Prevalence of Hospitalization for Schizophrenia, Schizotypical and Delusional Disorders in Brazil from 2017 To 2022
Lucas Tadeu Cerqueira Dos Santos, Mara Luiza Anunciação Rios Souza, Gustavo Fernandes Vieira, Isabelle Cristine Barbosa Pereira, Mariana Hellen do Carmo de Freitas*, Jean Lucas Almeida Canjirana dos Santos and Claras Malaquias Boaventura
Student o União Metropolitana para o Desenvolvimento da Educação e Cultura (UNIME), Lauro de Freitas, Bahia, Brazil
Submission:August 15, 2023;Published:September 12, 2023
*Corresponding author:Mariana Hellen do Carmo de Freitas, Student of União Metropolitana para o Desenvolvimento da Educação e Cultura (UNIME), Lauro de Freitas, Bahia, Brazil
How to cite this article:Mariana Hellen do Carmo de Freitas. Prevalence of Hospitalization for Schizophrenia, Schizotypical and Delusional Disorders in Brazil from 2017 To 2022. Glob J Intellect Dev Disabil. 2023; 12(3): 555840.DOI:10.19080/GJIDD.2023.12.555840
Abstract
Introduction: Considered a complex illness, schizophrenia is characterized by the presence of delusions, hallucinations, disorganized speech, grossly disorganized behavior and/or negative symptoms. Furthermore, delusional disorder constitutes a condition marked primarily by the presence of persistent delusions for at least 30 days. The impact caused on mortality by these diseases is highlighted, given that, according to epidemiological studies, schizophrenia, schizotypal and delusional disorders represent some of the main reasons for deaths from mental and behavioral disorders.
Objective: To analyze the prevalence of hospitalizations for schizophrenia, schizotypal and delusional disorders in Brazil from 2017 to 2022.
Method: This is a descriptive epidemiological study, whose data were obtained from the SUS Hospital Information System (SIH/SUS), by the Department of Informatics of the Unified Health System (DATASUS), at the electronic address (http://www2.datasus.gov.br), which was accessed on 20/ 04/2023. Data were collected from the “Epidemiological and Morbidity” section, using consolidated information on hospital morbidity, by place of residence, selecting the ICD-10 Schizophrenia, Schizotypal and Delusional Disorders. The following variables were used: gender, age group, average length of stay, cost of hospital services, with a time frame from 2017 to 2022. The collected data were systematized, grouped and calculated with the support of the Microsoft Office Excel 2021 application, using descriptive statistics (absolute and relative values). Because it is a study with secondary and aggregated data, open to public consultation and without personal identification, validation by the Research Ethics Committee was not required.
Results: The results show that during the period between January 2017 and December 2022, 405,660 patients required hospitalization for schizophrenia, schizotypal and delusional disorders in Brazil, with a total of 170,042 (41.92%) in the Southeast region, 97,689 (24.08%) in the Northeast region, 83,578 (20.60%) in the South region, 25,000 (6.16%) residents in the North region and 29,351 (7.24%) in the Midwest region, with a predominance of males in all regions of the country. In addition, the distribution of hospitalized patients according to age shows much higher numbers of hospitalizations for the disorders studied in the age group between 20 and 59 years old, with percentages above 83% in all regions of the country. With regard to cost, the data reflect a higher per capita expenditure for the care of the population studied in the northeast region, when compared to the cost per individual in the southeast region. According to the analysis, the northeast region was also the region with the highest average days of hospitalization for these patients, totaling an average of 44 (forty-four) days, and the north region was the one with the lowest rate, with an average of only 18 (eighteen) days of hospitalization.
Conclusion: The spatial analysis revealed that the geographic distribution of these conditions is not uniform, with some regions of the country having a higher number of hospitalizations associated with these disorders. These findings highlight the importance of specific public programs and policies for regions with higher rates of morbidity and mortality.
Keywords: Schizophrenia; Schizotypal disorders; Hospitalizations; Morbidity
Introduction
Considered a complex illness, schizophrenia is characterized by the presence of delusions, hallucinations, disorganized speech, grossly disorganized behavior and/or negative symptoms, requiring the presence of at least two of these characteristics [1]. In addition, delirium, hallucinations or disorganized speech are necessary to fulfill the diagnostic criteria for schizophrenia, and this condition — which has a prevalence that varies between 0.3 and 0.7% — is also associated with considerable morbidity and mortality, considering the risk of suicide, social and professional dysfunction related to schizophrenia [1].
