Predictors of Chronic Debilitating Conditions Among Refugees Resettled in the United States
Edson Chipalo*
Department of Social Work, College of Education and Social Sciences, Lewis University, One University Parkway, USA
Submission:September 15, 2023;Published:October 05, 2023
*Corresponding author:Edson Chipalo, Department of Social Work, College of Education and Social Sciences,Lewis University, One University Parkway, Romeoville, IL 60446, USA,
How to cite this article: Chipalo E. Predictors of Chronic Debilitating Conditions Among Refugees Resettled in the United States. Glob J Intellect Dev Disabil. 2023; 12(4): 555844.DOI:10.19080/GJIDD.2023.12.555844
Abstract
Background: Refugees resettled in the United States face numerous challenges, including poor health conditions. However, knowledge of factors influencing chronic debilitating conditions among refugees is scarce. Therefore, this study examined the prevalence and potential factors associated with chronic debilitating conditions within the U.S. refugee population.
Methods: This study utilized secondary data from the 2018 Annual Survey of Refugees (ASR) involving 1007 refugees resettled in the U.S. The prevalence estimates were obtained using chi-square tests, and multiple logistic regression was used to determine the significant association between predictor variables and chronic debilitating conditions among the refugees in the United States.
Results: 25.5% of the refugees reported having chronic debilitating conditions. Regression results showed that being an older refugee and having adjusted immigration status to become a permanent resident was associated with higher odds of reporting chronic debilitating conditions. However, refugees who were currently working, married, and with good English language proficiency were associated with a lower likelihood of reporting chronic debilitating conditions. Gender and education levels of refugees were not significantly associated with chronic debilitating conditions after covariates adjustments.
Conclusion: This study provides a comprehensive understanding of the prevalence and potential predictors of chronic debilitating conditions among refugees in the United States. Tailored interventions focusing on increasing access to education and employment opportunities to enhance health literacy and financial resources are crucial to mitigate chronic debilitating conditions. In addition, addressing the language barriers through language and interpretation services in clinical settings can also improve healthcare access, thus reducing the risk of chronic debilitating conditions among refugees resettled in the United States.
Keywords: Chronic debilitating conditions; Refugees; Immigration; English proficiency; Age; Gender; Education; Married; Employment; United States
Introduction
Refugees are widely acknowledged as one of the most vulnerable segments of our society, having left their home countries due to conflict and endured many hardships, including imprisonment, torture, persecution, property loss, malnutrition, physical assault, psychological trauma, profound fear, deprivation, sexual assault, loss of livelihood, and exposure to adverse environmental conditions [1]. The vulnerable refugees may exhibit distinct healthcare needs stemming from the adverse consequences of conflict and forced displacement leading to severe trauma and present substantial physical and mental health challenges [2-4]. The refugee resettlement journey frequently entails psychological and physical upheaval. Chronic debilitating conditions denote long-term physical or mental health issues that progressively weaken bodily mental or cognitive functions [5-7]. Given the traumatic experiences refugees have endured during the conflict, it is anticipated that a large portion of refugees may face the risk of developing chronic debilitating conditions as they age, which may include functional disabilities [8]. Chronic debilitating conditions can hinder refugees’ ability to engage in the workforce, rendering it progressively difficult for them to maintain employment, thereby leading to economic challenges for both the refugees themselves and the host nation [9-12].
A large majority of refugees encounter language barriers, leading to miscommunication and hindering their access to healthcare. Refugees originate from different countries with vastly different healthcare systems, and their limited familiarity with available services, compounded by language barriers, further contributing to poor health outcomes [13,14]. Refugees might face limited educational opportunities and encounter various obstacles when navigating the healthcare system and understanding the available healthcare resources. Consequently, this heightened the risk of experiencing poor health conditions among the refugees within the host country [15]. Refugees may also be at risk of certain diseases or health conditions due to their circumstances. These individuals often originate from economically disadvantaged and environmentally contaminated regions and have experienced natural disasters, factors that may contribute to their compromised health status [16]. Despite the contentious nature of addressing refugee healthcare within host countries, doing so can yield several benefits. These include improved health outcomes, the promotion of integration, the mitigation of long-term health issues and associated social costs, contributions to social and economic development, and the protection of public health and human rights [16]. It is also crucial to understand that immigration status does not directly determine poor health conditions. However, migrants can be vulnerable to various physical, mental, and social health challenges from the migration process and their unique circumstances [7].
