Treatments for Attention Deficit Hyperactivity Disorder
Ghazal Farjami*1 and Yalda Mahmoody2
1University of New England, Australia
2Monash University, Australia
Submission:October 26, 2023; Published:November 16, 2023
*Corresponding author:Ghazal University of New England, Australia, Email: gfarjami@myune.edu.au
How to cite this article: Ghazal F. Treatments for Attention Deficit Hyperactivity Disorder. Glob J Intellect Dev Disabil. 2023; 12(5): 555850. DOI:10.19080/GJIDD.2023.12.555850
Abstract
Attention Deficit Hyperactivity Disorder (ADHD) is a prevalent neurodevelopmental condition that typically emerges during childhood. It is characterized by difficulties in focus, distractibility, hyperactivity, and impulsiveness. These symptoms pose significant risks for individuals, their families, and the broader communities in which they reside. These complications include, but are not limited to, academic struggles, difficulties in developing and maintaining social and emotional relationships, mental comorbidities, and financial burdens. It is estimated that ADHD affects roughly 5-7% of school-age children, with boys receiving diagnoses twice as often as girls. Notably, a substantial majority of these children continue to exhibit symptoms into adulthood.
Keywords: Attention Deficit Hyperactivity Disorder; Neurodevelopmental conditions; Mental Disorders; Social skills
Introduction
Attention Deficit Hyperactivity Disorder (ADHD) is a prevalent neurodevelopmental condition that typically emerges during childhood. It is characterized by difficulties in focus, distractibility, hyperactivity, and impulsiveness [1,2]. These symptoms pose significant risks for individuals, their families, and the broader communities in which they reside. These complications include, but are not limited to, academic struggles, difficulties in developing and maintaining social and emotional relationships, mental comorbidities, and financial burdens [2-4]. It is estimated that ADHD affects roughly 5-7% of school-age children, with boys receiving diagnoses twice as often as girls [3,4]. Notably, a substantial majority of these children continue to exhibit symptoms into adulthood [3,4].
The precise aetiology of ADHD remains incompletely understood; however, there is considerable evidence suggesting a significant genetic contribution [5]. In addition, various environmental factors, such as maternal smoking or drinking during pregnancy, premature birth, low birth weight, exposure to chemicals, family environment characteristics, and early childhood trauma experiences, have been identified as potential contributors to ADHD [5].
As outlined in the Diagnostic and Statistical Manual of Mental Disorders [6], ADHD presents itself through three principal manifestations: i) predominantly inattentive: encompassing distractibility and challenges in task completion. ii) predominantly hyperactive and impulsive; including excessive motor activity, persistent verbalization, impulsive actions, and challenges in regulating impulsive urges iii) combined ADHD characterized by a combination of inattentiveness and hyperactive-impulsive traits. To diagnose the presence of any of these presentations, it is important to observe these behaviours across several contexts for example school and home, for a significant duration, and determine whether they result in hindrance to the child's educational achievements or social skills [6].
Method
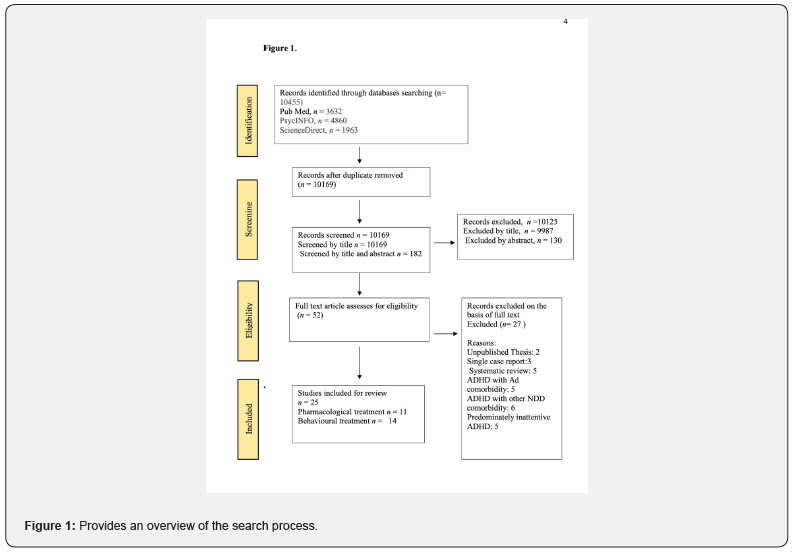
The objective of this review is to provide a summary of the scientific literature pertaining to the evidence-based pharmacological and non-pharmacological interventions for ADHD. Adhering to Prisma guideline [7], a comprehensive search conducted manually across 3 major electronic databases of PubMed, PsycINFO, and ScienceDirect with the key terms “ADHD”, and “treatment”. A total of 10455 studies were identified during the initial search procedure (PubMed, n =3632; PsycINFO, n= 4860; ScienceDirect, 1963).