According to the Diagnostic and Statistical Manual of Mental Disorders (2014), ideas of reference, magical thinking, body illusions, vague thinking, paranoid ideation and social anxiety are situations that may be present in a patient with Schizotypal Personality Disorder. The impact caused on mortality by these diseases is highlighted, given that Schizophrenia, Schizotypal and Delusional Disorders were the main reasons for death from Mental and Behavioral Disorders observed in females in the state of São Paulo between 2017 and 2020 [2].
Furthermore, delusional disorder, constitutes a condition marked primarily by the presence of persistent delusions for at least 30 days. The clinical picture is variable, differentiating it into: erotomanic (fixed idea that someone is in love with him), grandiose (conviction that he has made an important discovery or that he has a great insight, status or talent), persecutory (the certainty that he is being deceived, persecuted, observed or that someone is trying to do him some harm), somatic (presence of functional or sensory body changes) or jealousy [3]. The impact of symptoms on quality of life places the patient at a higher risk of suicidal ideation and behavior [4].
Schizophrenic and delusional spectrum disorders contribute to a significant morbidity and mortality profile in affected patients, increasing the risk of comorbidities such as diabetes mellitus, obesity, cardiovascular diseases, chronic respiratory diseases and other mental disorders, as well as dependence syndromes due to the use of drugs and psychoactive substances [5]. In this context, the outcomes of schizophrenic spectrum disorders draw attention to the need for an accurate diagnosis, to avoid underdiagnosis and therapeutic delay that can increase the risk of suicide in this population, considering that, globally, one in every 100 people with mental disorders die by suicide and, in 2019, there were about 703,000 deaths by suicide, especially in patients over 50 years of age [6].
Therefore, it is extremely important to identify the main factors that influence the maintenance of lasting vulnerabilities, with regard to the delay in diagnosis, poor therapeutic adherence and negative outcomes inherent in intentionally ending one’s own life, since social reintegration, prevention and reduction of secondary complications linked to addictions or chronic pathologies of individuals with such comorbidities is the basic principle of the abolition of the previously clarified symptoms. Thus, the present study seeks to analyze the prevalence of hospitalizations for schizophrenia, schizotypal and delusional disorders in Brazil from 2017 to 2022.
Methods
This is a descriptive epidemiological study, whose data were obtained from the SUS Hospital Information System (SIH/SUS), made available by the Department of Informatics of the Unified Health System (DATASUS), at the electronic address (http:// www2.datasus.gov.br), which was accessed on 04/20/2023. Data were collected from the “Health Care” section, using consolidated information from hospital production, by place of residence, Region/Units of the Federation, selecting the ICD-10 Schizophrenia, Schizotypal and Delusional Disorders. For the morbidity analysis, data were collected from the “Epidemiological and Morbidity” section, selecting the SUS hospital morbidity item, by place of residence, Region/Units of the Federation, using the variables: sex, age group, average length of stay, cost of hospital services, whose selected period was from 2017 to 2022. The collected data were systematized, grouped and calculated with the support of the Microsoft Office Excel 2021 application, using descriptive statistics (absolute and relative values), presenting the findings in tables and graohs. Because it is a study with secondary and aggregated data, open to public consultation and without personal identification, validation by the Research Ethics Committee was not required.
Results
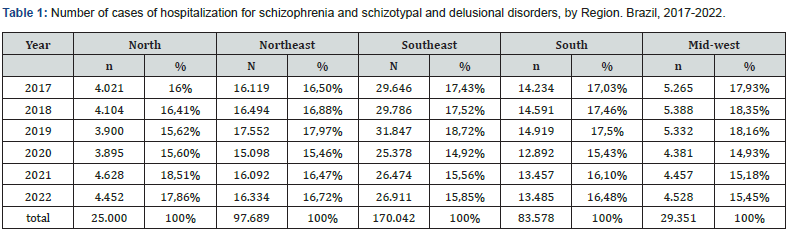
The results of the present study reveal that during the period between January 2017 and December 2022, 405,660 patients required hospitalization for schizophrenia, schizotypal and delusional disorders in Brazil, with a total of 25,000 (6.16%) residing in the north region, 97,689 (24.08%) in the northeast region, 170,042 (41.92%) in the southeast region, 83,578 (20.60%) in the south region and 29,351 (7.24%) in the midwest region during the surveyed period. A supremacy of the Southeast region can be observed when analyzing the numbers separately (Table 1).