Previous research has provided evidence of the poor health conditions experienced by refugees with traumatic backgrounds in host countries. To our knowledge, there has been no comprehensive examination of the relationship between various factors and these conditions among resettled refugees in the United States using credible national data. Therefore, the primary objectives of this study are twofold: (1) to determine the prevalence of chronic debilitating conditions and (2) to assess whether there is an association between sociodemographic factors and chronic debilitating conditions among refugees resettled in the United States. A deeper understanding of these contributing factors is essential for informing public health initiatives, improving practices, and refining policies for refugees in the United States. Throughout this study, “chronic debilitating conditions” will consistently refer to general physical, mental, or other health conditions affecting refugees in the United States, as previously conceptualized in the previous study [17].
Methods
Data Source and Sampling Design
This study utilized secondary data from the 2018 Annual Survey of Refugees (ASR). The 2018 ASR was a cross-sectional design, employing a stratified probability sampling method to select refugees. A total of 6,100 refugee households that were resettled between 2013 and 2017 were contacted for participation in the survey. During this period, the United States welcomed 348,508 refugees from 100 countries, speaking 246 different languages. The aim of ASR was to ensure that the selected refugees reflected the composition of the broader U.S. refugee population as accurately as possible [18].
Data Collection
The survey was conducted via telephone interviews in 17 different languages, resulting in a population coverage of 72.2%. The sampling frame for the survey was Office of Refugee Resettlement (ORR) Arrivals Data System, with the principal applicant (the family member whose refugee case served as the basis for admission) being the sampling unit. The Principal Applicant (PA) answered on behalf of other household members, and the overall response rate achieved was 21% [18]. An introductory letter was mailed to the respondents, and multiple attempts were made to reach them [18]. However, it was challenging for the survey administrators to obtain current information from refugees who had been in the U.S. for an extended period, and there was a significant increase in resettlements in 2016 compared to the previous four years [19]. To address these limitations, the researchers at the Urban Institute, who assisted ORR in conducting the survey, set target respondent goals for each year of entry. The sample was intentionally skewed towards refugees who were resettled in 2017, as they were more likely to have up-to-date contact information and represented a larger pool of potential respondents. ORR successfully reached its targets and managed to contact all 6,100 households, resulting in 1,500 completed phone interviews with refugee households (Urban Institute, 2019). Trained interviewers collected information from the principals of each household via phone interviews, using proxy reporting for all other eligible refugees within the same household [18].
Participants
All the participants in the 2018 ASR were refugees who were at least 16 years or older who arrived in the United States in the last 5 years (between 2013 and 2017). During the interviews, the survey administrators spoke to the Principal Applicant (PA) of each family in the household, asking about the individuals whose refugee case was granted, as well as up to four other household members who were 16 years or older at the time of the interviews. These interviews resulted in reaching a total of 5,260 refugees who were sampled. In this study, however, the sub-sample of 1,007 refugees was used to include only those who responded to having chronic debilitating conditions [18].
Measures
Outcome variable: Chronic debilitating conditions was measured by asking refugee respondents, “does this person (insert name) have a physical, mental, or other health conditions that has lasted six or more months?” (a) limits the kind of work this person can do at a job? and/or (b) prevents this person from working at a job? The two items were summed up for a total score and were coded as “no” if the refugees didn’t have chronic debilitating conditions, and “yes” if refugees had chronic debilitating conditions. The conceptualization of ‘chronic debilitating conditions’ was adopted based on the previous study that used similar items for the outcome variable in this study [17].
Predictors: The selection of predictors was based on their availability in the ASR data which included gender, age, marital status, highest level of education completed, employment status, current English proficiency and immigration status. The predictors were recoded into different variables as delineated below.
Gender was assessed by asking respondents: “Is [insert name] male or female?” The answer choices were male, female, don’t know, and refused. Respondents who answered don’t know and refused were excluded from the analysis. Gender was recoded dichotomously as 0=male or 1=female.
Age was assessed by asking respondents: “What was [insert name] ‘s age at last birthday?” This was coded as 0= 0 to 17 years old, 1=18 to 24 years old, 2= 25 to 39 years, 3= 40 to 54 years, and 4= 55 or older.