Further, 286 studies were removed due to duplication and subsequently the title and abstract of the studies were screened and categorised as either included or excluded research. From 10169 studies, 9987 studies excluded by title, further 138 publications excluded by screening the abstract and the remaining 44 studies were included for full text assessment. The inclusion criteria were: i) written in English language ii) conducted as a randomised controlled trial (RCT) iii) conducted between January 2004 and September 2023. The exclusion criteria were i) single-case reports ii) unpublished manuscript thesis iii) systematic reviews iv) no comorbidity with ASD or other NDD. The final examination included 25 studies for the review (Figure 1).
Result
Pharmacological approaches
The management of ADHD in people might be pharmacological base, nonpharmacological based or a mix of both approaches. The pharmacological management of ADHD is broadly classified into two main categories: stimulant and non-stimulant medications.
Stimulant medicines: Stimulant medicines are widely regarded as the first line therapy option,
demonstrating a response rate of roughly 70% [8]. Methylphenidate (MPH) and certain amphetamine are considered the primary stimulant drugs [9]. These substances act by the inhibition of dopamine and norepinephrine transporters, augmenting the effects of dopamine and norepinephrine leading to improved functioning of the prefrontal cortex [10]. This enhancement ultimately optimises executive and attentional capabilities in individuals diagnosed with ADHD [8].
A double blind randomised controlled trial conducted by Findling et al. [9] attempted to evaluate the efficacy of methylphenidate medication in ADHD children. Utilizing the Clinician-rated ADHD Rating Scale (ADHD-RS-IV), the researchers compared the effect of MRH with the placebo over the period of seven weeks and demonstrated a significant improvement in the total score of ADHD-RS-IV for the participants in MPH.
Similarly, Childress et al. [11] carried out a study on 199 children aged 4 to 5 years old randomly assigned to lisdexamfetamine dimesylate (LDX), which is a type of amphetamine, or placebo daily over a period of 6 weeks. The findings from this study showed reduced symptoms of ADHD in individuals received LDX compared to placebo.
Regarding tolerability, the above-mentioned studies consistently demonstrated that these medications were generally well-tolerated, with participants reporting modest side effects like decreased appetite, nausea, and insomnia.
Non- stimulant medicines: The second line of pharmacological intervention for ADHD is non
stimulant medications, which include atomoxetine, guanfacine, alpha agonist and non-tricyclic antidepressant [12]. Unlike stimulant medications, non-stimulant medications have a significantly slower onset of action and require more time to produce noticeable effects, with a lower rate of effectiveness when compared to stimulant medications [10].
Atomoxetine is a norepinephrine reuptake inhibitor that acts by increasing the level of norepinephrine in the synapses and consequently improving attention and reduces impulsivity [12]. An RCT carried out by Ni et al. [13] compared the effects of stimulant methylphenidate with nonstimulant atomoxetine on the executive function of the adults with ADHD revealed different aspects of the executive functions including working memory, planning/ prioritizing skills, emotional regulation, and flexibility, improved by both these treatments.
Additionally, non-tricyclic antidepressants such as bupropion and viloxazine are used for the management of the ADHD symptoms. These medications seem to work through blocking the reuptake of serotonin, dopamine, and norepinephrine neurotransmitters thereby increasing their levels in the brain [10,12]. In 2021, Naser et al. [14], conducted a study aiming to evaluate the effects of daily doses of either 200 mg or 400 mg of viloxazine as a monotherapy for ADHD in a sample of 313 adolescents aged 12-17 years. Interestingly, when compared to the placebo group, participants in both treatment groups demonstrated significant improvements, and there were no significant differences in the outcomes between the two treatment groups.
Alpha-2 noradrenergic agonists such as guanfacine and clonidine have also been used as non-stimulant medications for managing ADHD. These substances act by stimulating the presynaptic alpha-2A receptors and regulating the concentration of the norepinephrine in the brain [10]. In a two phased, double-blinded RCT conducted by Jain et al. [15], a sample of 236 participants, aged 6 to 17 years old with clinical diagnosis of ADHD was randomly allocated into three separate arms of CLON-XR 0.2 mg/day (n = 78), CLONXR 0.4 mg/day (n = 80), and placebo (n = 78) for the duration of 8 weeks. The findings from this study revealed a significant improvement in the ADHD-RS-IV total score within the treatment groups compared to the placebo group. However, no explicit comparison was recorded between the two therapy groups.
