Chronic Nasal Obstruction & Snore
Novak Vukoje1 and Jon Garito2*
1ENT office “dr Vukoje" Petrovaradin, Serbia
2PhD, Inventer the dual Frequency device and the RFelectrodes, USA
Submission: July 25, 2017; Published: August 04, 2017
*Corresponding author: Jon Garito, PhD, Inventer the dual Frequency device and the RF electrodes, 1111 Crandon, BLVD, FL 33149, USA, Tel: 516 375 7204; Email: drjgarito@aol.com
How to cite this article: Novak V, Jon G. Chronic Nasal Obstruction & Snore. Glob J Oto 2017; 9(3): 555763. DOI: 10.19080/GJO.2017.09.555763
Introduction
Numerous competent and scientific papers see connection between chronic nasal obstruction and frequency of loud sleep and split during breath. Narrowness of airway, collapsibility and bigger resistance of air flow are cognizable factors contributing to that syndrome. Loudness during breath can correlate with percentage of nose plug. To every very loud sleeper detailed clinical review of nose is recommended. Approximately, more than 40 per cent of snore-sleepers complain on hardship during breath through nose. Lot of inventions, gadgets and products that have been used as external or internal dilators of nostrils, reduce snore with bigger or smaller efficiency. Prevention of nostril wings collapse with 3-M band diminishes residence of airflow and, consequently, noise during sleep [1-3].
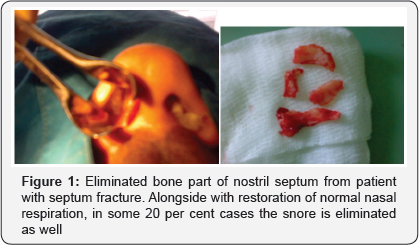
Application of steroids in lower nasal shell can secure silent night. Correct intervention on nasal occlusion confirms up said thesis. Studies that refer to polysomnograpric evaluation of intervention efficiency overtaken in nose and sleep quality, show that with elimination of pathological incorrectness and situation in that region level of noise during sleep is being reduced. With that, role of nose functioning in ronhopat pat physiology and apnea is confirmed (Figure 1). The more of pathology in nose is present; the surgical success is bigger, although degree of nose occlusion is not always in direct correlation with symptom graveness. By larging the diameter of nasal valve area and nose corridors level of sleeper for air turbulence, nasal resistance and collapse of upper breathing ways becomes smaller as well [4-6].
Today, more and more persons has chronic plugged nose. Due to air pollution, this is particularly recognized in bigger cities. This affection, called obstructive rinitis, is characterized by permanent bump in nasal inside, followed with feeling of obstructive breathing, postnasal rinorea, unpleasant odor from mouth, drying of mouth, pain in throat, disturbance of sense of smell, and also repeatable tonsil anginas and recidive sinusitis.
Intensity and frequency symptoms differ. Under oscillations of outside temperature and meteo - factors, they grow stronger. Accumulation of liquids around nasal valves and nose shells narrows nasal breathing space. By sleep on the rear, when snore usually becomes louder, so-called sleep-reflex is reduced. Nowhere without handkerchief...today, alergic rinitis is the most frequent reason of chronic nasal obstruction. Every fifth person suffers from some kind of excessive sensation on respiration allergens. During above-mentioned phases, snore is much more present [6-9].
Beside allergenic rinopathy, hypertrophy of lower nasal shells is considered to be one of the leading causes of hard breath through the nose and represent big therapeutic problem. If rinitis become refractive to local therapy that patients use for years in drops or spays, the only solution for them is surgical operation. The core of intervention is to avert hyperplasic mucous membrane. During sleep, mucosis of the region mentioned has predisposition to grow, affecting nasal respiration. In the situation when nose is partly or completely plugged, person has to breath stronger to bring the air in lungs. This is manifested by step-by-step rise of negative pressure in collapsible part of orofarincs and appearance of extensive vacuum in throat that pulls uvula and palate much deeper in the way of air [10,11].