Education level was assessed by asking participants: “What was the highest degree or certificate that [insert name] obtained before coming to the U.S.?” The answer choices included no education, primary, training in a refugee camp, technical certification, secondary (or high school diploma), university degree (other than medical), medical degree, other, don’t know, and refused. Training in the refugee camp, technical certification and university and medical degrees were combined. Respondents who answered don’t know and refused were coded as system missing. The highest level of education completed was recoded as 1=no education, 2=primary, 3=technical certification, 4=secondary school, 5=university degree, and 8=Other.
Employment status was assessed by asking the respondents: “Did [insert name] work at a job anytime last week? The answer choices included no, yes, don’t know, and refused. Respondents who answered don’t know and refused were excluded from the analysis. Employment status was recoded dichotomously as 0=currently not working, and 1=currently working.
Marital status was assessed by asking the respondents: “What is [insert name] ‘s current marital status? The answer choices included – now married, divorced, legally separated, never married, widowed, other, don’t know, and refused. Marital status was recoded to form a new categorical variable. Divorced, legally separated, widowed, others, never married were combined together due to lower response rates. This variable was recoded as 0= never married/other, and 1= married.
Current English proficiency was assessed by asking respondents: “How well does [insert name] speak English now?” The answer choices included --very well, well, not well, not at all, don’t know, and refused. First, this variable was reverse coded as not at all, not well, well, and very well, and those who answered don’t know, refused, and with missing values were coded as system missing. In the final step of the analysis, ‘not at all’ and ‘not well’ were combined and categorized as “poor,” and ‘well’ and ‘very well’ were categorized as ‘good.’ The current English proficiency variable was dichotomously coded as 0=poor or 1=good.
Immigration status was assessed by asking the respondents: “Has [insert name] applied to adjust his/her immigration status to that of a permanent U.S. resident?” The answer choices include yes, no, don’t know, and refused. Respondents who answered don’t know, not applicable, refused, and with missing values were excluded from the analysis. Therefore, immigration status variable was recoded dichotomously as 0=unadjusted or 1= adjusted.
Data Analysis
Prior to data analysis, missing data were addressed using multiple imputations to resolve uncertainty caused by missing data by generating multiple plausible datasets and appropriately combining the results from each dataset. Five copies of the dataset were created in the first step, with missing values replaced by imputed values. The second step involved applying standard statistical methods to fit the model, which included calculating the standard errors to account for the variability in the results due to missing values in the imputed datasets. Valid inferences were obtained by averaging the distribution of the missing data based on the observed data. Descriptive characteristics of the participants were obtained using frequencies and percentages. Chi-square tests (cross-tabulations) were employed to obtain the prevalence estimates between predictors and outcome variable (chronic debilitating conditions). Bivariate logistic regression was used to obtain crude ratios (unadjusted) for each predictor and outcome variable. Finally, multiple logistic regression was then performed to obtain adjusted odds ratios among all the predictors and the outcome variable. Both crude and adjusted odds ratios were evaluated and compared to assess the impact of confounding factors. IBM SPSS 28.0 software was utilized for all statistical analyses. A significance value of α = 0.05 was used throughout the study.
Ethical Considerations
This study utilized publicly available data from Annual Survey of Refugees (ASR). Since the study does not meet the regulatory criteria for human subject research, it was exempted from the Institutional Review Board (IRB) in accordance with Lewis University’s guidelines.