Non pharmacological approaches
While medications are considered as the primary therapeutic approaches for ADHD, they are only effective for 70 - 80% of individuals, leaving a significant proportion of patients unresponsive or experiencing adverse side effects [10]. Therefore, nonpharmacological treatments such as cognitive behaviour therapy (CBT), dietary changes, physical activity, supplements, meditation, and hypnotherapy were reported to be effective as either alternative or complimentary interventions.
In 2012, Sprich et al. [16], conducted interviews with a sample of 11 adults who were already undergoing prescription treatment for ADHD to explore their challenges in managing their ADHD symptoms. The collected responses revealed significant difficulties, particularly in the areas of organization/planning and anger control in day-to-day lives of these individuals. These findings highlighted the need to equip these individuals with strategies to overcome those challenges. Subsequently, the same research team developed a CBT approach consisting of three core modules: i) organizing and planning, ii) coping with distractibility, and iii) adopting effective thinking. Additionally, there were two elective modules: i) procrastination management and ii) involving a partner or spouse in the process. To assess the practicality and effectiveness of these modules, 31 adults diagnosed with ADHD were recruited and randomly assigned to either receive 'CBT plus pharmacotherapy' or continue with 'pharmacotherapy only.' The performance of the participants was assessed first at baseline and subsequently on week 4, 8 and 12 and showed greater improvement in the group that incorporated CBT into their treatment. In another study, Sprich et al. [17] investigated the effectiveness of CBT on 46 adolescents who did not respond to medication and suggested that CBT can be an alternative replacement for those who do not respond to pharmacological intervention.
Exercise
Research has repeatedly shown that physical activity stimulates the production of dopamine, reduces stress, enhances memory, and improves the quality of sleep all of which can assist with the symptoms of ADHD. In a 10-week CRT, Bustamante, et al. [18], investigated the effectiveness of regular after school exercise on the ADHD related behaviours. The participants in the treatment group showed improvements in attention and emotion control. A similar study conducted by Ramer et al. in 2020 showed improvement in the effects of a 10-week after-school physical activity on the academic performance and classroom behaviour of children aged 6 to 12 who were diagnosed with ADHD and/or disruptive behaviour problems.
Diet
Research on the impact of nutrition on ADHD symptoms has yielded diverse results. Some studies propose that avoiding specific foods like allergens, artificial food dyes, sugar, additives, and preservatives can help alleviate ADHD symptoms, while others contest this hypothesis. In a two-arm RCT conducted by Bosch et al. [19], 162 children were randomly assigned to three groups: an elimination diet, a healthy diet, and a control group (no change in dietary routine). This study demonstrated significant improvements in symptoms, academic and social performance, sleep patterns, and dietary habits in both diet groups. However, studies by Verlaet et al. [20] and Cagigal et al. [21], argue against this idea, suggesting that the differences are minimal, and the risk of bias is high.
Supplements
Supplements such as vitamin D, B6, magnesium, omega-3 fatty acids, iron and zinc have been suggested to improve cognitive and behavioural outcomes, including attention, hyperactivity, impulsivity, and oppositional behaviour [22-24]. These positive effects may be attributed to the crucial roles these substances play in synaptic plasticity and the regulation of neurotransmitter levels, thereby influencing brain function [23]. In a multivariate analysis conducted by Bener et al. [22], statistically significant differences were found in the levels of various biomarkers, including vitamin B, vitamin D, and magnesium between the ADHD group and the control group. Also, two studies by Mohammadpour et al. and Dehbokri et al. [25,26], reported a reduction in ADHD symptoms after a period of vitamin D therapy. Similarly, in a 12-week double-blind study conducted by Pellow et al. [24], a daily supplement of 150 mg of zinc sulfate, resulted in significant reductions in hyperactivity, impulsivity, and impaired socialization among the participants.
