Bilateral Succesive Otogenic Cerebellar Abscesses- Case Report
Cristina Laza1* and Carp Ovidiu2
1ENT Clinic, Romania
2NKClinic, Romania
Submission: April 06, 2017; Published: April 17, 2017
*Corresponding author: Associate Professor, Cristina Otilia Laza-ENT/OMF Clinic, SCJU, SF Apostol Andrei "Bdul Tomis, 145, cod 8700, Constanta, Romania, Email: cristinaotilia@gmail.com
How to cite this article: Cristina L, Carp O. Bilateral Succesive Otogenic Cerebellar Abscesses-Case Report. Glob J Oto 2017; 6(5): 555697. DOI: 10.19080/GJO.2017.06.555697
Abstract
Chronic otitis with cholesteatoma, is a potentially dangerous disease and can lead to fatal complications, likeotogenic intracranial abscesses. Cerebellar abscess is two times less frequent than cerebral one, but 50% off all are otogenic in cause. Ussualy present in young male adults, but extremely rare can be a complications in chilldren with otitis. Although the frequency of these has dramatically decreased with advancements in antibiotic treatment, new neurosurgical techniques and diagnostic imaging technology such as CT, MRI, and the disease can still lead to death or complications like seizures, paresis and cognitive impairments. The purpose of this lecture is to presents a case with billateral cholesteatomatous otomastoiditis complicated succesive on both sides with cerebellar abscesses.This is an extremelly rare condition, only a few cases are described in literature
Keywords: Otogenic cerebellar abscess; Cholesteatoma; Osteitis; Mastoidectomy; Craniotomy; Otology; Neurosurgery
Case Presentation
The subject of this paper work it is a young patient with bilateral suppurated otitis from infancy, but neglected in a disorganized family, living on a farm house without current water or electricity.
The first contact with this patient was 11 years ago when at 13-years old was admitted in emergency in the clinic with a very bad general status and:
- ear related complains -bilateral foe tide otorrhea , hearing loss dizziness
- sings of intracranial hypertension =intense headache, nuchal rigidity, photophobia, vomiting
- neurological signs-dizziness, discoordination, vertigo strange behavior, confusion, superficial coma,
- infection related symptoms-high fever-39- 40oC , tahicardia, bad general status
Diagnosis was based on ENT, neurosurgical, infectious disease examinations, completed with
Imaging Studies
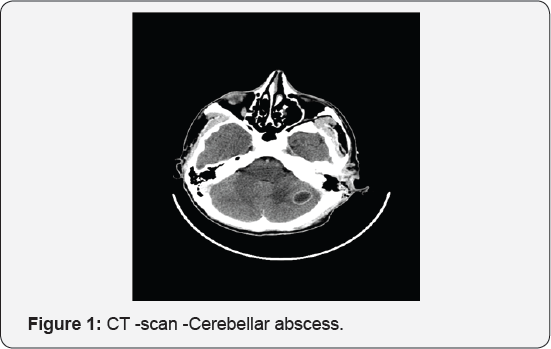
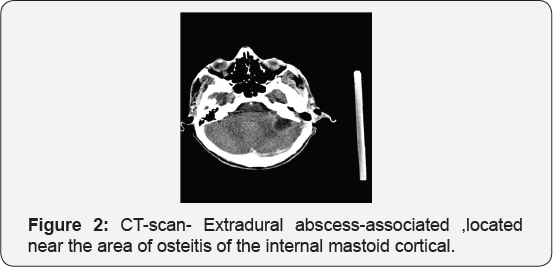
X-ray: mastoid Schuller, view show only erosion of the mastoid bone. CT scan, with i.v. contrast, confirm the diagnosis not only the destruction of the mastoid cells ,with osteitis of the walls, internal mastoid cortical, or of the tegmen tympany or antri ,erosion of the bony walls of the lateral sinus, horizontal semicircular channel, also presence of endocranial lesions in this case meningoencephalitis, extradural abscess and posterior cranial fossa -cerebelar abscess .Repeted at every 7 days permit evaluation in time of the process, abscess formation ,capsule formation and optimum moment for drainage (Figure 1 & 2). MRI offer a better exposure of soft tissues and inflammation saw is ideal for the brain showing difference between cerebritis and edema, also thrombosis of the venous sinuses [1-6].