Results
Descriptive characteristics of the refugee participants
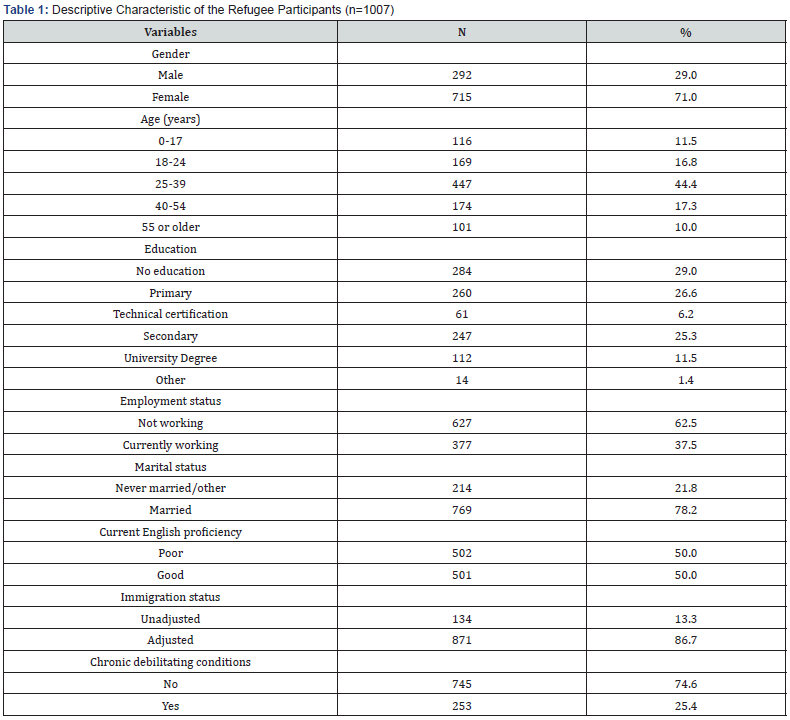
Table 1 shows the descriptive characteristics of the refugee participants. Data were collected from 1007 eligible refugees; 71% were females, 44.4% were between 25 and 39 years old, 29% had no education, and 37% were currently working. A large majority of the refugees adjusted their immigration status to become permanent residents (86.7%) and were currently married (78.2%). Finally, about half of the refugees (50%) had good English proficiency, and 25.5% reported having chronic debilitating conditions.
The prevalence of chronic debilitating conditions among refugee participants
Table 2 shows the prevalence of chronic debilitating conditions among refugees. Regarding gender, 69% of the females reported having chronic debilitating conditions relative to 21.6% of their male counterparts. The prevalence of reported chronic debilitating conditions increased as refugees were become older: 0 to 17 years (7.8%), 18 to 24 years (11.4%), 25 to 39 years (21.7%), 40 to 54 years (41.3%) and 55 years or older (57.6%). Pertaining to education level, chronic debilitating conditions were reported among refugees with no education (29.3%), primary education (29.2%), secondary education (21.2%), university degree (20.5%), technical certification (16.9%) and other (14.3%), respectively. Additionally, only 13.2% of refugees with chronic debilitating conditions reported currently working compared to 32.6% who were not working. More than one-quarter of married refugees (27.2%) reported having chronic debilitating conditions compared to those who were never married (20%). More than one-third of refugees with poor English proficiency (34.8%) reported having chronic debilitating conditions compared to those with good English proficiency (15.9%). Finally, 26.8% of refugees who adjusted their immigration status reported having chronic debilitating conditions, while only 15.2% of refugees who never adjusted their immigration status reported having chronic debilitating conditions in the United States.
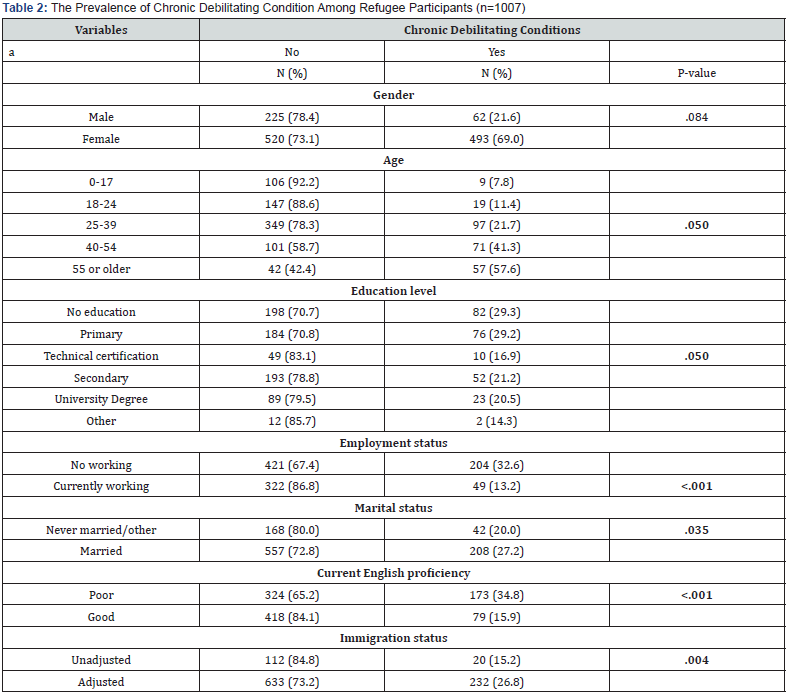
Note: Chi-square tests (cross-tabulations) were used to determine the prevalence estimates.