GABA
Maintaining sufficient and balanced levels of the excitatory neurotransmitter glutamate and the inhibitory neurotransmitter GABA is crucial for sustaining a healthy, functioning brain. A substantial body of empirical research has demonstrated that a decrease in GABA concentration and an increase in glutamate levels are associated with disfunctions in the activity of brain and the development of neurodevelopmental disorders, including ADHD [27,28]. Gilbert et al. [28], utilized transcranial magnetic stimulation (TMS) to study the balance of excitatory and inhibitory processes within the human cortex by measuring short-interval intercortical inhibition (SICI) in a group of school-age children who had been diagnosed with ADHD. The findings of this research suggested a direct link between the reduction of SICI, which indicates an imbalance of GABA and glutamate, and the severity of ADHD symptoms.
Neurofeedback (NF)
Neurofeedback (NF) is a cognitive training method that teaches individuals how to regulate their own brain processes by assessing brainwave activity and providing positive or negative feedback. The effectiveness of neurofeedback as a monotherapy or an adjunctive treatment for ADHD has been studied by several researchers. Namely, in a RCT conducted by Geladé et al. [29], three interventions (stimulant medication, exercise, and NF) were compared, and medication showed greater therapeutic results than the other two treatments. Meanwhile, Lee and Jung [30], assessed the efficacy of NF as an addition to medication treatment, revealing improved attention and cognitive function in subjects who received both NF and medication compared to those who only received medication.
Hypnotherapy and meditation
The potential benefits of hypnotherapy and meditation for individuals with ADHD can be attributed to a range of neurobiological and psychological factors. Hypnotherapy has the potential to facilitate stress reduction, improve self-regulation capabilities, enhance focus and concentration, and effectively target behavioural challenges such as procrastination [31]. Additionally, meditation has been found to enhance self-regulation, neuroplasticity, attentional capacity, stress management, and sleep quality [32].
These techniques are frequently employed in conjunction with additional therapeutic modalities such as CBT and pharmacological interventions. Aladdin (2008; 2009) has elucidated a methodology pertaining to cognitive hypnotherapy. Jensen and Kenny [33], examined the potential benefits of yoga as a complementary treatment for boys with ADHD who were already on medication. Results showed significant improvements in areas assessed by the Conners' Parent Rating Scales (CPRS) compared to the control group.
Behavioural parent training (BPT)
Behavioral parent training (BPT) is considered one of the psychosocial treatments for ADHD supported by empirical evidence. During these training sessions, parents learn about the disorder and effective strategies for managing ADHD-related behaviors. Two studies by Van Den et al. [34], and Xie et al. [35], demonstrated the positive impact of training parents on children's success in school, including academic achievement, social interactions, and impulsivity. The importance of parent training programs was emphasized by Fabiano et al. [36].
Discussion
ADHD is a common neurobehavioral disorder that typically manifests in childhood and may persist into adulthood, potentially affecting various aspects of an individual's life if not appropriately addressed. The present paper is based on findings from several evidence based studies on interventions that have shown effectiveness in mitigating ADHD symptoms. These interventions encompass various pharmacological and behavioural approaches. Pharmacological-based treatments include stimulant and non-stimulant medications. Stimulant medications such as methylphenidate and certain amphetamines are reported as the first line and most effective therapeutic approach for addressing ADHD. These medications function by inhibiting the reuptake process of certain neurotransmitters responsible for the core symptoms associated with ADHD. Furthermore, non-stimulant drugs, including atomoxetine, guanfacine, alpha agonists, and non-tricyclic antidepressants, have exhibited effectiveness in mitigating symptoms of ADHD, albeit with a longer time frame for their effects to become apparent compared to stimulant medications. Significantly, non-stimulant drugs often exhibit a reduced likelihood of adverse side effects and a decreased potential for dependency or drug addiction compared to stimulant medications [37-39].
Conclusion
Since the response to pharmacological treatment varies among individuals, nonpharmacological interventions such as CBT, dietary adjustments, physical activity, vitamin supplements, hypnotherapy, and meditation have been identified as potentially efficacious alternative or adjunctive interventions capable of augmenting the outcomes of pharmacological treatments. These therapies have the potential to result in enhancements in attention, hyperactivity, impulsivity, and oppositional behaviour, ultimately enhancing the quality of life of the affected individuals.
References
- Dalsgaard S (2013) Attention-deficit/hyperactivity disorder (ADHD) European Child & Adolescent Psychiatry 22: 43-48
- Tarver J, Daley D, Sayal K (2014) Attention-Deficit Hyperactivity Disorder (ADHD): an updated review of the essential facts. Child Care Health Dev 40(6): 762-774.