Laboratory studies
- CBC count-anemia,leukemoid reaction, neutrophilia, trombocitosis ,Erythrocyte sedimentation rate -high,Serum C-reactive protein (CRP), high, HIV test-negative
- Blood cultures in fever,cultures from the ear (at least 2; preferably before antibiotic usage reveale Sthaphilococcus aureus
- Abscess aspirate (stereotactic CT or surgery) cultures for aerobes, anaerobes, Gram, acid-fast (for Mycobacterium), and special fungal stains (eg, methenamine silver, mucicarmineLab shows the same germ tests.
The therapy starts in ICU, with medical treatment consists in antibiotics with large spectrum and good penetrations in the brain and bone -Vancomicine plus Netromycine plus Metronidazole. Osmofundine , Dexamethasone ,sustaining of vital functions followed by-ENT surgery- radical mastoidectomy -performed on the third day when the patients was stabilized. The purpose is to remove the real cause of complications (Figures 3 & 4).
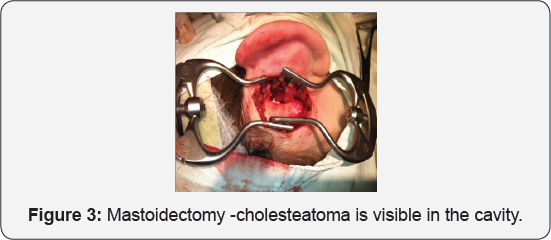
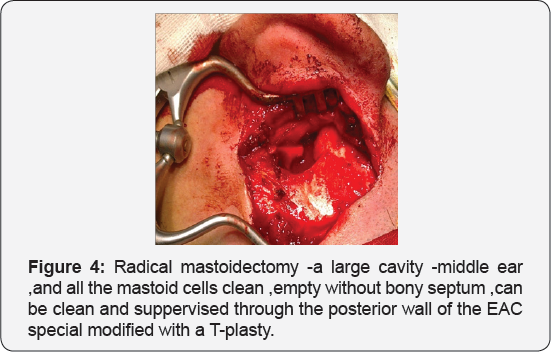
On surgery, performed using a retro auricular way, a large infected cholesteatoma was discovered, already the pseudotumour create a large cavity with erosion of the inner cortical, a portion of 1cm2 being absent [7]. At this moment of surgery pus came from the exposed extradural space, so we use suction, gentle irrigation with saline and peroxide till all the pus was remove. The neurosurgeon colleague complete the drainage of this collection. In the end we explore at the microscope the cells and the walls of the middle ear, antrum, removing all the lesions till good ,sane bone remained. The Fallope,s channel of facial nerve ,semicircular horizontal channel were intact. So finally a large total cavity remain in place after plastic opening of the EAC, capable to offer a good view of the middle ear and mastoid cavity.
After 2 weeks CT -scan revealed a large cerebellarabscess mature with clear capsule and was drained using a retro sigmoidcraniotomy. The child had an uneventful recovery. The pus from the mastoid process and cerebellar abscess revealed the same Staphilococcusaureus sensible to AB in use so we continue the same regimen for 6 weeks. He left the hospital in a good shape, with dry ears, a slight dizziness, walking on his feet [8]. He was called for follow up every month, to clean the cavity and for adenoidectomy but a never saw him. 10 years later I have the surprise to see him in emergency, now a 23 years young man, with the other side involved-with old otorrhea, but aggravated in the last 10 months, retroauricular right fistula, deafness, headache, dizziness, desechilibrum, sub fever. CT scan showed a small, < 2, 5 cm right cerebellar abscess, and cholesteatomatousotomastoiditis. The neurosurgical consultation recommends just medical treatment, the abscess being to small to require drainage so the patient was prepared for a mastoidectomy (Figure 5).

However, the patient left the hospital against medical advice, but after 10 days he return with severe headache, vomiting, abnormal behavior, nuchal rigidity, ataxia, vertigo. CT scan, showed a marked enlargement of the right-sided cerebellar abscess so, it was drained in emergency. After 10 days of intensive care treatment the patients was ready to support another surgical procedure mastoidectomy. Pus culture revealed Pseudomonasaeruginosa but the Meropenem+Vancomicine were continued for another 4 weeks period. The patient rapidly improved, with no signs of neurological sequels just deafness.
Discussion
Otogenic intracranial abscesses are usually caused by direct extension of infection beyond the temporal bone to the intracranial cavity, usually through [9]:
- Osteitisbony defect in the tegmenantri, tympani (in case of cerebral abscess usually temporal) or in Trautmann's triangle (cerebellar abscess).