Predictors of chronic debilitating conditions among refugee participants
Table 3 shows the logistic regression results predicting the chronic debilitating conditions of the refugees. Gender was not significantly associated with chronic debilitating conditions among refugees. Regarding age differences, compared to refugees who were between 0 to 17 years, refugees who were between 18 to 24 years old (AOR= 2.19, 95% CI= 0.78 – 6.17), 25 to 39 years old (AOR=6.10, 95% CI=2.27- 16.39), 40 to 54 years old (AOR=14.00, 95% CI=5.08 -38.60), and 55 years or older (AOR=18.06, 95% CI=6.54- 49.85) had the highest odds of reporting chronic debilitating conditions. In regard to education level, refugees who completed secondary education were less likely to report chronic debilitating conditions only in the unadjusted model (OR=0.60, 95% CI = 0.44 - 0.97). However, after covariates adjustments, education was not significantly associated debilitating conditions. When it comes to education, refugees who were currently working were less likely to report chronic debilitating conditions compared to those who were not working (AOR=0.40, 95% CI=0.27- 0.59). Similarly, married refugees had lower odds of reporting chronic debilitating conditions than those who were never married/other (AOR=0.57, 95% CI=0.33 -0.98). Refugees with good English proficiency were less likely to report chronic debilitating conditions compared to those with poor English proficiency (AOR=0.61, 95% CI=0.42-0.91). Finally, refugees who adjusted their immigration status had the highest odds of reporting chronic debilitating conditions compared to those who never adjusted their immigration status (AOR=2.34, 95% CI=1.29- 4.24).
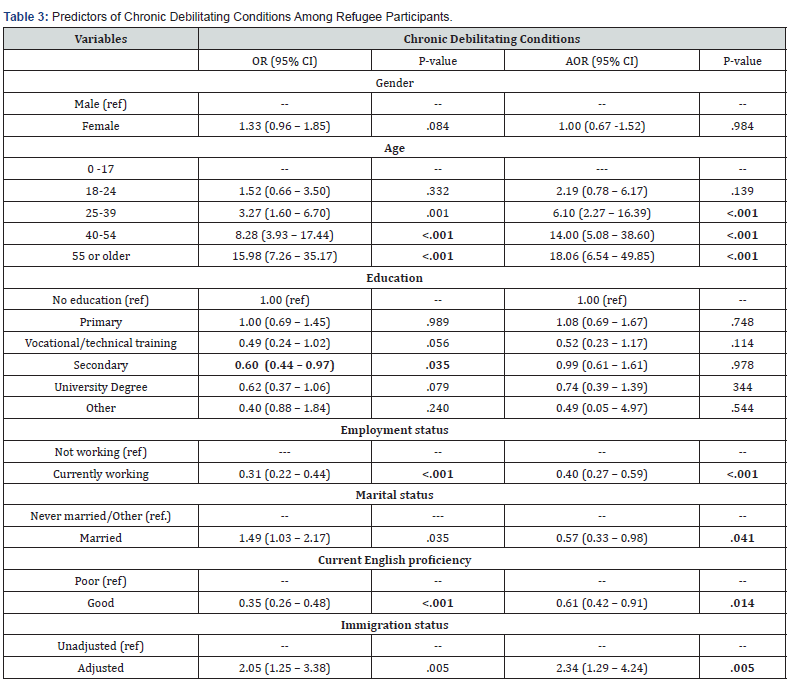
Note: Significance level= p<.05, bivariate and multiple logistic regression were conducted to determine significant association between independent and outcome variable.
