Determinants of Metabolic Syndrome in the Workplace of the National Electricity Company in Kinshasa, Democratic Republic of Congo
Louise Kikontwe Komanda Kalabo1, Benjamin Longo Mbenza2,3, Serge Kabangu2, Hervé Alex Tukadila Kabangi3 and Aliocha Nkodila Natuhoyila3*
1Department of Physical Medecine, University of Kinshasa, Kinshasa, Democratic Republic of Congo
2Department of Internal Medecine, University of Kinshasa, Kinshasa, Democratic Republic of Congo
3Department of Public Health, Lomo University Reseach, Kinshasa, Democratic Republic of Congo
Submission: September 09, 2020; Published: October 27, 2020
*Corresponding author: Aliocha Nkodila Natuhoyila, Department of Public Health, Lomo University Reseach, Kinshasa, Democratic Republic of Congo
How to cite this article: Louise K K K, Benjamin L M, Serge K, Hervé A T K, Aliocha N N. Determinants of Metabolic Syndrome in the Workplace of the National Electricity Company in Kinshasa, Democratic Republic of Congo. Curre Res Diabetes & Obes J 2020; 13(5): 555873. DOI: 10.19080/CRDOJ.2020.13.555873
Abstract
Background: Non-communicable diseases (NCDs) and chronic diseases such as cardiovascular disease (CVD), chronic respiratory conditions, diabetes, cancer, and musculoskeletal disorders are multifactorial and disabling diseases. They have become a real burden globally [1-5]. Indeed, metabolic syndrome is a warning sign of a serious health problem in the workplace. It witnesses the significantly increased risk of developing type 2 diabetes and/or cardiovascular disease-causing disability, reduced production, and premature death.
Aims: To identify the factors associated with the metabolic syndrome in SNEL workers in the city of Kinshasa.
Methods: longitudinal study for analytical purposes carried out among agents of an electricity company in the city of Kinshasa. The data collection was based on a questionnaire, a clinical examination, and a laboratory assessment.
Results: 92 agents responded to the summons, or 65.5%. The risk factors associated with metabolic syndrome in SNEL employees before the procedure are: sex (OR=9.9), marital status (OR=0.24), function, tobacco consumption (OR=1.23). , history of arterial hypertension (HBP) (OR=1.29), history of CVD (OR=0.59) and history of type 2 diabetes (T2D), (OR=0.01), healthy diet (OR=26.5), quality of life (OR=1.3) and recreational physical activity (APL) (OR=1.28). After the intervention, it emerges from the same table that the RF associated with the metabolic syndrome in SNEL employees are: age (OR=0.48), level of study (OR=3.09), function (OR=3.09), sedentary lifestyle (OR=0.445), tobacco (OR=0.21), alcohol (OR=0.20), history of hypertension (OR=0.33) , history of CVD (OR=0.26), Quality of life (OR= 9.87),healthy diet (OR=1.9). and APL (OR=1.7).
Conclusion: This study made it possible to objectify the extent of the metabolic syndrome and the associated RFs. He witnesses the significantly increased risk of developing NCDs in sedentary workers with an impaired quality of life. These results call for the urgent implementation of targeted preventive and therapeutic strategies for the metabolic syndrome in order to combat the emergence of chronic and non-communicable diseases.
Keywords: Metabolic syndrome; Associated factors; Kinshasa
Introduction
According to projections, in 2030 CVD will be responsible for more than 23.6 million deaths worldwide [7]. In developing countries, they will be responsible for more deaths than the sum of infectious, nutritional, maternal and perinatal diseases [8]. In addition, CVD is the leading cause of death in diabetics. The progression of these insidiously progressive diseases is associated with the prevalence of obesity, which has almost doubled in adults over the past 30 years [9]. They are the result of interactions between a set of well-known non-modifiable (sex, age, ethnicity) and modifiable risk factors (RF) including physical inactivity (PI), smoking, excessive alcohol consumption and poor diet (low intake of vegetables and fruits) [10-13] in a context of urbanization, rapid industrialization and health transition (epidemiological, demographic, nutritional). Indeed, changes in the global food system have led developing countries (DCs) into a nutritional transition characterized by a diet that is westernized and an increasingly sedentary lifestyle, factors that all contribute to modulating the prevalence. obesity and its metabolic and cardiovascular consequences (hyperglycemia, hypercholesterolemia, arterial hypertension, visceral obesity), in populations and in individuals [6,14-17].
The constellation of three or four of these risk factors in an individual are well identified and constitute a pathological entity called metabolic syndrome (Smet) which is currently a public health problem in the world. Globally available data indicate that 20% to 30% of the adult population has metabolic syndrome [6]. The prevalence of Smet and its manifestations varies from 10 to 30% in industrialized countries depending on the definition used to determine it, the age of the group studied, the sex and the ethnicity of the participants in the different studies [5,18-19]. In the United States, it affects about a fifth of the adult population and in Europe almost a quarter. This is an evolving phenomenon, the number of patients with Smet in the world was 150 million in 2000 and, in the absence of essential primary prevention measures, it will reach 235 million in 2025. WHO says “most” Africans are prone to at least one of the major risk factors for NCDs?