- Retrograde thrombophlebitis of lateral sinus -propagating infected thrombus
- Anatomical pathway: oval, round window, internal auditory canal, cochlear & vestibular aqueduct
- Congenital bony defects: facial canal, tegmen plate
- Acquired bony defects: fracture, sharp objects, neoplasm, stapedectomy, implantable devices.
Microbial etiology depends on the patient's age, site ofprimary infection, and the patient's immune status: Staphylococcus aureus, Streptococcus pneumoniae, Enterobacteriaceae (Klebsiella pneumoniae, Escherichia coli, and Proteus species), Pseudomonas species, H influenzae, Neisseria meningitidis With increase nr of immune compromised patients ,HIV infected/AIDS transplants, chemoterapy, immuno-supresive medication ,increase the incidence of brain abscesses causes by opportunistic pathogens.
Laboratory studies
- CBC count, Erythrocyte sedimentation rate, Serum C-reactive protein (CRP)
- Blood cultures in fever, cultures from the ear (at least 2; preferably before antibiotic usage)
- Cerebrospinal fluid-lumbar punction is proscribe because of increased intracranial pressure with CNS herniation and death, only after previous CT imaging or MRI scanning, can be performed showing meningitis -abscess can burst in the subdural space [10]
- Abscess aspirate (stereotactic CT or surgery) cultures for aerobes, anaerobes, Gram, acid-fast (for Mycobacterium), and special fungal stains (eg, methenamine silver, mucicarmine)
Imaging Studies
- X-ray: mastoid Schuller, Chausee III, Stenvers views are now rare used showing only erosion of the bone, a possible abnormal position of the lateral sinus or of the tegmen (Figure 6).
- CT scanning: with contrast, is used to confirm the diagnosis, to localize the lesion, and to monitor the progression after treatment. Practic is the main investigation capable to explore not only the lesion in the ear, mastoid, extension, erosion of the lateral sinus, orizontal semicircular channel, facial nerv, internal or external cortical of the mastoid bone, also the lesion like edema, collection, trombosys are encephalitis, hydrocephalus are visible.
- MRI: confere a better ability to detect cerebritis, greater contrast betweenedema and the brain, and earlier detection of satellite lesions and the spread .
Treatment
Most abscesses are managed with a combined medical & surgical program
The management involves cooperation among neurologists, neurosurgeons, and infectious diseases specialists. Other specialists may be consulted as required by the patient's condition.
Medical Treatment
The antibiotic regimen used on ivadm. First empirical then is revised as data become available from cultured abscess material. Length of therapy is determined by patient course and follow-up MRI or CT. In general, antibiotics should be continued for at least 4-6 weeks. Vancomycin--effective against MRSA and S. epidermidis, aerobic/anaerobic streptococci, and Clostridium Linezolid-the same. Metronidazole -penetrates well into the CNS, active against anaerobic bacteria. Third- generation cephalosporins ( cefotaxime, ceftriaxone) provide adequate therapy for aerobic g-+ram-negative organisms, aerobic streptococci. If Pseudomonas are isolated the choice is a forth generation cephalosporin (ceftazidime or cefepime). Fluoroquinolones -penetration into the CNS, limited use in treating brain abscesses. Meropenem used in large doses seams to increase chance of survival. Injection of Ab into the abscess cavity after drainage is not needed -many Ab penetrate brain fairly well [11,12].
Adjuvant Therapy
Several additional therapeutic issues must be used in the patient with brain abscess. Cerebral edema may require emergent treatment with hyperventilation, mannitol, or Dexamethasone. Mannitolas a 20% solution, 0.25 to 0.5 g/kg every 3 to 5 hours, with control of serum electrolytes and osmolarity. Dexamethasone is effective in reducing vasogenic edema, 8 mg intravenously initially followed by 4 mg intravenously every 4 to 6 hours when intracranial pressure is of major concern
- Administration of glucoses, serum, electrolytes, it's important for the supports.
- Subcutaneous heparin should be considered in patients remaining at bed rest for extended periods of time.
