Healthcare Strategies in Subjects with Intellectual Disabilities During COVID-19 Pandemic
Marilisa Toma1*, Mariachiara Perrotta1, Marisa Roncati2, Dolaji Henin1, Gaia Pellegrini1, Cristina Allievi1, and Claudia Dellavia1
1Department of Biomedical, Surgical and Dental Sciences, Università Degli Studi di Milano, Italy
2Department of Prosthodontics, Alma Mater Studiorum, Università di Bologna, Italy
Submission: December 20, 2021; Published: January 26, 2022
*Corresponding author: Marilisa Toma, DDS, PhD, Department of Biomedical, Surgical and Dental Sciences, via Mangiagalli 31, 20133 Milano. Università degli Studi di Milano, Italy
How to cite this article:Toma M, Perrotta M, Henin D, Pellegrini G, Allievi C, et al. Healthcare Strategies in Subjects with Intellectual Disabilities During COVID-19 Pandemic. Glob J Intellect Dev Disabil, 2022; 9(4): 555768. DOI:10.19080/GJIDD.2022.09.555768
Abstract
In the period of Covid-19 pandemic, attention to oral health and hygiene in patients with intellectual or physical disabilities is mandatory. The limited manual skills and motor impairments hinder the maintenance of oral health. With that in mind, devices that facilitate the removal of food debris and dental plaque have been developed and associated with solutions to reduce the overall microbial load. A total of 210 athletes were screened at the Italian Special Olympics National Games by participating volunteer dentists. Oral health-related data were collected and recorded using the Special Smiles official screening form by calibrated examiners. After the screening, the athletes were invited to eat two biscuits in order to simulate food and plaque deposition on teeth surfaces. Then subjects were randomly assigned to 2 groups, test and control, to perform oral hygiene procedure with a gauze embedded with Chlorhexidine 0,12% (Digital Brush®) and standard size toothbrush, respectively. Oral Hygiene index and Food debris index were applied to both groups to evaluate the oral hygiene efficacy before (t0) and after (t1) the brushing procedure. For both analyzed indexes no significant difference was evidenced between the two groups while from t0 to t1 was recorded a significant improvement in all the athletes. In conclusion, a combination of simple and quick mechanical removal techniques and antimicrobial chemical agents could be an efficacious option.
Keywords: Intellectual disabilities; Special athletes; Oral hygiene; Covid-19; Sars-Cov-2; Home care dental devices; Preventive, dentistry Digital Brush
Introduction
In the COVID-19 pandemic, paying attention to oral hygiene procedures and oral health in patients with intellectual disability (ID) is mandatory. Intellectual or physical disability often make oral hygiene maintenance very difficult to achieve [1,2] due to limited manual skills, poor reflexes, and motor impairments.
Moreover, subjects with ID are susceptible to oral diseases because of anatomical anomalies such as high palate, maxillary hypoplasia, malocclusions, open bites and abnormalities in tooth morphology or eruptive pattern and due to dental parafunctions, such as lip-biting and tongue thrusting. ID subjects have been reported to have poorer oral hygiene, higher plaque levels, more severe gingivitis, and periodontitis than the population without ID [1].
Dental plaque is a bacterial aggregate that adhering to teeth or dental implants may cause decays, periodontal and peri-implant diseases [3]. Mechanical removal of dental plaque allows to prevent the onset of oral diseases and to reduce the microbial load in the oral cavity [4].
COVID-19 pandemic determined movement restrictions, fears of medical care and risk of cross-infections that limited the access to dental practice in the general population, thus highlighting the need for new effective strategies to improve oral health especially in patients with ID. These strategies would aim to i) educate and precociously diagnose oral diseases and ii) to potentiate self-oral care. Considering the first objective Tele-dentistry may represent an option to allow consultation, diagnosis, triage and monitoring of patients. On the other hand, the use of supplementary devices able to remove residual debris and diminish microbial load may represent a feasible strategy for self-oral care potentiation in ID patients.