Several studies report very high and increasing rates of these factors of MCR, Smet, obesity, diabetes mellitus and CVD in the workplace in SSA [18,20-26]. NCDs in general and CVD are growing rapidly in low- and middle-income countries, as there is no integrated primary health care program for the detection of metabolic syndrome and treatment of individuals at risk unlike to PD. The DR Congo is not spared by this global epidemic, it responds to practically the same changes in living conditions observed in the world. However, there is little work on this association in the population of DR Congo in general and in the workplace. NCDs are already established as a public health problem in the Democratic Republic of Congo (DRC), both in hospitals [27-30], in the population [31,32] and in the workplace [33-34].
Indeed, all the epidemiological studies on the Congolese population in these different environments have described a population in nutritional, demographic and epidemiological transition, and characterized by a high risk of developing chronic non-communicable diseases in general and CVD in particular. Studies carried out at the National Electricity Company (SNEL) indeed note a predominantly inactive and sedentary working population with a low quality of life (QOL). In an earlier SNEL population study, NKOY observed a very high rate of physical inactivity estimated at 61.9% and a rate of 72.9% of stressed employees [35]. In addition, in the same study, a positive association between the rate of stressed employees and the category with high socioeconomic level was highlighted. ONYUMBE [36] noted an estimated mortality rate of 35.3% for all departures during the period from 1990 to 2003 within SNEL.
There is a high concentration of two-thirds of the active agents of SNEL in the age group between 40 years and 54 years, raising a population in advancing age and at risk of developing CVD. During daily work in the SNEL rehabilitation service, between 2003 and 2007, the KIKONTWE team (candidate for this thesis) noted that the number of cases of diabetic neuropathy, morbid obesity, musculoskeletal disorders -skeletal, physical deconditioning, high blood pressure and that of employees suffering from cerebrovascular accident (CVA) respectively increased from year to year and the cases of premature death became more and more frequent. These supposedly considerable clinical consequences of MCR in the SNEL workplace, especially in terms of SMET, are not yet attributable to BP, healthy diet, and quality of life.
Method
The study is longitudinal for analytical purposes, we followed up on the employees of the National Electricity Company in the city of Kinshasa province, managers and non-managers combined being on the list of staff as provided by the Human Resources Department. For three years, during the period from 06 November 2007 to 10 October 2010. In addition, the sampling for this study is accidental non-probability. The agents were selected according to the order of their arrival at the offices of Occupational Medicine or at the SNEL Polyclinic located on Avenue de la Justice in the commune of Gombe. Therefore, a sample of 92 agents was selected based on the inclusion criteria (Table 1).
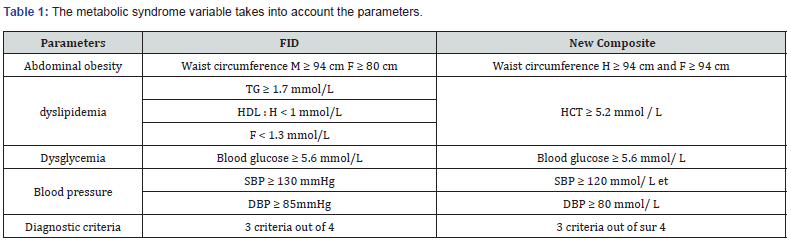
In addition, a pre-established and pre-coded data collection sheet as well as validated and adapted questionnaires were used for the annotation of the parameters of interest collected according to techniques, tests, and standardized scores. In addition, with regard to the variables, the dependent variable is the metabolic syndrome, which is a dependent variable built on the basis of the approach to the definition of FID modified by the author of the present thesis by considering at least three criteria to diagnose metabolic syndrome. The metabolic syndrome variable considers the parameters: for abdominal obesity: waist circumference according to local thresholds; for high total cholesterol, dysglycemia, and high blood pressure (SBP and DBP) according to WHO [37]. Thus, we will have two modalities namely:
a. Yes: presence of metabolic syndrome
b. No: No metabolic syndrome
The independent variables are grouped into two categories, the non-modifiable and the modifiable. Non-modifiable independent variables (sex, age, family history of hypertension, T2DM and CVD) and modifiable variables These are the anthropometric measurements of the SNEL employee collected at the time of the survey, at the start and in end of intervention for the two interventions, in particular: anthropometric, clinical and biological data, as well as the composite variable on quality of life, healthy diet and physical leisure activity.
The intervention consisted of health promotion in terms of moderate free physical activity and healthy eating supported by therapeutic education of the patient in primary prevention, over a period of three years. The recommended healthy diet was a diet rich in fruits and vegetables, fish, and white meat, low in fat, various cold cuts, salt and red meat. As for BP, it was recommended that they reduce the time of sedentary behaviors, increase the volume of BP, especially APL, reduce alcohol consumption and stop smoking. Finally, personalized advice was provided for the management of quality of life.
After data entry using EPI DATA 3.0 software, the data was and analyzed using SPSS 25.0 software. Indeed, within the framework of this study we used two statistical analyzes of the data: univariate and multivariable analyzes. As for the univariate analysis, the qualitative variables are grouped together in the form of tables of frequencies and for the quantitative variables data are summarized as the mean with standard deviation when the distribution is symmetric or otherwise by the median. and its interquartile space. For multivariate analysis, the binary logistic relationship is used to determine the risk factors for Metabolic Syndrome. In short, all the analyzes for the modifiable variables were carried out in two phases, before the intervention and after the intervention.