Discussion
This study examined the prevalence of developing chronic debilitating conditions, as well as multiple factors that predict the risk of developing chronic debilitating conditions among refugees resettled in the United States. In this study, 25.5% of the refugees reported having chronic debilitating conditions. It was revealed that chronic debilitating conditions exacerbated as refugees became older - implying the variations of health status based on age differences of the refugees. For instance, the odds of having chronic debilitating conditions were higher for refugees between 18 to 24 years (11.4%), 25 to 39 years (21.7%), 40 to 54 years (41.3%), and 55 years or older (57.6%) relative to those who were between 0 to 17 years (7.8%). This is consistent with the previous studies that linked aging to an increased risk of pre-existing health conditions, such as arthritis, diabetes, hypertension, or heart disease, and cognitive impairments, which can continue to affect the physical and mental health of refugees even after resettlement [20,21]. Additionally, older refugees may have experienced prolonged conflict and trauma in their home countries, which can have lasting physical and mental health consequences, thus leading to an increased risk of developing chronic debilitating conditions in their host country.
The education refugees attain before leaving their home country can influence their health outcomes Krafft et al. [22]. In the current study, we found that having secondary education was associated with a lower likelihood of reporting chronic debilitating conditions among refugees only before the adjustment of the model, suggesting that education was not the stronger predictor of chronic debilitating conditions for refugees. However, we noted that refugees with lowest education status, including those without education (29.3%) and primary education (29.5%), had higher rates of reporting chronic debilitating conditions, while those with at least technical certification (16.9%), secondary education (21.2%) and university degree (20.5%) had lower rates of reporting chronic debilitating conditions. It is possible that refugees with higher levels of education may have better health literacy and informed about the preventive health measures, potentially reducing their risk of developing chronic debilitating conditions. In contrast, refugees with limited educational opportunities in the host country may face greater challenges in navigating the healthcare system and understanding health information, thereby increasing the potential risk of developing chronic debilitating conditions.
Regarding employment status, the findings in this study indicated that refugees who were currently working had lower likelihood of reporting chronic debilitating conditions. Employment provides refugees financial stability essential for meeting their basic needs, including access to food, shelter, and healthcare. A lack of employment opportunities can result in economic insecurity, exacerbating health-related stressors. The stress associated with unemployment can have adverse effects on physical health [23]. Chronic stress can contribute to various health problems, including cardiovascular and weakened immune systems [24]. Employment often comes with health insurance or access to employer-sponsored healthcare programs. Unfortunately, without employment, refugees may struggle to afford healthcare services, including necessary medications and medical treatments. The inability to secure employment can further lead to prolonged frustration, hopelessness, low self-esteem, and development of mental problems such as anxiety and depression [25]. Therefore, host countries and organizations involved in refugee resettlement must focus on policies and initiatives promoting economic integration and employment opportunities for refugees. This may include providing refugees with job training and opportunities to acquire skills in demand in the current local labor market, which can enhance their employability. Access to stable employment can significantly improve the health and well-being of refugees, while unemployment can lead to various health challenges, including the chronic debilitating conditions.
Marriage often provides emotional and practical support that can impact an individual’s financial situation, as married individuals may also have access to a spouse who can offer caregiving and emotional assistance, thereby positively affecting their ability to cope with chronic debilitating conditions [26]. This concurs with the findings in the current study that demonstrated that refugees who were married had were less likely to report chronic debilitating conditions. This implies that marital status can influence health-related behaviors. For example, married individuals may be more likely to engage in healthier behaviors, such as regular exercise and a balanced diet, and access to basic healthcare due to the influence and support of their spouse. In the United States, married couples may be more likely to have health insurance coverage through one spouse’s employer and may be more inclined to seek medical attention when needed, and combined household incomes may provide more financial resources to afford necessary healthcare and medications for refugees, thus reducing the risk of chronic debilitating conditions.
Language barriers contribute to health disparities, particularly among immigrant refugee populations [27]. In the present study, we found that refugees with good English proficiency (15.9%) were less likely to report chronic debilitating conditions compared to those with poor English proficiency (34.8%). Disparities in chronic debilitating conditions may exist among refugees with limited language proficiency. Having language proficiency empowers refugees to advocate for their health needs, which is unlikely to voice their concerns about their healthcare if they have language barriers [28]. Refugees with language barriers may have higher rates of undiagnosed or poorly managed chronic conditions due to difficulties in seeking care and understanding preventive measures. Effective communication between patients and healthcare providers is essential for correctly diagnosing and treating chronic conditions. Limited language proficiency can hinder the ability to describe symptoms, understand treatment plans, and ask questions about medications and side effects. In order to address language barriers in refugee healthcare, healthcare systems, and providers can adopt several strategies such as offering professional interpreter services in person or via telehealth to facilitate communication during medical appointments. Additionally, healthcare providers should receive training in culturally competent care to better understand refugee populations’ diverse backgrounds and needs. Providing healthcare materials in multiple languages can enhance refugees’ comprehension of health-related information. Employing cultural mediators who share the same language and cultural background as refugees can foster effective communication and trust. When interacting with refugees, healthcare staff should also receive training emphasizing sensitivity to language and cultural differences.