Recently, a disposable product consisting of a gauze containing 0.12% chlorhexidine (Digital Brush Enacare, Micerium S.p.A., Genoa, Italy- DB) has been developed to combine mechanical and chemical effects in self-oral hygiene maintenance, and therefore to reduce the overall oral microbial load. This device can be easily rolled around a finger to remove food debris and dental plaque with simple movements, thus representing a safe tool, especially in patients with motor disturbances. Thanks to its portability and manoeuvrability, DB may be proposed in all individuals combined with conventional oral hygiene procedures and/or in those cases where toothbrushing is not possible as in subjects having frequent meals throughout the day such as athletes.
Special Olympics is an international nonprofit organization founded in 1968 to improve the quality of life of people with intellectual disabilities (ID), primarily through sports training and athletic competitions. Since its foundation, the control and the prevention of medical problems in the athletes attending the competitions have played a crucial role in assuring a safe performance while playing sports (16). Six Healthy Athletes Programs were thus planned to evaluate the health status of Special Olympians, including screenings for dental and oral conditions assessment [5]. During each event, volunteer dentists involved in the program educate the athletes with ID on how to maintain their daily oral care, by improving their ability to perform effective oral hygiene procedures. Oral hygiene control is very important for these athletes, but not so easy to achieve; they use to eat quite often to compete well, in addition, competitions usually last all day, so controlling plaque deposition represents a problem [6].
This study aimed to evaluate if DB is an effective tool to remove dental plaque in ID subjects attending Special Olympics games.
Methods
Study population
In this randomized case-control clinical trial, a total of 210 subjects were screened between the participants at the Italian Special Olympics National Games.
Inclusion and exclusion criteria
Adult athletes with the presence of at least all superior permanent incisors were recruited. Subjects were excluded based on the following criteria: permanent upper incisors presenting fracture, decays, prosthesis, fillings and signs of fluorosis/ discolouration; systemic medications that affect dentogingival conditions.
Study design
For each participant, the following oral health-related data were collected and recorded using the Special Smiles official screening form [7] by four calibrated examiners (volunteer dentists): presence of untreated caries, missing teeth, restorations, gingival health (signs), fluorosis, sealants, dental injuries and the oral hygiene habits [8]. Demographic data (drugs and alcohol assumption, smoke, life at home or in community and presence of syndromic diseases) were also collected.
After this “screening phase” the dental team of the “Special Smiles” program provided a detailed explanation of the protocol to all athletes and their legal companions to obtain their informed consensus to the study. All procedures were non-invasive, non-dangerous, and did not provoke pain or discomfort to the subjects, who were free to stop their examination at any moment. This standardized protocol of examination has been developed for the program “Special smiles” of Special Olympics by the US Centers for Disease Control and Prevention. The protocol of the study followed the indications of the Special Olympics committee and was approved by the Ethic Committee of National Special Olympics [7].
Figure 1 reports the flow chart of the study design. After inclusion into the study, athletes were invited to eat two glutenfree biscuits in order to simulate a regular meal and to help food and plaque deposition on teeth surfaces. Then, participants were randomly divided into 2 groups based on their syndromic/ non-syndromic intellectual disability: 1) test group, performing oral hygiene procedure with Digital Brush Chlorhexidine 0,12% (Enacare, Micerium S.p.A., Genoa, Italy), 2) control group, using standard size toothbrush (Ena Oral Care Toothbrush, Micerium S.p.A., Genoa, Italy; TB). The randomization was performed by tossing a coin.