Results
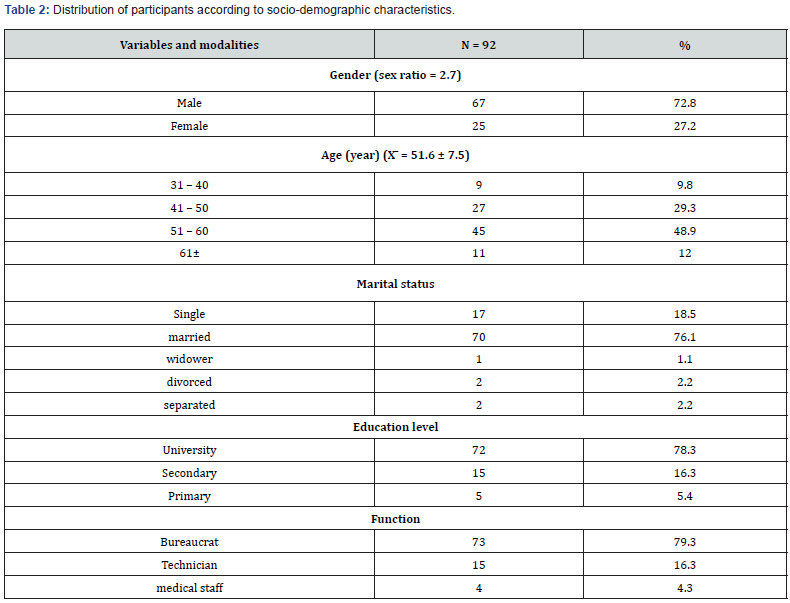
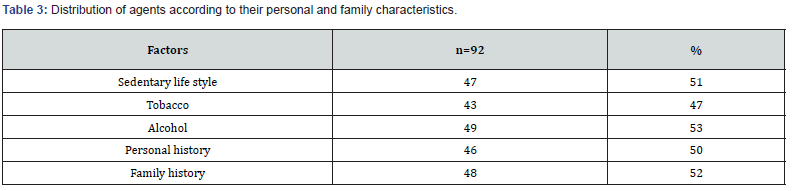
For the univariate analysis, based on the selected sample, table 2 shows that with regard to gender, 72.8% of employees are men; for age, the mean age is 51.6 years with a standard deviation of 7.5 years. Regarding marital status, 76.1% of employees have married marital status, 78.3% have university level. In the end, for the function, 79.3% of SNEL employees are bureaucrats. Table 3 shows that 51% of agents are sedentary, 47% who consume tobacco, 53% consume alcohol, 50% had a personal history of hypertension, T2D or CVD and 52% had a family history of hypertension, T2DM or CVD. Table 4 shows before the intervention, there were 22% of the agents who had good quality of life and there is a strong improvement of 51% after the intervention.
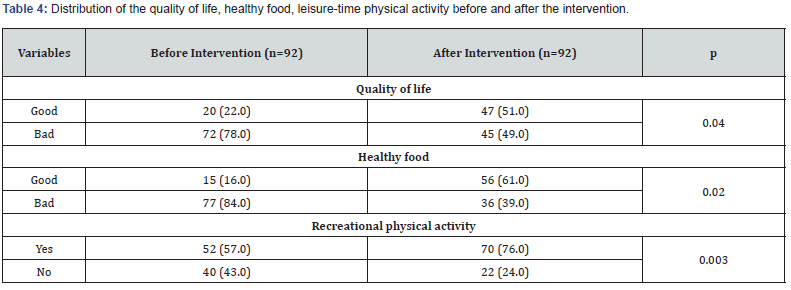
In addition, there is a statistically significant relationship between the quality of life before and after the intervention at the 5% level. Before the intervention, there were 16% of the workers who had the right healthy diet and there is a strong improvement of 61% after the intervention. In addition, there is a statistically significant relationship between healthy eating before and after the intervention at the 5% level. Before the intervention, there were 57% of the agents who engaged in recreational physical activity and there is a strong improvement of 76% after the intervention. In addition, there is a statistically significant relationship between the APL before and after the intervention at the 5% level.
For the multivariate analysis, before the intervention, it emerges from Table 5 that the factors associated with the metabolic syndrome in SNEL employees are: sex, marital status, function, tobacco consumption, personal history and family hypertension, CVD and T2DM, healthy diet, quality of life and physical activity for leisure. Indeed, about sex, there is an equal chance that male agents have the metabolic syndrome compared to female agents (p=0.000, OR=1.28). Regarding marital status, agents who live outside a union are 10 times more likely to develop the metabolic syndrome compared to those who are in a union (p=0.002, OR=9.9). For function, there is 76% less chance than SNEL employees who are non-bureaucrats to have the metabolic syndrome compared to bureaucratic employees (p=0.003, OR=0.24).