- Kazda L, McGeechan K, Bell K, Thomas R, Barratt A (2022) Association of Attention-Deficit/Hyperactivity Disorder Diagnosis with adolescent quality of life. JAMA Network 5(10):
- Wilens TE, Spencer TJ (2010) Understanding Attention-Deficit/Hyperactivity Disorder from childhood to adulthood. Postgraduate Medicine 122(5): 97-109.
- Sciberras E, Mulraney M, Silva D, Coghill D (2017) Prenatal risk factors and the aetiology of ADHD-review of existing evidence. Current Psychiatry Reports 19(1): 1.
- American Psychiatric Association D, American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders: DSM-5 (Vol. 5, No. 5) Washington, DC: American psychiatric association.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, et al. (2021) The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ (Clinical research ed.): 372: n71.
- Tebartz van Elst L, Maier S, Klöppel S, Graf E, Killius C, et al. (2016) The effect of methylphenidate intake on brain structure in adults with ADHD in a placebo-controlled randomized trial. J Psychiatry Neurosci 41(6): 422-430.
- Findling RL, Bukstein OG, Melmed RD, López FA, Sallee FR, et al. (2008) A randomized, double-blind, placebo-controlled, parallel-group study of methylphenidate transdermal system in paediatric patients with Attentiondeficit/Hyperactivity Disorder. J Clin Psychiatry 69(1): 149-159.
- Drechsler R, Brem S, Brandeis D, Grünblatt E, Berger G, et al. (2020) ADHD: Current Concepts and Treatments in Children and Adolescents. Neuropediatrics 51(5): 315-335.
- Childress AC, Lloyd E, Jacobsen L, Gunawardhana L, Johnson SA, et al. (2022) Efficacy and safety of Lisdexamfetamine in preschool children with Attention-Deficit/Hyperactivity Disorder. J Am Acad Child Adolesc Psychiatry 61(12): 1423-1434.
- Budur K, Mathews M, Adetunji B, Mathews M, Mahmud J (2005) Non-stimulant treatment for attention deficit hyperactivity disorder. Psychiatry 2(7): 44-48.
- Ni HC, Shang CY, Gau SS, Lin YJ, Huang HC, et al. (2013) A headto- head randomized clinical trial of methylphenidate and atomoxetine treatment for executive function in adults with attention-deficit hyperactivity disorder. Int J Neuropsychopharmacol 16(9): 1959-1973.
- Nasser A, Liranso T, Adewole T, Fry N, Hull JT, et al. (2021) A Phase 3, Placebocontrolled trial of once-daily Viloxazine extended-release capsules in adolescents with Attention-Deficit/Hyperactivity Disorder. J Clin Psychopharmacol 41(4): 370-380.
- Jain R, Segal S, Kollins SH, Khayrallah M (2011) Clonidine extended-release tablets for paediatric patients with Attention-Deficit/Hyperactivity Disorder. J Am Acad Child Adolesc Psychiatry 50(2): 171-179.
- Sprich SE, Knouse LE, Cooper-Vince C, Burbridge J, Safren SA (2012) Description and demonstration of CBT for ADHD in adults. cognitive and behavioral practice 17(1): 10.
- Sprich SE, Safren SA, Finkelstein D, Remmert JE, Hammerness P (2016) A randomized controlled trial of cognitive behavioural therapy for ADHD in medication‐treated adolescents. Journal of Child Psychology and Psychiatry 57(11): 1218-1226.
- Bustamante EE, Davis CL, Frazier SL, Rusch D, Fogg LF, et al. (2016) Randomized controlled trial of exercise for ADHD and disruptive behaviour disorders. Medicine and Science in Sports and Exercise 48(7): 1397-1407.
- Bosch A, Bierens M, de Wit AG, Ly V, van der Velde J, et al. (2020) A two-arm randomized controlled trial comparing the short- and long-term effects of an elimination diet and a healthy diet in children with ADHD (TRACE study) BMC Psychiatry 20(1): 262.
- Verlaet AA, Noriega DB, Hermans N, Savelkoul HF (2014) Nutrition, immunological mechanisms, and dietary immunomodulation in ADHD. European Child & Adolescent Psychiatry 23(7): 519-529.
- Cagigal C, Silva T, Jesus M, Silva C (2019) Does diet affect the symptoms of ADHD? Current Pharmaceutical Biotechnology 20(2): 130-136.
- Bener A, Kamal M, Bener H, Bhugra D (2014) Higher prevalence of iron deficiency as strong predictor of attention deficit hyperactivity disorder in children. Annals of Medical and Health Sciences Research, 4(Suppl 3): S291-S297.
