicated epiglottitis. Airway intervention is more likely to occur in children compared to adults [18]. To ensure safe airway intervention this should be conducted in an operating room under monitoring. In children once the diagnosis of epiglottitis is confirmed, they need to remain erect, even sitting on their parents’ laps. This is followed by an inhalation induction of general anesthesia to ensure spontaneous ventilation and avoid complications of asleep intubation and inability to secure the airway [21]. A flexible video laryngoscopy, a difficult airway trolley and a tracheostomy tray must be set up at the bedside. Paralytic agents of skeletal muscle should be avoided to prevent cessation of spontaneous ventilation and increased risk of a surgical airway. The trachea in children can usually be anesthetized with a deep inhalation agent. Although the time necessary for deep anaesthesia may be increased due to airway obstruction. Capnography monitoring of exhaled gas analysis is useful in determining the depth of anaesthesia (Figure 4).
Fiberoptic awake nasotracheal intubation is the preferred method of securing the airway to avoid accidental extubation which could be disastrous [21]. The type of endotracheal tube used (cuffed or uncuffed) and size depend on the patient’s age. However, to prevent subglottic stenosis, there needs to be an air leak at 20cm H2O. Once intubated an examination for complicated epiglottitis is made and if there is an epiglottic abscess it is drained with the pus sent for a culture swab. Once the airway is secured and any complication of epiglottitis managed, the patient is transferred to the intensive care unit (ICU) for ongoing antibiotics (second or third generation cephalosporins). If there is an immediate hypersensitivity allergy to penicillin, then levofloxacin or moxifloxacin can be used. Most pediatric intensivists consider extubation within 24 to 48 hours once the toxemia has resolved. An air leak needs to be demonstrated once the endotracheal cuff is deflated to consider readiness of extubating [22]. Moreover, a second direct laryngoscopy with deep sedation or general anaesthesia may be needed to assess the extent of epiglottic oedema or assess for new complicated epiglottitis. Corticosteroids are administered during the admission reduce pharyngeal and epiglottic oedema and have been associated with shorter ICU and overall length of stay [17].
Adults in contrast may present with supraglottitis with varied severity and management should be tailored to the presentation. Mild to moderate cases without symptoms of respiratory compromise can be managed with medical management with vigilant airway monitoring. Emergent airway intervention with intubation or tracheostomy occurs in approximately 11% of cases [23]. Symptoms of respiratory distress, stridor, tachycardia, and tachypnoea warrant prompt airway management. Securing the airway in an adult involves high-flow nasal prong oxygenation, fiberoptic nasoendoscopic application of topical anaesthesia with light sedation and subsequent intubation whilst awake [24].
Non-surgical management
All non-intubated patients are monitored in a high-vigilance area with continuous pulse oximetry, parenteral antibiotics as discussed above and a tracheostomy tray available at the bedside. Despite a patient being allocated non-surgical management, communication between the otolaryngology team and anesthetist are required early in the event of an emergency airway being required in the form of intubation or a tracheostomy in the operating room.
Limitations and future research
The main limitation of this review is that most of the literature are case reports due to the infrequent presentation of complicated epiglottitis. Furthermore, assessing validity and quality is challenging when assessing the data. Future research is needed when comparing the outcomes of complicated epiglottitis management in the adult and pediatric populations in tertiary centers with large patient presentations.
Conclusion
Epiglottitis and complicated epiglottitis require high clinical suspicion and rapid intervention to avoid life-threatening airway obstruction. The disease presentation in children and adults varies with different degrees of respiratory compromise. Airway management is a priority over investigations and should be secured in a controlled setting such as the operating room with experienced anaesthetic and otolaryngology providers.
Author Contribution
Joe Jabbour contributed to conception, design, collection and assembly of data, manuscript writing and final approval of manuscript. Sarah Lorger, Ranga Sirigiri, Chris Milross and Hayder Ridha contributed to manuscript writing and final approval of manuscript.
References
- Smith R, P Loizou, M Smith (2017) Epiglottic abscess and the management of a ‘precious airway’: A case study. Otorhinolaryngol Head Neck Surg 2.
- Huopio M, Jukka Kokkonen, Sirkku Heino, Mika Valtonen, Tapio Hakala (2014) Epiglottitis and necrotizing mediastinitis in a middle-aged man. Duodecim 130(5): 503-506.
- Alho O P, K Jokinen, T Pirilä, A Ilo, H Oja (1995) Acute epiglottitis and infant conjugate Haemophilus influenzae type b vaccination in northern Finland. Arch Otolaryngol Head Neck Surg 121(8): 898-902.