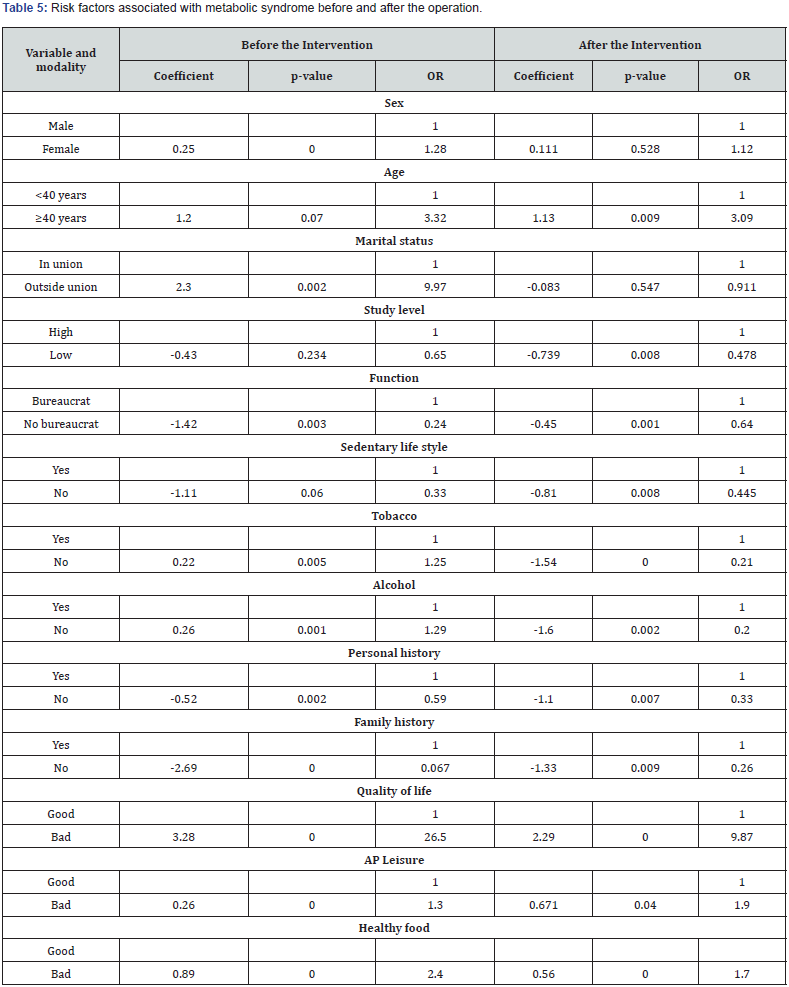
Compared to tobacco, there is almost equal chance of nonsmoking employees to have metabolic syndrome compared to smokers (p=0.005, OR=1.23). Also, for alcohol consumption, there is also almost equal chance of employees who consume alcohol to have metabolic syndrome compared to those who do not (p=0.002, OR=1, 29). For a personal history of hypertension, CVD and / or T2DM, there is a 41% lower chance that those without a personal history of hypertension, CVD and T2DM have metabolic syndrome compared to those who have some (p=0.002, OR=0.59). As for a family history of hypertension, CVD and / or T2DM, there is almost 99% less chance for employees who do not have a family history of hypertension, CVD and T2DM developing the metabolic syndrome compared to those who have a family history of hypertension, CVD and / or T2DM (p=0.000, OR=0.01).
In relation to quality of life, there is a 26 times greater chance that employees of SNEL in Kinshasa who have a poor quality of life of developing the metabolic syndrome compared to those who have a good quality of life (p=0.000, OR=26.5). Compared to recreational physical activity, there is almost equal chance that employees who do not practice recreational physical activity develop metabolic syndrome compared to those who do (p=0.000, OR=1.3). Finally, when it comes to healthy eating, employees who have poor diet are twice as likely to have metabolic syndrome compared to those who have a good diet (p=0.000, OR=2.4). After the intervention, it emerges from the same table that the risk factors associated with the metabolic syndrome in SNEL employees are: age, level of education, Functions, sedentary lifestyle, Tobacco, Alcohol, personal and family history of ‘HTA, MCV and / or T2D, Quality of life, food and APL.
Indeed, with regard to age, there is 3 times more chance that agents who are 40 years of age and over to develop the metabolic syndrome compared to those who are less than 40 years (p=0.009, OR=3.09). In terms of education level, there is a 52% lower chance that employees with low education levels will develop metabolic syndrome compared to those with low education (p=0.008, OR=0.48). For function, there is 36% less chance than SNEL employees who are non-bureaucrats to have metabolic syndrome compared to bureaucratic employees (p=0.001, OR=0.64). Compared to a sedentary lifestyle, there is a 55.5% lower chance for employees who are not sedentary to develop metabolic syndrome compared to those who are sedentary (p=0.008, OR=0.445). Compared to tobacco, there is a 79% lower chance of non-smoking employees of having metabolic syndrome compared to smokers (p=0.000 OR=0.21).
Also, for alcohol consumption, employees who do not consume alcohol are 80% less likely to have metabolic syndrome compared to those who consume it (p=0.002, OR=0.20). For a personal history of hypertension, CVD and / or T2DM, there is a 67% lower chance that those without a personal history of hypertension, CVD and / or T2D have metabolic syndrome compared to those which have (p=0.007, OR=0.33). As for a family history of hypertension, CVD and / or T2DM, there is almost less than 76% chance for employees who do not have a family history of hypertension, CVD and / or T2DM developing the metabolic syndrome compared to those with a family history of hypertension, CVD and / or T2DM (p=0.009, OR=0.26).