Depending on obstruction scale, snore begins as independent symptom or in conjunction with night throttle syndrome. Snore is present even by persons who would not snore if they could easily breath. Except this pathology, that is, alongside with allergic rintis, the most frequent, there should not be avoided even hormonal and chronically infective rinitis that is more and more present in oto-rinology practice. The other endo-nasal pathological processes as are - malignant or benign tumors, polyps, papillioms, than, deviations or fractures of nostril wall, septo-conhinal synechies, stenosis of nostril walls, collapse of alar cartilages and alike, can also become reason of nostril obstruction. The connection between those diseases with snore has been recognized long time ago, and during recent decades completely explained. Resolving it, either by surgery or other means, one of the rings in pathophysiology of loud snore, sleeping apnea and hypoventilation of alveoli, will be split.
When nose is plugged rinosurgical intervention is recommended as part of routine snore therapy. It must be mentioned that surgical intervention on upper respiration way (nose) is rarely healing, but is imperative. There is no way to predict by whom of the patients this intervention on loud respiration will succeed. From correct end nasal operation we expect -
a) Much easier respiration
b) Reduction of noise during snore
c) Ease in apneatic frequency
d) Improved quality of sleep
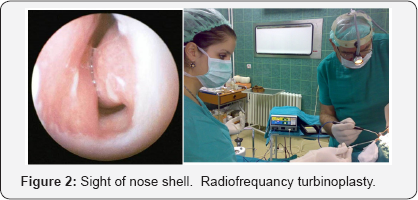
Up to now, to eliminate obstruction factor irritated by hyperplasia of konhi mucosis, the way was to get through surgical intervention under total anesthesia followed by risk of bleeding and tent-wick wear in nose during several days. That refers predominant on conventional techniques as are partial or total resection of lower nasal shells. As by-effect, some particles appear to fall from nose for weeks. Consequences and complications after mentioned interventions can appear in shapes of increases and scars that lead to secondary occlusion of nasal channels and lately to atrophic rinitis as well. With contemporary rinosurgery technology at hand, above mentioned complications could be avoided. New methods in submucosis konhoplastics are the leaders of our times (Figure 2).
Sub mucous conhoplastics with radio-wave (Ellman Surgitron 4.0 Dual) is technique that absolutely conserves quality and quantity of mucous membrane function, followed by quantity reduction of the same till the respectable level. Intervention is in local anesthesia, without complications and pain as well. The VAS scale shows permanent upheaval of patient's symptoms. Method is based upon principle of submukous melting of tissue of enlarged nose shells. By using appropriate electrodes that are placed under the mucous membrane of nose shells, several micro-thermal necrotic places are made, that during further process lead to scar changes and minimizing of conhi volumes. Reducing them, quantity and function of epitel is preserved, so that normal nasal respiration, as prerequisite of tranquil sleep, is made possible.
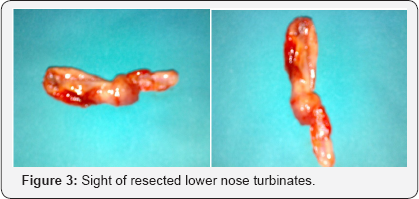
Earlier, classic and abound resections of abnormally grown lower nasal shells of turbinectonomia type often leaded to infection and inflammation of remaining bone tissue. More, inadequately decrease of volume of respiration epitel presents one more problem that patients are exposed to. Because of excessive destruction of functional tissue, using traditional methods, problems with respiration are often still persistent (Figure 3).
Recently, operation of nose shells is done with CO2 laser under the simple local anesthesia. One and only one intervention is enough for instant nose “uncork”. After laser treatment, patient does not feel any pain, has no epitax or tent-wick in nose, and soon after intervention he is ready for the job. The results of that kind of technique are stable, and in case of recidive, the procedure can be repeated.