- Königs A, Kiliaan AJ (2016) Critical appraisal of omega-3 fatty acids in Attention- Deficit/Hyperactivity disorder treatment. Neuropsychiatric Disease and Treatment 12: 1869-1882.
- Pellow J, Solomon EM, Barnard CN (2011) Complementary and alternative medical therapies for children with attention-deficit/hyperactivity disorder (ADHD) Alternative Medicine Review 16(4): 323-337.
- Mohammadpour N, Jazayeri S, Tehrani-Doost M, Djalali M, Hosseini M, et al. (2018) Effect of vitamin D supplementation as adjunctive therapy to methylphenidate on ADHD symptoms: A randomized, double blind, placebo-controlled trial. Nutritional Neuroscience 21(3): 202-209.
- Dehbokri N, Noorazar G, Ghaffari A, Mehdizadeh G, Sarbakhsh P, et al. (2019) Effect of vitamin D treatment in children with attention-deficit hyperactivity disorder. World Journal of Paediatrics: WJP 15(1): 78-84.
- Naaijen J, Bralten J, Poelmans G, IMAGE consortium, Glennon JC, et al. (2017) Glutamatergic and GABAergic gene sets in AttentionDeficit/Hyperactivity Disorder: Association to overlapping traits in ADHD and Autism. Translational Psychiatry 7(1): e999.
- Gilbert DL, Isaacs KM, Augusta M, Macneil LK, Mostofsky SH (2011) Motor cortex inhibition: A marker of ADHD behaviour and motor development in children. Neurology 76(7): 615-621.
- Geladé K, Janssen TW, Bink M, van Mourik R, Maras A, et al. (2016) Behavioral effects of neurofeedback compared to stimulants and physical activity in Attention-Deficit/Hyperactivity Disorder: A randomized controlled trial. The Journal of Clinical Psychiatry, 77(10): e1270-e1277.
- Lee EJ, Jung CH (2017) Additive effects of neurofeedback on the treatment of ADHD: A randomized controlled study. Asian Journal of Psychiatry 25: 16-21.
- Alladin A (2012) Cognitive hypnotherapy: A new vision and strategy for research and practice. The American Journal of Clinical Hypnosis, 54(4): 249-262.
- Krisanaprakornkit T, Ngamjarus C, Witoonchart C, Piyavhatkul N (2010) Meditation therapies for Attention-Deficit/Hyperactivity Disorder (ADHD) The Cochrane Database of Systematic Reviews 2010(6): CD006507.
- Jensen PS, Kenny DT (2004) The effects of yoga on the attention and behaviour of boys with Attention-Deficit/ hyperactivity Disorder (ADHD) Journal of Attention Disorders 7(4): 205-216.
- Van den Hoofdakker BJ, van der Veen-Mulders L, Sytema S, Emmelkamp PMG, Minderaa RB, et al. 2007) Effectiveness of behavioural parent training for children with ADHD in routine clinical practice: A randomized controlled study. Journal of the American Academy of Child and Adolescent Psychiatry, 46(10): 1263-1271.
- Xie Y, Dixon JF, Yee OM, Zhang J, Chen YA, et al. (2013) A study on the effectiveness of videoconferencing on teaching parent training skills to parents of children with ADHD. Telemedicine Journal and E-Health: The Official Journal of the American Telemedicine Association, 19(3): 192-199.
- Fabiano GA (2007) Father participation in behavioural parent training for ADHD: Review and recommendations for increasing inclusion and engagement. Journal of Family Psychology 21(4): 683-693.
- Hemamy M, Heidari-Beni M, Askari G, Karahmadi M, Maracy M (2020) Effect of vitamin D and magnesium supplementation on behaviour problems in children with Attention-Deficit Hyperactivity Disorder. International Journal of Preventive medicine 11: 4.
- Ramer JD, Santiago-Rodríguez ME, Davis CL, Marquez DX, Frazier SL, et al. (2020) Exercise and academic performance among children with attention-deficit hyperactivity disorder and disruptive behaviour disorders: A randomized controlled trial. Paediatric Exercise Science 32(3): 140-149.
- Van der Heijden KB, Smits MG, Van Someren EJ, Ridderinkhof KR, Gunning WB (2007) Effect of melatonin on sleep, behavior, and cognition in ADHD and chronic sleep-onset insomnia. J Am Acad Child Adolesc Psychiatry 46(2): 233-241.






