In relation to the quality of life, there is 10 times more chance that employees of SNEL in Kinshasa who have a poor quality of life to develop the metabolic syndrome compared to those who have the good quality of life (p=0.000, OR=9.87). For recreational physical activity, employees who do not engage in recreational physical activity are twice as likely to develop metabolic syndrome compared to those who do (p=0.000, OR=1, 9). Finally, when it comes to healthy eating, employees who have poor diet are twice as likely to have metabolic syndrome compared to those who have a good diet (p=0.000, OR=1.7).
Discussion
The prevalence of metabolic syndrome depends on the definition used, the year of the study, the ethnicity, the age and the sex of the population, which does not make analyzes between countries and between continents very objective [38-40]. As reported by the literature review, regardless of the definition used, the presence of Smet in a population really shows that MCR, a precursor of CVD and T2DM, is present and this calls for action. The results of the majority of epidemiological studies on MCR carried out in the clinic, in the general population or in the workplace, have reported an African population characterized not only by the presence of Smet, a high risk of developing NCDs, many factors of cardiovascular risk but also the presence of already confirmed diseases, mainly T2DM, CVD or even chronic kidney disease [6,41-43]. It therefore seemed imperative to act sooner and detect this MCR in the SNEL workplace, at the very beginning of its development. Especially since during screening campaigns, both in PDs and DCs, the most alarming is that most people are unaware of their state of health [44]. This situation is a challenge for the health system.
Thus, in the present study, the metabolic syndrome was assessed according to the criteria of the new approach as detailed in the methodology. It considered the same parameters as the FID 2009 (abdominal obesity according to local thresholds, dysglycemia, dyslipidemia and high blood pressure) while having, however, rectified certain criteria, in particular the thresholds for abdominal obesity. (≥ 94 cm for both sexes according to local thresholds specific to DR Congo), high blood pressure or pre-hypertension according to WHO [45] (PAS ≥ 120 mmHg and PAD ≥ 80 mmHg) and dyslipidemia (for a total cholesterol level ≥ 5.2 mmol/ L). It should be noted that the study by Nasila Sungwasha et al has consolidated the choice of the Smet approach as defined in this thesis. Indeed, they concluded in their study that the constellation of non-lipid variables is sufficient to define MCR in black Africans including carbohydrate metabolism,
blood pressure and obesity. They also noted that three factors among dyslipidemia, abdominal hypertension, and obesity, and dysglycemia are identified in the Smet phenotype in African Bantus.
And obviously, the waistlines should be defined according to the thresholds specific to the African Bantu [46] The results of this study reported alarming rates of Smet and FRCV and behavioral RF determining not only the emergence of MCV but also the danger of the early onset of CVD and T2DM and socio-professional and disabling consequences, in particular in terms of quality of life and productivity [47]. Worse, most participants in this study were unaware of their risk profile. The results of this study showed that the rate of Smet was significantly associated with age in the 41-50 age group, however the highest rate was concentrated in the 51-60 age group ( the mean age of this study population was 51.6 ± 7.5 years). These results are consistent with those from the NHANES survey, the D.E.S.I.R study and the MONICA study, which determined that Smet was associated with aging [48,49], and its frequency increased with age. And the WHO has announced an improvement in life expectancy in SSA countries, particularly in the WHO African region where it increased by 9.5 years from 2010 to 2015, or 60 years [47,50].
Apart from the fact that older people are sedentary, this advancement in age increases the risk burden associated with non-communicable and chronic diseases. The study by Ouédraogo et al, carried out on a population in the workplace of Burkina Faso with a sex ratio equal to 2.7 as in the present study, clearly illustrated the association of Smet with age. Although the average age was far lower than that of this study, i.e. 42.07 ± 9.3 years, the highest rate of Smet was the most represented in the 40-60 age group [51]. According to WHO, the prevalence of sedentary lifestyle in SSA varies depending on the country from 6.5% to 51% with a median of 24%. Sedentary lifestyle contributes to the development of metabolic syndrome through obesity. The results of this study reveal a working population with one of the highest sedentary rates in SSA. Studies conducted in other workplaces have also reported high rates of sedentary lifestyle such as those conducted in Morocco [52] and Senegal [53]. Sedentary lifestyle contributes to the development of metabolic syndrome through obesity. Since 2005, lack of physical activity has been recognized as an emerging occupational risk factor by the European Agency for Safety and Health at Work [54].
It is worth remembering that the usual level of physical activity is now recognized as one of the important determinants of health status. The volume of PA recommended by WHO for achieving health impact has evolved into seeking every opportunity to be active in all circumstances of life. In agreement with Goldberg and Zins, who state that recreational PA is a protective factor for cardiovascular risk, this study found that there is twice as much chance that agents who do not engage in physical activity leisure activities of developing metabolic syndrome compared to those who practice it [55]. Few studies have reported the association between Smet and quality of life. Conversely, this study reports that SNEL agents which have a low quality of life have a 10 times greater chance of developing the metabolic syndrome compared to those which have a high quality of life.