Finally, the findings of this study indicated that refugees who adjusted their immigration status to become permanent residents were more likely to report chronic health conditions compared to those who never adjusted their immigration status. Immigration status intersects with various social determinants of health, such as employment, housing, and education. For example, individuals with precarious immigration status may be more likely to work in low-paying jobs without health insurance, live in substandard housing conditions, or face discrimination, all of which can affect health outcomes. Eligibility for public health programs, such as Medicaid, can be influenced by immigration status as well. Limited access to these programs can affect an individual’s ability to manage their health conditions effectively. Immigration status can also contribute to elevated stress levels and mental health issues. Chronic stress is a known risk factor for various health conditions, including cardiovascular diseases, diabetes, and mental health disorders [20]. When refugees are officially recognized as refugees by the host country, they gain legal protection and access to certain rights and services. This recognition can include access to healthcare services, education, and social support, which can positively impact their health and mental health. While recognized refugees may still face mental health challenges due to trauma and displacement, they often have access to mental health services and support networks, which can mitigate the impact of these challenges. Recognized refugees often have the legal right to work in the host country. Employment can provide financial stability, a sense of purpose, and social connections that positively affect physical and mental health.
Limitations of the Study
The study has several limitations worth noting. First, this study’s use of a cross-sectional research design makes it difficult to draw causal inferences. The sample was drawn as a fresh crosssection by cohort, and there was no longitudinal component in the current study. Some of the variables had more than 20% missing cases. Second, this study depended on self-reported data, which may lead to socially desirable responses. In some households, proxies were used that could have led to missing data and inaccurate representations of the refugees’ perceptions within the household. Also, since some refugees could not properly speak English, limited translation was available, and the data collection solely depended on telephone administration, the results may not have represented all refugees, and some important information may have been lost due to language barriers. The survey may also not be representative of the most recently resettled refugees, and comparison to ASRs is recommended to understand temporal trends. However, the strength of this study included using nationally representative data with a large sample size that can be generalized to other refugees resettled in the United States.
Conclusion
This study provides a more comprehensive understanding of the prevalence and potential predictors of chronic debilitating conditions for refugees resettled in the United States. Specifically, this study showed that 25.5% of the refugees reported having chronic debilitating conditions. It was further indicated that age, employment, marital status, English language proficiency, and immigration status were significantly associated with chronic debilitating conditions among refugees resettled in the United States. Interventions should be tailored towards increasing opportunities for education, and employment to help refugees to have better health literacy and increased financial resources to access healthcare services. Additionally, language barriers to healthcare can be addressed by providing language and interpretation services, thus increasing understanding on the best ways to access healthcare and reducing the potential risk of chronic debilitating conditions among refugees resettled in the United States.
Funding
No funding was obtained for the completion of the study.
References
- Kennedy JD, Moran S, Garrett S, Stanley J, Visser J, et al. (2020) Refugee-like migrants have similar health needs to refugees: a New Zealand post-settlement cohort study. BJGP open 4(1).
- Chipalo E (2023) Exposure to Violence and Other Characteristics Associated with Posttraumatic Stress Disorder Among Students in Nyarugusu Refugee Camp, Tanzania. The University of Alabama.
- Lamb CF, Smith M (2002) Problems refugees face when accessing health services. New South Wales public health bulletin 13(7): 161-163.
- Sagaltici E, Alpak G, Altindag A (2020) Traumatic life events and severity of posttraumatic stress disorder among Syrian refugees residing in a camp in Turkey. Journal of loss and trauma 25(1): 47-60.
- Fazel M, Wheeler J, Danesh J (2005) Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. The lancet 365(9467): 1309-1314.