- Frantz T D, B M Rasgon, C P Quesenberry (1994) Acute epiglottitis in adults. Analysis of 129 cases. JAMA 272(17): 1358-1360.
- Ryan M, M Hunt, T Snowberger (1992) A changing pattern of epiglottitis. Clin Pediatr (Phila) 31(9): 532-535.
- Takala A K, H Peltola, J Eskola (1994) Disappearance of epiglottitis during large-scale vaccination with Haemophilus influenzae type B conjugate vaccine among children in Finland. Laryngoscope 104(6): 731-735.
- Garpenholt O, S Hugosson, H Fredlund, L Bodin, P Olcén (1999) Epiglottitis in Sweden before and after introduction of vaccination against Haemophilus influenzae type b. Pediatr Infect Dis J 18(6): 490-493.
- Berger G, Tali Landau, Sivan Berger, Yehuda Finkelstein, Joelle Bernheim, et al. (2003) The Rising Incidence of Adult Acute Epiglottitis and Epiglottic Abscess. Am J Otolaryngol 24: 374-383.
- Chen C, Mukil Natarajan, David Bianchi, Georg Aue, John H Powers (2018) Acute Epiglottitis in the Immunocompromised Host: Case Report and Review of the Literature. Open Forum Infect Dis 5(3): ofy038.
- Schröder A S, C Edler, J P Sperhake (2018) Sudden death from acute epiglottitis in a toddler. Forensic Sci Med Pathol 14(4): 555-557.
- Tsai Y T, Ethan I Huang, Geng He Chang, Ming Shao Tsai, Cheng Ming Hsu, et al. (2018) Risk of acute epiglottitis in patients with preexisting diabetes mellitus: A population-based case-control study. PLoS One 13(6): e0199036.
- Baiu I, E Melendez (2019) Epiglottitis. JAMA 321(19): 1946-1946.
- Gilbert G L, D A Clements, S J Broughton (1990) Haemophilus influenzae type b infections in Victoria, Australia, 1985 to 1987. Pediatr Infect Dis J 9(4): 252-257.
- Butler D F, A L Myers (2018) Changing Epidemiology of Haemophilus influenzae in Children. Infect Dis Clin North Am 32(1): 119-128.
- Al Qudah M, S Shetty, M Alomari, Maen Alqdah (2010) Acute adult supraglottitis: current management and treatment. South Med J 103(8): 800-804.
- Tibballs J, T Watson (2011) Symptoms and signs differentiating croup and epiglottitis. J Paediatr Child Health 47(3): 77-82.
- Guardiani E, M Bliss, E Harley (2010) Supraglottitis in the era following widespread immunization against Haemophilus influenzae type B: evolving principles in diagnosis and management. Laryngoscope 120(11): 2183-2188.
- Lichtor J L, Maricarmen Roche Rodriguez, Nicole L Aaronson, Todd Spock, T Rob Goodman, Eric D Baum (2016) Epiglottitis: It Hasn’t Gone Away. Anesthesiology 124(6): 1404-1407.
- Chung C H (2002) Adult acute epiglottitis and foreign body in the throat - chicken or egg? Eur J Emerg Med 9(2): 167-169.
- Hung T Y, Shang Li, Po Shen Chen, Liang Ting Wu, Yuh Jeng Yang, et al. (2011) Bedside ultrasonography as a safe and effective tool to diagnose acute epiglottitis. Am J Emerg Med 29(3): 359.e1-3.
- Lindquist B, S Zachariah, A Kulkarni (2017) Adult Epiglottitis: A Case Series. Perm J 21: 16-089.
- Mhanna M J, Ingrid M Anderson, Narayan P Iyer, Amy Baumann (2014) The use of extubation readiness parameters: a survey of pediatric critical care physicians. Respir Care 59(3): 334-339.
- Sideris A, Timothy R Holmes, Benjamin Cumming, Thomas Havas (2020) A systematic review and meta-analysis of predictors of airway intervention in adult epiglottitis. Laryngoscope 130(2): 465-473.
- Mathoera R B, P C Wever, F R C van Dorsten, S G T Balter, C P C de Jager (2008) Epiglottitis in the adult patient. Neth J Med 66(9): 373-377.
- Grover C (2011) ”Thumb Sign” of Epiglottitis. N Engl J Med 365(5): 447-447.





