Unlike the study by Vetter and Wadden which failed to establish significant relationships between these two parameters [56]. In addition, an Australian study has shown that an employee in poor health has on average 18 days of absence compared to 2 days for an employee in good health (Guide to promoting health and wellness in the workplace, 2012). Many studies have shown that physical activity reduces the rate of sick leave. For example, according to the WHO, physical activity programs in the workplace can reduce sick leave by 6% to 32%, and therefore absenteeism on the employer side [57]. Numerous studies have demonstrated the benefits of physical activity in the workplace on indicators of well-being and quality of life at work: employee morale, self-confidence, job satisfaction, cohesion between teams, stress level [58,59]. In 2015, a first study carried out by Goodwill management with more than 200 companies, carried out by Medef with the French National Olympic and Sports Committee, showed that sports activity improved the quality of life at work.
The benefits for the employer were reduced absenteeism, lower accidents at work and improved performance [60]. Finally, when it comes to healthy eating, agents who have poor diet are twice as likely to have metabolic syndrome compared to those who have a good diet. Trend studies carried out in several countries illustrate unhealthy diet (having lost food quality) [61,62] and its consequences for human health [63,64]. This loss of quality is expressed by the tendency to replace a diversified diet rich in fruits, vegetables, fiber, and whole grains in favor of red meats, cold meats, and ready-to-eat food products [64,65]. According to the most recent data from the Global Burden of Disease, Injuries, and Risk Factor study 2013 (GBD 2013), the risk associated with unhealthy or poor-quality food is the leading cause of death worldwide with 11.3 million deaths. in 2013 ahead of tobacco, alcohol and physical inactivity combined. The greatest risks have been associated with a diet low in vegetables, whole grains, fruits, fiber and high in sodium [66].
Conclusion
The present study described a working population characterized by an epidemic rate of Metabolic Syndrome (46.7%) which was lowered by management based on moderate individual PA and healthy diet and improvement of quality of life. It determined the RF associated with Smet such, age≥40 years, level of university studies, bureaucratic function, sedentary lifestyle, tobacco, excessive alcohol consumption, family history of hypertension and cardiovascular disease. In addition, she also determined protective factors which are good quality of life, healthy diet, and regular and moderate leisure PA. These results call for the urgent implementation of targeted preventive And therapeutic strategies for the metabolic syndrome to combat the emergence of chronic and non-communicable diseases.
Acknowledgment
We thank all who participated in the study.
Author’s Contribution
LKKK and ANN designed and analyzed the statistical data for the study. SK and HATK contributed to the data collection. BLM supervised the study. All authors have read and approved the final and revised version of the manuscript
References
- Organisationmondiale de la Santé (2016) WHO Mortality Database. Genè
- Alleyne G, Binagwaho A, Haines A, Jahan S, Nugent R, Rojhani A, et al. (2013) Embedding non-communicable diseases in the post-2015 development agenda. Lancet 381(9866): 566-574.
- Organisationmondiale de la Santé (2008)Obésité: prévention et priseen charge de l’épidémiemondiale, in Série de Rapports techniques. Genè
- Abegunde DO, Mathers CD, Adam T, Ortegon M, Strong K (2007) The burden and costs of chronic diseases in low-income and middle-income countries. Lancet 370(9603): 1929-1938.
- Nasheeta Peer, AndréKengne, Ayesha Motala, JeanClaude Mbanya (2014) Diabetes in the Africa region: An update.Diabetes Res Clin Pract 103(2): 197-205.
- Wémeau J L (2014) Syndrome mé Endocrinologie, Diabète, Métabolisme, Nutrition pour le Praticienpp 407-410.
- OMS (2016) Rapport mondial sur le diabè Résuméd’orientation.
- Eckel RH, Khan R, Robetson RM, Rizza RA (2006) Preventing cardiovascular disease and diabetes: A call to action from the American Diabetes Association and the American Heart Association. Circulation 113(25): 1206-1252.
- WHO (2011) Physical inactivity a global public health problem.
- Khaw KT, Wareham N, Bingham S, Welch A, Luben R, et al. (2008) Combined impact of health behaviours and mortality in men and women: the EPIC-Norfolk prospective population study. PLoS Med 5(1):e12.
- Dépiesse F, Coste O (2016)Prescription des activités physiques enprévention et enthé Elsevier Masson pp 517.
- Danaei G, Rimm EB, Oza S, Kulkami SC, Murray CJ, et al. (2010) The promise of prevention: the effects of four preventable risk factors on national life expectancy disparities by race and country in the United States. PloS Med7(3): E1000248.
- WHO (2014)Global Status Report on non-communicable diseases 2014. Geneva: WHO Press, World Health Organization pp 298.
- Swinburn BA, Sacks G, Hall KD, Mc Pherson K, Finegood DT, et al. (2011) The global obesity pandemic: shaped by global drivers and local environments. Lancet378(9793):804-814.
- Popkin BM, Adair LS, Ng SW (2012) Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev 70(1):3-21.
- Yusuf S, Reddy S, Ounpu S, Anand S (2001) Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation 104(22):27465.