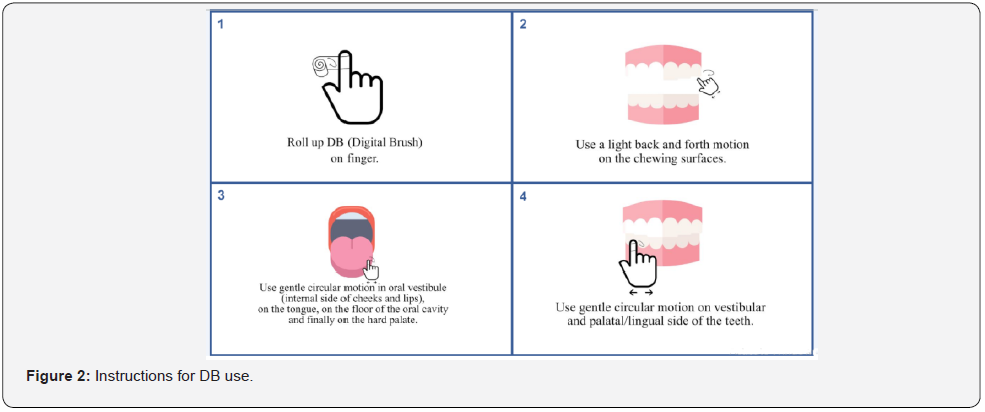
The dental team instructed the recruited athletes to obtain adequate oral hygiene. Subjects were given a detailed explanation for the correct use of DB (test group) using the roll motion technique: DB was wrapped around the index finger and utilized with a sweeping motion from the oral mucosa to the tooth surfaces in a cervico-incisal direction, similar to the roll brushing technique, for 2 minutes. It was also required to wipe DB in the oral vestibule (internal side of cheeks and lips), on the tongue, on the floor of the oral cavity and finally on the hard palate. Otherwise, for the control group, subjects were given a detailed explanation of the modified Bass brushing technique [9].
Subjects were asked to brush their teeth with TB or with DB, according to the given instructions as suggested by Roncati et al [10]:
i. Roll up DB on finger.
ii. Use a gentle circular motion on the vestibular and palatal/lingual side of the teeth.
iii. Use a light back and forth motion on the chewing surfaces.
iv. Use gentle circular motion in the oral vestibule (internal side of cheeks and lips), on the tongue, on the floor of the oral cavity and finally on the hard palate (Figure 2).
And they were invited to eat a plaque disclosing pill [11], to underline the remaining dental plaque deposition. Oral hygiene was evaluated on four anterior maxillary teeth using photographs (Canon Eos 5D Mark III, zoom 105mm and annular flash) taken just before (t0) and after (t1) the oral cleaning procedure, and using cheek retractors.
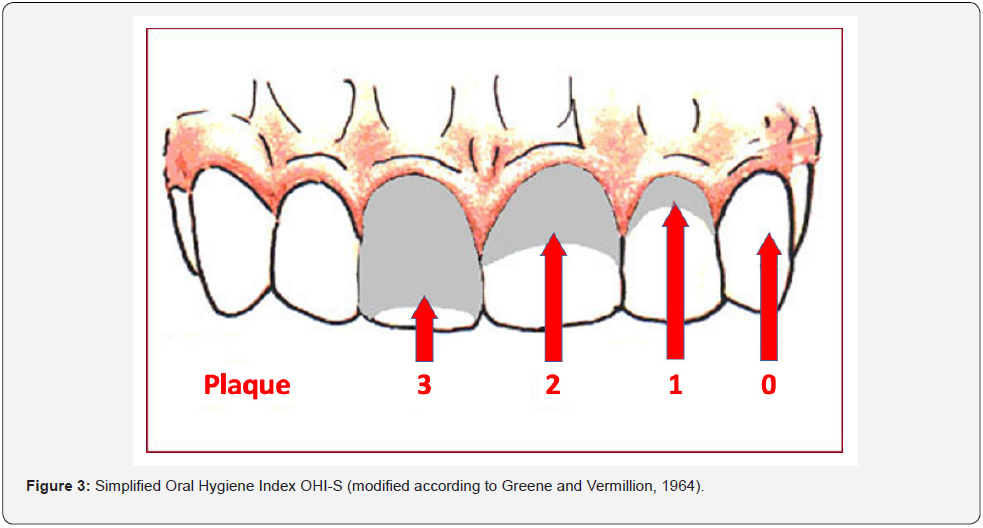
Incisor maxillary teeth were numbered from 1 to 4, from right to left for the quantitative analysis of dental plaque accumulation (Figure 3) [12]. On the pictures, the plaque accumulated on tooth surface scored as follows, dividing the buccal surface of dental crowns into three parts (cervical, medium, incisal): 0 no plaque; 1 soft debris covering not more than one third of the tooth surface; 2 soft debris covering more than one third, but not more than two thirds, of the exposed tooth surface; 3 soft debris covering more than two thirds of the exposed tooth surface. The mean value of the 4 teeth was computed in each subject (OHI-S).