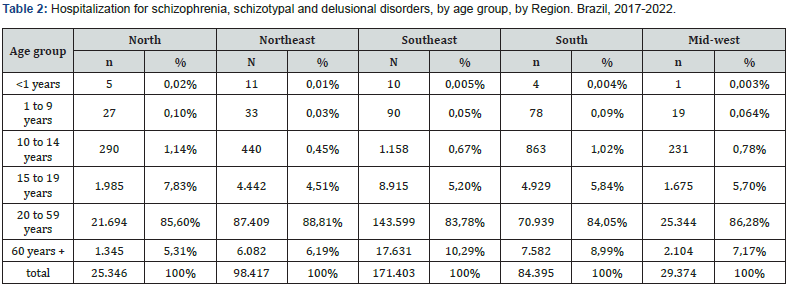
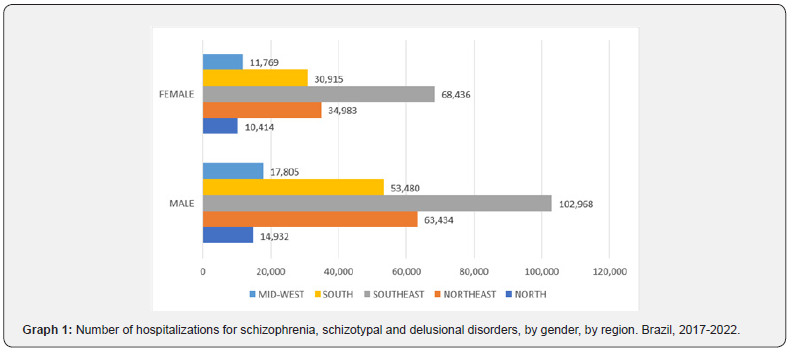
Graph 1 contains data related to hospital admission rates for schizophrenia, schizotypal and delusional disorders according to patient gender. Based on this information, it is concluded that there is a predominance of males in all regions of Brazil, while Table 2 shows the distribution of hospitalized patients according to age, which demonstrates much higher numbers of hospitalizations for the disorders studied in the age group between 20 and 59 years old, with percentages above 83% in all regions of the country. Based on this finding, it is noted that the public aged less than 1 year up to 14 years old had lower rates raised and populations aged 15 and 19 years old presented results similar to those recorded for people aged 60 years or more.
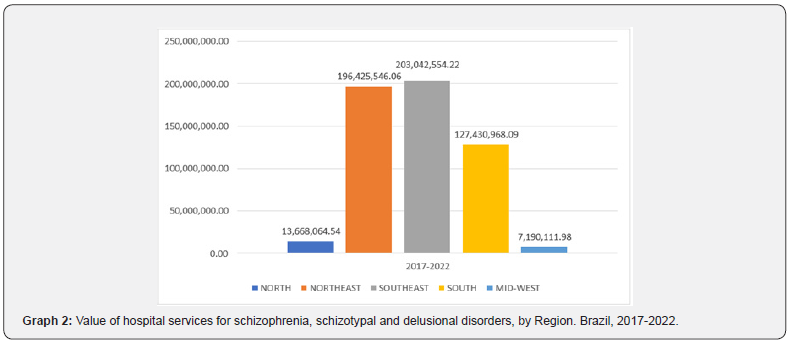
The information listed in Graph 2 translates into a higher per capita cost for the care of the population studied in the Northeast region, when compared to the cost per individual in the Southeast region. It was observed that the total amount invested in hospital care for people who suffered from schizophrenia, schizotypal and delusional disorders was R$ 196,425,546.06 (one hundred and ninety-six million, four hundred and twenty-five thousand, five hundred and forty-six reais and six cents) in the northeast region, from R$ 203,042,554.22 (two hundred and three million, fortytwo thousand, qui one hundred and fifty-four reais and twentytwo cents) in the southeast region and R$ 127,430,968.09 (one hundred and twenty-seven million, four hundred and thirty thousand, nine hundred and sixty-eight reais and nine cents) in the south region. Considering the information in table 1, which recorded a total of 97,689 hospitalizations in the northeast region, 170,042 hospitalizations in the southeast region and 83,578 hospitalizations in the south region, it is concluded that the average cost per person was R$ 2,010.72 (two thousand, ten reais and seventy-two cents/person) in the northeast region, of R$ 1,195.07 (one thousand, one hundred and ninety-five reais and seven cents/person) in the southeast region and R$ 1,524.70 (one thousand, five hundred and twenty-four reais and seventy cents/ person) in the south region.