- Despres JP (2012) Body fat distribution and risk of cardiovascular disease: an update. Circulation126(10):130113.
- Park Y, Zhu S, Palaniappan L, Heshka S, Carnethon MR, et al. (2003) The metabolic syndrome: prevalence and associated risk factor findings in the US population from the third national health and nutrition examination survey. 1988-1994. Arch Intern Med 163: 427-436.
- Cameron, Adrian J, Jonathan E, Shaw, Paul Z Zimmet (2004) The metabolic Syndrome: Prevalence in worldwide Populations. Endocrinol Metab Clin North Am33: 351-375.
- Ervin, Bether R (2009) Prevalence of metabolic syndrome among Adults 20 years of age and over, by sex, age, race and ethnicity and body mass index : united states, 2003-2006. Natl Health Stat Report13:1-7.
- BitaFouda AA, Lemogoum D, Owona J Manga,J II Dissongo, R Tobbit, et al. (2012) Epidémiologie de l’obésitéen milieu du travail à Douala, Cameroun. Rev Med Brux 33: 131-137.
- Koffi NM, Sally SJ, Kouame P, Silue K, Diarra Nama AJ (2001)Faciès de l’hypertensionartérielleen milieu professionnel à Abidjan. Médecined’Afrique Noire 48: 257-260.
- EtoundiNgoa LS, Melaman SF, Belinga A (2006)Obésitéen milieu hôtelier : Influence du poste de travail sur les métabolismeslipidique et glucidique et sur la pression artérielle de 80 employées de sexeféminin des hôtels de Yaoundé au Cameroun. Médecined’Afrique Noire53: 137-141.
- Chatti S, Debbabi F, Ben AA, Harbaoui R, Ghannem H (2010)Facteurs de risquecardiovasculaire chez les travailleurspostésd’une centrale de production d’électricité au centretunisien. Ann CardiolAngeiol (Paris) 59: 190-195.
- Gombeth TH, Kimbally KG, Ikama MS, Ellenga MB (2007) Hypertension artérielle et les autresfacteurs de risquecardiovasculairesen milieu professionnelBrazzavillois. Médecined’Afrique Noire 54: 545-548.
- Boursier V (2006) Le Syndrome Mé Journal des Maladies Vasculaires31: 190-201.
- Organisationmondiale de la Santé (2003) Diet, Nutrition and the Prevention of Chronic Diseases. Report of a Joint WHO/FAO Expert Consultation, OMS, série de rapports techniques no 916. Genève, Organisationmondiale de la Santé.
- Ng SW, Popkin BM (2012) Time use and physical activity: a shift away from movement across the globe. Obes Rev13:659-680.
- Rezende LF, Sa TH, Mielke GI, Viscondi JY, Rey Lopez JP, et al. (2016) All-Cause Mortality Attributable to Sitting Time: Analysis of 54 Countries Worldwide. Am J Prev Med 51:253-263.
- Patel AV, Bernstein L, Deka A, Heather Spencer Feigelson, Peter T Campbell, et al. (2010) Leisure time spent sitting in relation to total mortality in a prospective cohort of US adults. Am J Epidemiol172:419-429.
- Chatterjee A, Stewart B Harris, Lawrence A Leiter,David H Fitchett, Hwee Teoh, et al. (2012) Priseen charge des risquescardiométaboliquesensoinsprimaires : Résumé de la déclarationconsensuelle de 2011. Can Fam Physician58(4): e196–e201.
- OrganisationMondiale de la Santé (2002) Rapport sur la santé dans le monde. Réduire les risques et promouvoirune vie saine. Genè
- Agence de santépublique du Canada (2006)Stratégie de développement durable 2007-2010; Démarche de développement durable dans la santé Ottawa.
- Promouvoir la santé et prévenir maladies et accidents. Argumentaire. Promotion Santé Suisse, Lausanne et Berne. Juin 2010.
- Fédération internationale du diabète, « Rapport annuel », Bruxelles, 2014.
- Church TS, Thomas DM, TudorLocke C, Peter T Katzmarzyk, Conrad P Earnest, et al. (2011) Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLoS One 6: e19657.
- WHO EMRO Maîtrisezvotre tension artérielle, maîtrisezvotrevie.
- DECODE study Group, Qiao Q (2006) comparison of different definitions of the métabolic syndrome in relation to cardiovascular mortality in European men and women. Diabetologica 49: 2837-2846.
- Mithun D, Susil P, Arnab G (2010) Factor analysis of risk variables associated with metabolic syndrome in adult Asian Indians. J Cardiovasc. Dis Res 91: 86-91.
- Eckel RH, Grundy SM,Zimmet PZ (2005) The metabolic syndrome. Lancet 365: 1415-1428.
- M’BuyambaKabangu JR, Biswika RT, Thijs L, Tshimanga GM, Ngalula MF, et al. (2009) In-hospital mortality among Black patients admitted for hypertension-related disorders in Mbuji Mayi, Congo. Am J Hypertens22:643-648.
- M’BuyambaKabangu JR, Longo Mbenza B, Tambwe MJ, Dikassa LN, Mbala Mukendi M (1995) J-Shaped relationship between mortality and admission blood pressure in black patients with acute stroke. J Hypertens13: 1863-1868.