Also, a qualitative evaluation of the food remnants in the recesses of the oral cavity was performed at the end of the visit and the eventual presence of any residual debris was recorded in each subject by means of the Food Debris Index (FDI) [13]. The evaluation was carried on by two different blind experienced observers in order to assess analysis repeatability.
Data elaboration and statistical analysis
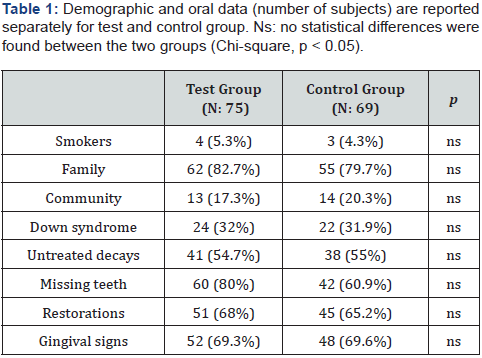
In both test and control groups, the total number of subjects who smoked, who lived with family or in community and who had Down syndrome was calculated. Also, the total number of subjects with untreated decays, missing teeth, restorations and gingival signs were computed for each group. For all these demographic and oral health related data taken at t0, mean and standard deviation were computed for each group, and the frequency of distribution between test and control groups was assessed by Chi-Squared test.
For oral hygiene evaluation, the mean and standard deviation of OHI-S and FDI were calculated for each group and time point. OHI-S and FDI were compared in each group at t0 and t1 with a paired sample t-test (t0 vs t1 in both groups); an unpaired sample t-test was used to analyze differences in the oral hygiene conditions between groups at each timepoint. Paired sample t-test was applied to verify repeatability, comparing scores taken by two different observers (operators 1 and 2). Values of p < 0.05 were considered significant.
Results
Study population
According to inclusion and exclusion criteria, 144 adult subjects (89 males and 55 females, age range 18-62 years; mean 31.7 years) were included in the present study and were therefore randomly divided into the 2 groups. The test group was composed of 75 subjects (45 males and 30 females, age range 18-62 years, mean 31.3); the control group was composed of 69 subjects (44 males and 25 females, age range 18-56 years, mean 32.8) (Table 1). No statistical differences were found between the two groups for both oral screening and demographic recorded data. Considering the presence of syndromic conditions, only Down syndrome was found, while the remaining subjects were affected by unspecified intellectual disability. The distribution of syndromic and nonsyndromic subjects was similar in the test and control groups. Considering the two groups as a unique population regarding demographic data it results that the majority of the special athletes lived with their families. DS and non-syndromic subjects had a similar percentage of individuals living with their families (p > 0.05); only about 4% - 5% of the participants were smokers in both test and control groups. Overall, 75% of the participants reported cleaning their mouth at least once daily, 20% reported brushing their teeth two to six times a week, only 3% cleaned their teeth once a week, and 2% brushed their teeth less than once a week. No sex and syndromic differences were found concerning oral hygiene (p > 0.05). In addition, approximately 70% of athletes had “gingival signs”. Non-syndromic subjects had a significantly greater prevalence of untreated caries than DS athletes (p < 0.05).