- Kiss V, Pim C, Hemmelgarn BR, Quan H (2013) Building knowledge about health services utilization by refugees. Journal of immigrant and minority health 15: 57-67.
- Pavli A, Maltezou H (2017) Health problems of newly arrived migrants and refugees in Europe. Journal of travel medicine 24(4): tax016.
- Mirza M, Luna R, Mathews B, Hasnain R, Hebert E, et al. (2014) Barriers to healthcare access among refugees with disabilities and chronic health conditions resettled in the US Midwest. Journal of immigrant and minority health 16: 733-742.
- Broemeling AM, Watson DE, Prebtani F (2008) Population patterns of chronic health conditions, co-morbidity and healthcare use in Canada: implications for policy and practice. Healthcare Q11(3): 70-76.
- Chipalo E, Suntai Z, Mwima S (2022) Factors Associated with Receiving Supplemental Nutrition Assistance Program (SNAP) Among Newly Resettled Refugees in the United States. J Soc Soc Welfare 49: 135.
- Pyke J, Doughney J, Kyle L, Macdonald F (2004) Refugees in the Labour Market: Looking for cost-effective models of assistance.
- Yakushko O, Backhaus A, Watson M, Ngaruiya K, Gonzalez J (2008) Career development concerns of recent immigrants and refugees. Journal of Career development 34(4): 362-396.
- Kemp C (1993) Health services for refugees in countries of second asylum. Int Nurs Rev 40(1): 21-24.
- Portes A, Kyle D, Eaton WW (1992) Mental illness and help-seeking behavior among Mariel Cuban and Haitian refugees in South Florida. Journal of health and social behavior 283-298
- Straiton ML, Myhre S (2017) Learning to navigate the healthcare system in a new country: a qualitative study. Scandinavian journal of primary health care 35(4): 352-359.
- Divkolaye NSH, Burkle Jr, FM (2017) The enduring health challenges of Afghan immigrants and refugees in Iran: a systematic review. PLoS Currents 9.
- Baumann KJ, Adera T (2022) Sociodemographic Characteristics and Inadequate Usual Sources of Healthcare in a National Sample of US Refugees. International journal of environmental research and public health 19(12): 7234.
- Urban Institute (2018) Annual survey of refugees. Ann Arbor, MI: inter-university consortium for political and social research.
- Refugee Processing Center. (2020) Worldwide refugee admissions processing system.
- Rosenthal T, Touyz RM, Oparil S (2022) Migrating populations and health: risk factors for cardiovascular disease and metabolic syndrome. Current Hypertension Reports 24(9): 325-340.
- Zaimi NHA, Supaat DI (2023) Flood disasters in Malaysia: Examining the Impact on Older people’s Vulnerability and Right.
- Krafft C, Sieverding M, Salemi C, Keo C (2018) Syrian refugees in Jordan: Demographics, livelihoods, education, and health. Economic Research Forum Working Paper Series 141-172.
- Sharma SV, Chuang RJ, Rushing M, Naylor B, Ranjit N, et al. (2020) Peer reviewed: Social determinants of health–related needs during COVID-19 among low-income households with children. Preventing chronic disease 17.
- Seiler A, Fagundes, CP, Christian LM (2020) The impact of everyday stressors on the immune system and health. Stress challenges and immunity in space: From mechanisms to monitoring and preventive strategies 71-92.
- Lee JO, Jones TM, Yoon Y, Hackman DA, Yoo JP, et al. (2019) Young adult unemployment and later depression and anxiety: does childhood neighborhood matter? Journal of youth and adolescence, 48, 30-42.
- Peacock S, Sethi B, Williams A, Duggleby W, Bayly M, et al. (2017) Older adult spouses with multiple chronic conditions: challenges, rewards, and coping strategies. Can J Aging 36(2): 209-222.
- Chang CD (2019) Social determinants of health and health disparities among immigrants and their children. Current problems in pediatric and adolescent health care 49(1): 23-30.
- Hawkins MM, Schmitt ME, Adebayo CT, Weitzel J, Olukotun O, et al. (2021) Promoting the health of refugee women: a scoping literature review incorporating the social ecological model. Int J Equity Health 20(1): 45.






