- Katchunga B, Katenga M, Kayembe NJM (2007) Morbi-mortalité des accidents vasculairescérébraux dans les unités de soinsintensifs de la ville de Kinshasa. Congo Medical4:995-999.
- Vernay M, Salanave B, De Peretti C, Druet C, Malon A, et al. (2013) Metabolic syndrome and socioeconomic status in France : the French Nutrition and Health Survey (ENNS, 2006-2007). Int J Public Health 58(6): 855-864.
- LongoMbenza, KasiamLasiOn’Kin JB, NgeOkwe A,KongoloKabangu N (2011) The metabolic syndrome in a congolese population and its implications for metabolicc syndrome definitions. Diabetes MetabSyndr 5: 17-24.
- NasilaSungwacha J, Tyler J, LongoMbenza B, KasiamLasi On Ki JB, Gombet T, et al. (2013) Assessing clustering metabolic syndrome components available at primary care for Bantus Africans using factor analysis in the general population. BMC Res Notes 6:228.
- Longo MbenzaB, Tonduangu, Muyeno, Phanzu, A Kebolo Baku, D Muvova, et al. (2000) Predictors of stroke associated mortality in Africans.Rev Epidem et Santépublique48:31-39.
- B Balkau (1996) An epidemiologic survey from network of french Health Examination Centres.D.E.S.I.R: Epidemologic Data on the Insulin Resistance Syndrome. Rev Epidemiol SantePublique 44(4):373-375.
- Balkau B, Vernay M, Mhamdi L, et al. (2002) The frequency and incidence of the NCP (National Cholesterol Education Progam) metabolic syndrome in the french D.E.S.I.R study. Diabetologia 45(2):A15.
- Tabutin D, Masquelier B (2017) Tendances et inégalités de mortalité de 1990 à 2015 dans les pays à revenufaible et intermé Population 72: 227-307.
- Ouedraogo SM, Tougouma JB, Sanon/Lompo S, Yemeogo TM, S Maiga, et al. (2016) Syndrome Metabolique et risquecardiometaboliqueen milieu professionnel. RAFMI (1): 47-55.
- HouhouatAhoungbre ML, Yoyo SE, AkeEdjema A, HFYapi, H Ahibo, et al. (2008) Le Syndrome Métaboliqueexiste-il en Côte d’Ivoire ? Immuno-analyse et biologiespécialisée23:375-378.
- Seck SM, Gueye S, Tamba K.Issa Ba(2013) Prevalence of chronic cardiovascular and metabolic diseases inSenegalese workers : a cross- sectionnal study 2010. Prev Chronic Dis 10: 110339.
- AgenceEuropéenne pour la Santé et la Sécurité au Travail 2005.Prévisions des experts sur les risques physiques émergentsliés à la sécurité et à la santé au travail. Facts 60, 2005.
- Goldberg M, Zins M(2017) Le travail stressant et le cœur ne font pas bon mé Stressful work and heart do not get along well. Med Sci (Paris) 33 :991-996.
- Vetter ML T AWadden, J Lavenberg, R H Moore, S Volger, et al. (2010) Relation of health- related quality of life to metabolic syndrome, obesity, depression and comorbid illness. Int J Obes35(8):1087-1094.
- OMS (2008)La prévention des maladies non transmissibles parl’alimentation et l’activité physique sur le lieu de travail. FEM.
- Entreprise(2013) Nutrition: Améliorer la santé des salaries par l’alimentation et l’activitéMinistère chargé de la santé.
- O’Donnell MP (2000) How to design workplace health promotion programs. Keego Harbor: American Journal of Health Promotion.
- Goodwill management (2015) Etude de l’impactéconomique de l’Activité Physique et Sportive (APS) surl’entreprise, le salarié et la société
- Monteiro C A, Levy RB, Claro R M, de Castro I R R, Cannon G (2011) Increasing consumption of ultra-processed foods and likely impact on human health: evidence from Brazil. Public Health Nutr 14: 5-13.
- Wang D D, Cindy W Leung, Yanping Li, Eric L Ding, Stephanie E Chiuve, et al. (2014) Trends in dietary quality among adults in the United States, 1999 through 2010. JAMA Intern Med 174: 1587-1595.
- Joshipura KJ,Alberto Ascherio, JoAnn E Manson (1999) Fruit and vegetable intake in relation to risk of ischemic stroke. JAMA 282(13) :1233‑1239.
- Tavares L F, Fonseca S C, Garcia Rosa M L, Yokoo E M (2012) Relationship between ultra-processed foods and metabolic syndrome in adolescents from a Brazilian Family Doctor Program. Public Health Nutr 15: 82–87.
- Canella D S, Renata Bertazzi Levy, Ana Paula Bortoletto Martins, Rafael Moreira Claro, JeanClaude Moubarac (2014) Ultra-processed food products and obesity in Brazilian households (2008-2009). PLoS One 9: e92752.
- Poti J M, Mendez M A, Ng S W, Popkin B M (2015) Is the degree of food processing and convenience linked with the nutritional quality of foods purchased by US households? Am J Clin Nutr 101: 1251-1262.






