Data analysis
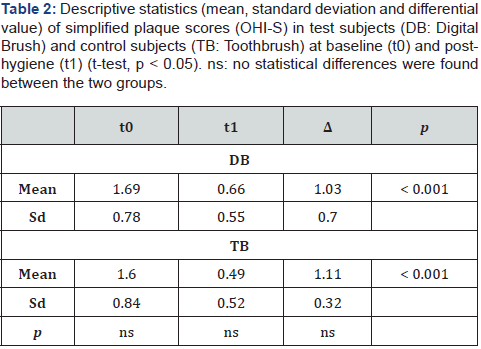
Since no statistical differences were found between OHI-S and FDI scores taken by two operators (p > 0.05), we considered results taken by operator 1, randomly chosen. For both groups and both OHI-S and FDI, mean scores were analysed comparing the two time points in the same group and each time point t0 and t1 among the two groups.
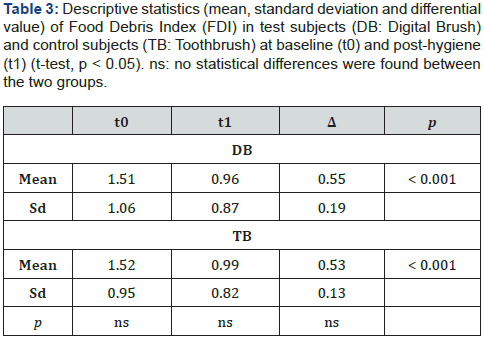
The difference between t0 (DB) and t0 (TB), t1 (DB) and t1 (TB), Δ(DB) and Δ(TB) was not statistically significant (p > 0.05). Significant difference was evidenced between t0 and t1 in both groups (p < 0.001) considering both indexes (Figure 4 & 5) (Table 2 & 3).


Discussion and Conclusion
In the current study, we compared the efficacy of a handy device for oral hygiene (Digital Brush) with the conventional TB in Special Olympians participating in Italian national competitions. The examinations demonstrated that DB seems to be an effective plaque removal device.
According to the current data, DB showed a satisfactory removal of food debris and dental plaque similarly to the traditional brushing technique with a plaque score reduction in all the analyzed teeth. In addition, the procedure was demonstrated as simple, quick and easy to learn for all subjects with ID. Even if TB remains the gold standard device for oral hygiene procedures, disposable and handy products that simplify the cleaning may be useful in addition to routine oral hygiene techniques in all subjects presenting impaired dexterity due to mental and physical disorders either permanent or temporary. Finger tactile receptors can guide cleaning movements to reach frequently neglected dental surfaces in the posterior lingual/palatal areas and food remnants in oral cavity recesses, thus improving the thoroughness and efficiency of cleaning [13].
This advantage could be more evident in subjects with ID living in residential institutions where the support of families for oral cleaning procedures is lacking. In addition, these kinds of tools may also be proposed as an additional hygiene device in subjects without disabilities when lifestyles unbalance the ratio between food/drink intake and oral hygiene procedures. Modern habits imply a frequent assumption of junk food, but a not corresponding frequency in oral care especially in people that spend a lot of time away from home.
COVID-19 pandemic highlighted the possibility to transmit the infection through droplets from the oral cavity and to develop severe pulmonary complications COVID-19 related, due to the inhalation of bacteria from the oral cavity. For these reasons, increased attention to oral hygiene procedures and oral health are required, despite a reduced attendance to the dental office [14- 19]. The identification of SARS-CoV-2 in saliva suggested the oral cavity as a reservoir from which the virus transmission may occur during coughing, sneezing, talking, and during dental care [20- 25]. Preoperative antimicrobial mouth rinses with chlorhexidine gluconate (CHX), and hydrogen peroxide (H2O2) have been recommended to reduce the number of microorganisms in aerosols and drops during oral procedures [26-28]. Chlorhexidine has excellent plaque inhibitory properties with an immediate antibacterial effect as well as a prolonged bacteriostatic effect on the oral flora [26]. Clinical studies ranging from 3-month up to 2-year duration with CHX-containing mouth rinses have demonstrated significant reductions in plaque and gingivitis. When CHX toothpaste/gel are used in a non-brushing model, it is significantly less effective in plaque inhibition compared to CHX mouthwash [26].
However, in children, elders and particularly in subjects with ID, mouthwashes seem to be difficult to perform because of their impaired motorial capabilities. Then, the use of such antimicrobial solutions with potential toxic excipients may be associated with adverse symptoms.