There is no need to omit even the “cold” technique that uses special instrument with small cutting edge, with what the excess of hyperplasic tissue under the mucous membrane is eliminated. Minimum of risk from complications and, especially, absent of thermal effect on surrounding tissue, promises to this method great potential. Diminished volume of curves is visible immediately, and no signs of scare formations characteristic to other techniques are found. Thanks to one inbound point of only 2 mm diameter on the front part of lower nose shell, risk of bleeding is minimized. Mode of employment is simple. Patient is prepared for standard endonasal procedure in local anesthesia. Breed of instrument is firmly pushed towards the bone of lower nose shell, until mucous membrane is perforated. The sumucosis pocket is formed and tunneled from onward till backward, in circles. It can be seen when mucous stratum falls, and process is going on until the adequate diminishing of shell volume is being achieved.
In case of comprehensive hyperplasia of nose shells, one of up to date methods called "cold technique" is recommended. Future for it is bright thanks to cheap equipment and successes do not fail. Functional konhoplastics great success made that procedure very useful and there is no need to ignore it in context of general treatment of nasal obstruction as one of the etiologic factors of sleeping apnea and snore. Today, endonasal surgical interventions are done in classic manner, using the laser; radio- frequent energy etc. depending on equipment that doctor has at disposal. Of course, every patient prefers less painful and less aggressive method, without tent-wick and hospitalization, with the greatest success possible. For that goal, this latest, the most modern and less invasive techniques has been introduced. The times will show what of the techniques and technologies are most efficient and most comfortable (Figure 4).

Conclusion
Improvement of nasal respiration after endonasal procedure can have a positive impact on noisy sleep. With a certain number of noisy sleepers, this procedure alone significantly reduced or completely eliminated snoring. Rhino surgical procedures, despite the fact that all patients experience no beneficial effect on snoring, is recommended as a "primum moves" condition because without them subsequent surgeries at secondary level would not result in success. The relationship between the degree of nasal insufficiency, type of pathology and oral cavity configurations classified by Malampathiu should be considered in the prognoses of a effectiveness of surgical treatment. Our result indicate that score by Malampathiu is inversely correlated to surgical success. The author concludes that ronchopathy co-exist with chronically stuffed nose, nasal surgery should be considered as first-line surgical treatment of these patients and it should not be bypassed as part of a routine plan of treating this unpleasant symptom. Rynosurgical interventions are recommended as part of "cut for restful sleep" and standard therapy of snore, OSA and alveolar hypoventilation. In fact, after interventions sleeping is less divided and improved.
References
- Novak Vukoje: Rez za miran san. Medicinska knjiga. Izdavacka Knjizarnica Zorana Stojanovica. Sremski Karlovci 2008 g.
- Novak Vukoje: Hrkanje i slip apneja -uzroci i lecenje. Medicinska knjiga. Izdavac Maxima Graf. Petrovaradin 2015 g.
- Kiril Haralampijev i Novak Vukoje: Osnovi savremene otorinolaringologije, Udzbenik, Sajnos, Novi Sad, 2012 g.
- Novak Vukoje, Enoz M, Cventinov M, Laperia JF (2011) Arco-palato- uvular flap: a new surgical technique for the treatment of palatal. snoring in tonsillectomized patients, Kulak Burun Bogaz Ichtis Derg 21(5): 261-265.
- Verse Th (2002) Effect of nasal surgery on sleep releted breathing disorders. Laryngoscope 112(1): 64-68.
- Fairbancs D (1985) Effect of nasal surgery on snoring Southern Medical Journal 48.
- Ellis P, M. Harries, JEF Willams, JE Shneerson (1992) The relief of snoring by nasal surgery. Clinical Otolaryngology 17: 525-527.
- Doyokov, V Stojanov (2013) Effecat of endo-nasal surgery on snoring. Trakia Journal of Sciences 4: 349-351.
- Low WK (1994) Can snoring relief after nasal septal surgery be predicted Clin. Otolaryngol Allied Sci.apr 19(2): 142-144.
- Elsherif J, Hussein S N (1998) The effect of nasal surgery on snoriing. AM J Rhinol 12(2):77-79.
- Yu Li (2008) Nasal surgery for snoring in patients with OSA. Laryngoscope 118: 354-359.





