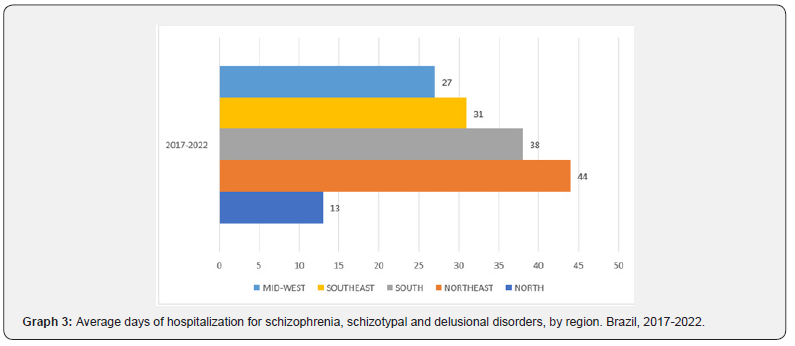
According to the analysis, the Northeast region was also the region of Brazil with the highest average number of days of hospitalization for these patients, as can be seen in Graph 3. While the Northeast region had an average of 44 (forty-four) days of hospitalization, the South region had an average of 38 (thirty-eight) days, the Southeast region had 31 (thirty-one) days, the Midwest region had 27 (twenty-seven) days and the North region had the lowest index, with an average of just 18 days of hospitalization.
Conclusion
Based on the results obtained in this epidemiological study, it is possible to conclude that schizophrenia, schizotypal and delusional disorders represent an important public health problem in Brazil. The morbidity and mortality analysis showed that these conditions are associated with a higher probability of hospitalization, representing high costs for health services. These results suggest that there is a need to improve access to mental health services and improve the diagnosis and treatment of these disorders in the country. Spatial analysis revealed that the geographic distribution of these conditions is not uniform, with some regions of the country having a higher number of hospitalizations associated with these disorders. These findings highlight the importance of specific public programs and policies for regions with higher rates of morbidity and mortality.
In conclusion, this study provides important insights into morbidity from schizophrenia, schizotypal and delusional disorders in Brazil in the years 2017 to 2022. The results highlight the need to improve detection, treatment and access to mental health services for these conditions. It is expected, therefore, that these results can be used to guide public mental health policies that are more effective and directed towards the Brazilian population.
References
- American psychiatric association (2014) Espectro da esquizofrenia e outros transtornos psicóticos. In: american psychiatric association. DSM-V: manual diagnóstico e estatístico de transtornos 5. Ed. Porto alegre: artmed pp: 87-122.
- Ramos GSL, Silva GMM (2021) Transtorno mental e comportamental no estado de são paulo: variações da mortalidade e morbidade de 2017 A Colloq vitae 13(2)12-18.
- Diniz E, Fonseca l, Gadelha A (2022) Espectro da esquizofrenia e outros transtornos psicó In: nardi AE, Silva AG, quevedo, j(org). Tratado de psiquiatria da associação brasileira de psiquiatria. Porto alegre: artmed 19.
- Gonzáles-rodríguez A, Oriol Molina Andreu, Rafael Penadés Rubio, Rosa Catalán Campos, Miguel Bernardo Arroyo (2014) Clinical significance of suicidal behaviour in delusional disorder: A 44 case-series descriptive study. Med Clin (Barc) 142(7): 299-302.
- Moreira WN, oliveira KC (2021) Comorbidades clínicas em indivíduos com transtornos psicóticos atendidos em hospital universitá Revista eletrônica acervo saúde13(12): 1-9.
- Organização mundial de saúde (2022) Relatório mundial de saúde mental: transformando a saúde mental para todos. Isbn 978-92-4-004933-8.






