For this reason, a device that allows the spreading of the active ingredient in an easy, controlled and safe way is necessary. The device analyzed in the present study, combining mechanical and chemical antimicrobial effects, could be considered a handy product helpful in the reduction of the microbial load in the oral cavity. Further, clinical and microbiological studies detected the amount of Candida albicans, Candida species, Enterobacter species, Staphylococcus aureus, Streptococcus viridans before and after DB cleansing [1,26,27].
The procedure proposed by Roncati et al. [10] allows an efficient, handily and reliable oral brush to control the food debris and dental plaque formation, thus, lowering the viral and bacterial load and consequently reducing microbial transmission. For this reason, it could be useful to consider the application of hydrogen peroxide solution either in combination with CHX or alone to improve the effectiveness of the product against the SARS-CoV-2/Covid-19.
About Hydrogen Peroxide, a relatively potent oxidative agent, low concentrations neither damage oral hard or soft tissues nor do they pose a significant risk of adverse long-term effects [28].
Considering the difficulty of the analyzed subjects in opening their mouth widely and then taking clear pictures of posterior teeth, evaluations were limited only to the anterior teeth that are well reachable and less “food retainers” than posterior ones. A further limitation was that athletes were already aware of traditional brushing while they received information and instruction on the use of DB for the first time in the experimental setting. It could be hypothesized that a learning curve may ulteriorly improve the performance of the cleaning procedure in the test group. In addition, the antimicrobial activity of Chlorhexidine should be considered as an important factor strengthening the mechanical action [29]. The possible influence of better assistance in the oral hygiene in those subjects living at home compared with those in institutions was checked and no differences were found in the residential distribution of subjects in test and control groups.
In conclusion, the Digital Brush has been evidenced to be an appropriate tool for both institutionalized and noninstitutionalized special athletes, in removing dental plaque and food debris, similarly to the conventional toothbrush.
Acknowledgement
The Authors thank Micerium S.p.A. (Genoa, Italy) for providing all products for oral hygiene used in the current study.
Conflict of Interest and Source of Funding Statement
The authors declare that they have no conflict of interest. This study was self-funded by the authors and their institution.
References
- Kumar S, Sharma J, Duraiswamy P, Kulkarni S (2009) Determinants for oral hygiene and periodontal status among mentally disabled children and adolescents. Journal of Indian Society of Pedodontics and Preventive Dentistry 27(3): 151-157.
- Dellavia C, Allievi C, Ottolina P, Sforza C (2009) Special care dentistry for people with intellectual disability in dental education: An Italian experience. European Journal of Dental Education 13(4): 218-222.
- Axelsson P, Lindhe J (1981) Effect of controlled oral hygiene procedures on caries and periodontal disease in adults: Results after 6 years. Journal of Clinical Periodontology 8(3): 239-248.
- Checchi L (1997) Plaque removal with variable instrumentation. Journal of Clinical Periodontology 24(10): 715-717.
- Block SS, Beckerman SA, Berman PE (1997) Vision profile of the athletes of the 1995 Special Olympics World Summer Games. Journal of the American Optometric Association 68(11): 699-708.
- Stanish HI, Temple VA, Frey GC (2006) Health-promoting physical activity of adults with mental retardation. Mental Retardation and Developmental Disabilities Research Reviews 12(1): 13-21.
- White JA, Beltran E, Perlman SP (1998) Training manual for standardized oral health screening.
- Fernández Rojas C, Emmanouil D, Dellavia C, Limeres J, Castro N, et al. (2021) Oral health needs of athletes with intellectual disability in Southern Europe: Greece, Italy and Spain. Special Care in Dentistry 41(2): 187-194.
- Rajwani AR, Hawes SND, To A, Quaranta A, Rincon Aguilar JC (2020) Effectiveness of Manual Toothbrushing Techniques on Plaque and Gingivitis: A Systematic Review. Oral Health & Preventive Dentistry 18(1): 843-854.