- Seizures may be treated with intravenous diazepam, 10 mg, or lorazepam, 4 mg, or 10 to 15 mg/kg phenytoin in normal saline. Midazolam, propofol, phenobarbital, or other agents may be required to control seizures unresponsive to phenytoin. Seizures may occur weeks to months after recovery so initiation of therapy with phenytoin or other agents, for 2 years is required after neurosurgical drainage
- Symptomatics-AINS, stabilisation in ICU, corection of anaemia, trombopenia
- Local drops with antibiotics, aspiration of the pus from the ear
Surgical Care
A delay in surgical drainage and decompression can be associated with high morbidity and mortality
Neurosurgical procedures: is possible in large, mature abscesses, imposible to responde to medical therapy alone or if neurologic, motor or sensory cortex area are involved or the patient is comatose. Needle aspiration -stereotactic procedure via CT guided with fewer sequelae, also for inaccesible deep areas, speech, motor areas, comatouspatients, multiples abscesses. Excision of the capsule using a retrosygmoidcraniectomy, transmastoid = indicated in superficiall multiloculated abscesses, if reaccumulate following repeated aspirations, there are no clinical improvements within 7 days, or in a progressively growing abscess.
Otological procedures: must clear the source of infection. Radical mastoidectomy/canal wall-down after patient became stable. The surgical procedure is then fallowed by every day cleaning the wound, aspiration of the cavity after paking was removed in the 3-th day, gentle washig trough the draining tubes with saline ,peroxide or betadine .In the cavity we can insert small gauses with local antibiotics like Ciplox, Tobradex, Vygamox etc or we can pulverised boric acid or riphampycine
Complications
Permanent neurological damage include hydrocephalus, intellectual and behavioral disorders, ataxia, spasticity, vertigo, discoordination. Recurrent seizures develop in about 10-30% of survivors.
Results
- Every time the recovery was complete and quick, without complications, or neurological sequels, so we consider that the results were excellent.
- CT scan repeated at 1,6 and 12 month with contrast enhacement were negative
- Bilateral deafness remained at the same level medium-transmission type, but reconstruction of eardrum, ossicles, is proscribed-high risc of reccurence of cholesteatoma
- The rehabilitation of the hearing is a futures project for this patient, a BAHA implant is considered the best choice.
- Another problem to solve -nasal chronic obstruction caused by a nasal septum deviation is a new step in the follow-up programm.
- Predisposing factors like immune-deficient, HIV inf, congenital defects in the petro us bones were excluded with lab tests, like HIV, immunogram or CT scans.
- Our patient belong to the lower socio-economic class, maybe nutritional status, bad hygiene are implicated,but for sure later presentation to the doctor.
- viii. The patient now a young adult was well informed how to prevent water to enter in the ears, respect the follow-up program, including periodic cleaning of the mastoid cavities
Conclusion
The development of a simillar complication on the other side is extremely rare in the history of endocranial complications in cholesteatomatousotomastoiditis. Just a few reports exist in literature till now. Much rare than the temporal abscess, cerebellum abscess is known to be particularly serious difficult to diagnose and to drain. Also, it presents higher mortality and can be multicentric.
CT scan and MRI are essential for diagnosis- osteitis, cholesteatoma in the temporal bone, erosion of the internal mastoid cortical, endocranial disorders -edema, masses, collections, evolutions of the lesions. The coordination between ENT and NK surgeon is essential, the exact time for a mastoidectomy and drainage of the cerebellar abscess depends on the lesions, evolution, and general status of the patient. Early management of the primary ear disease, drainage of the abscess, appropriate course of antibiotics is the therapeutic approach of choice.Surviance must be from both departments at least 1 year.
References
- Bailey, Love's. Short Practice of Surgery (20th edn)
- JL Cummings. Clinical Neuropsychiatry.
- Davidson's Principal and Practice of Medicine (16th edn).
- Erdogan E, Cansever T (2008) Pyogenic brain abscess. Neurosurg Focus 24(6): 1-10.
- JH Adams, LW Duchen. Greenfield's Neuropathology.
- Harrison's. Principles of Internal Medicine (12th edn).
- Logan Turner's. Diseases of the Nose, Throat and Ear (10th edn).
- Lu CH, Chang WN, Lui CC (2006) Strategies for the management of bacterial abscess. J Clin Neurosci 13(10): 979-985.
- Mathisen GE, Johnson JP (1997) Brain abscess. Clin Infect Dis 25(4): 763-781.
- Burrows and Leeds. Neuro -Radiology (9th edn).
- Raymond D Adams, Maurice Victor. Principles of Neurology.
- Solomon T (2009) Donaghy M Brain's Diseases of the Nervous System (12th edn) Oxford University Press, USA.





