- Cohen DW, Stoller NH, Chace R, Laster L (1972) A Comparison of Bacterial Plaque Disclosants in Periodontal Disease. Journal of Periodontology 43(6): 333-338.
- Löe H (1967) The Gingival Index, the Plaque Index and the Retention Index Systems. Journal of Periodontology 38(6): 610-616.
- Migliario M, Rimondini L (2011) Food debris index. British Dental Journal 211: 581-521.
- Roncati M, Lucchese A (2013) Journal of Dentistry and Oral Hygiene Plaque removal efficacy of a novel oral care device: A microbiological assessment 5: 83-8.
- Brian Z, Weintraub JA (2020) Oral Health and COVID-19: Increasing the need for prevention and access. Preventing Chronic Disease 17: 200266.
- Sampson V, Kamona N, Sampson A (2020) Could there be a link between oral hygiene and the severity of SARS-CoV-2 infections? British Dental Journal 228: 971-975.
- González-Olmo MJ, Delgado-Ramos B, Ruiz-Guillén A, Romero-Maroto M, Carrillo-Díaz M (2020) Oral hygiene habits and possible transmission of COVID-19 among cohabitants. BMC Oral Health 20:286.
- Carmagnola D, Pellegrini G, Canciani E, Henin D, Perrotta M (2021) Saliva Molecular Testing for SARS-CoV-2 Surveillance in Two Italian Primary Schools. Children (Basel) 8(7): 544.
- Borghi E, Massa V, Carmagnola D, Dellavia C, Parodi C, et al. (2021) Saliva sampling for chasing SARS-CoV-2: A Game-changing strategy. Pharmacol Res 165: 105380.
- Carmagnola D, Henin D, Pellegrini G, Canciani E, Perrotta M, et al. (2021) Diagnostic testing for SARS-CoV-2: state of the art and perspectives of molecular salivary testing. Dental Cadmos 89(4): 264-276.
- Peng X, Xu X, Li Y, Cheng L, Zhou X, et al. (2020) Transmission routes of 2019-nCoV and controls in dental practice. International Journal of Oral Science 12: 9.
- Li Y, Ren B, Peng X, Hu T, Li J, Gong T, et al. (2020) Saliva is a non-negligible factor in the spread of COVID-19. Molecular Oral Microbiology 35(4): 141-145.
- Baghizadeh Fini M (2020) Oral saliva and CVID-19. Oral Oncology 108: 104821.
- Basso M, Bordini G, Bianchi F, Dian A, Vitelli CA, et al. (2020) Preprocedural mouth rinses and COVID-19 transmission: Narrative literature review and clinical recommendations.
- Vergara-Buenaventura A, Castro-Ruiz C (2020) Use of mouthwashes against COVID-19 in dentistry. British Journal of Oral and Maxillofacial Surgery 58(8): 924-927.
- Kelly N, Nic Íomhair A, McKenna G (2020) Can oral rinses play a role in preventing transmission of Covid 19 infection? Evidence-Based Dentistry 21: 42-43.
- Haffajee AD, Roberts C, Murray L, Veiga N, Martin L, et al. (2009) Effect of herbal, essential oil, and chlorhexidine mouthrinses on the composition of the subgingival microbiota and clinical periodontal parameters. Journal of Clinical Dentistry 20(7): 211-217.
- Socransky SS, Haffajee AD, Cugini MA, Smith C, Kent RL (1998) Microbial complexes in subgingival plaque. Journal of Clinical Periodontology 25(2): 134-144.
- Walsh LJ (2000) Safety issues relating to the use of hydrogen peroxide in dentistry. Australian Dental Journal 45(4): 257-269.
- Burton MJ, Clarkson JE, Goulao B, Glenny AM, McBain AJ, et al. (2020) Antimicrobial mouthwashes (gargling) and nasal sprays administered to patients with suspected or confirmed COVID-19 infection to improve patient outcomes and to protect healthcare workers treating them. The Cochrane Database of Systematic Reviews 9.






























