Identification of Risk Factors for Obesity Retinopathy among Bangladeshi Adults
KC Bhuyan*
Department of Statistics, Jahangirnagar University, Bangladesh
Submission: September 25, 2020; Published: October 12, 2020
*Corresponding author: KC Bhuyan, Department of Statistics, Jahangirnagar University, Dhaka, Bangladesh
KC Bhuyan. Identification of Risk Factors for Obesity Retinopathy among Bangladeshi Adults. Curre Res Diabetes & Obes J 2020; 13(5): 555872. DOI:10.19080/CRDOJ.2020.13.555872
Abstract
The paper dealt with identification of socioeconomic variables responsible for simultaneous prevalence of obesity retinopathy among Bangladeshi adults. Accordingly, the information provided here were the analytical results of data collected from 995 adults of 18 years and above residing in both urban and rural localities. The adults were classified into two groups. In one group there were 7.5% obese-retinopathy patients. They were classified by different levels of socioeconomic variables and association any of the variable with prevalence of obesity- retinopathy was investigated. It was observed that the prevalence of obesity-retinopathy was significantly associated with age, blood pressure and duration of diabetes. The percentages of affected adults of ages less than 25 years, optimal blood pressure and those who were suffering from diabetes for 20 years and above were 11.7, 10.2 and 22.2, respectively. The most responsible variable in discriminating obese-retinopathy adults form others was blood pressure followed by age, gender, prevalence of diabetes and duration of diabetes. These were identified by discriminant analysis.
Keywords: Obesity; Retinopathy; Discriminant analysis; Correlation coefficient of variable and discriminant function score; Odds ratio; Confidence interval of odds ratio
Introduction
The prevalence of overweight and obesity are in increasing trend over the last decades in both developed and developing countries [1-4]. In 2011 WHO estimated that globally approximately 1.5 billion adults (age > 20 years) were overweight and more than 500 million adults were obese [5]. Obesity is generally associated with risk of arterial hypertension, diabetes, cardiovascular disease (CVD), cancer and renal failure and CVD risk factors play an important role for prevalence of retinopathy [4,6-13]. In other studies it was observed that retinopathy was positively associated with elevated blood pressure, body mass index, cholesterol and triglyceride [14-17].
One of the deadliest disease in the eye is retinopathy and it occurs due to prolonged diabetes and uncontrolled blood glucose [14-16]. Retinopathy was also observed among older people without diabetes [17]. It happens when high blood sugar levels damage blood vessels in the retina and it starts due to uncontrolled blood sugar and delayed treatment of diabetes and it is the second largest non-communicable disease among human beings [ 18-19 ]. The disease is the leading cause of blindness and visual impairment affecting 30 – 40 percent of diabetic patients of age 40 years and above [20-23]. The number of people with blindness due to prevalence of diabetes and retinopathy and low vision were estimated 400000 and 2.6 million, respectively, both almost double since 1990 which indicates that the risk of visual impairment is in increasing trend. For this reason, World Health Organization considers the epidemic a worldwide problem which requires public health intervention that act on different factors associated with overweight and obesity so that congenial atmosphere prevails in the society for maintaining healthy life by the people so that non-communicable diseases can be avoided [24].
But people are less aware, specially the rural people, of the problem of obesity and the consequences of it. Even government and public health planners remain largely unaware of the current prevalence of obesity which is the cause of many diseases like diabetes, CVD, retinopathy, neuropathy, etc. [21]. For these diseases there were well described risk factors. The most and clearly recognized factors are duration of diabetes, the degree of glycaemic control measured as glycosylated haemoglobin. In addition to that, hypertension, dyslipidaemia, smoking, age, body mass index (BMI), were also identified as risk factors of retinopathy [14-17]. Besides these factors some biological factors were also identified as the risk factors of retinopathy [14,22-33].
In this paper, attempt was made to identify some socioeconomic variables responsible for obesity-retinopathy among Bangladeshi adults.
Methodology
To fulfil the objective of the study the data were recorded from adults by quota sampling plan to cover males and females in the ratio 50.1: 49.9 as this ratio is prevailed in the national level of population [34]. Total investigated adults was 995, out of which 498 were males and 497 were females. The investigated respondents were of ages 18 years and above and they were the residents of both urban and rural areas.
The data were collected during the session 2018-19 by some nurses with the help of medical assistants working in some diagnostic centres located in urban and semi-urban areas in Bangladesh. These centers were selected purposively. The data were recorded through a pre-designed and pre-tested questionnaire which contains different questions on demographic characteristics like residence, religion, gender, marital status, age, education, occupation, family income, etc. Beside these, other variables were on their lifestyle and prevalence of any of the noncommunicable diseases, duration of the diabetes, and the stages of treatment of the disease. Some of the variables were qualitative in nature, but all the variables were noted in nominal scale for ease of analysis. The data of weight ( in kg ) divided by height ( in metre2) was used to measure the value of body mass index (BMI) to identify obese adults( if BMI ≥ 27.5; underweight ,if BMI< 18.5; normal, if 18.5 ≤BMI< 23.0; overweight, if 23.0 < BMI< 27.5 ) [35,36]. They were also divided into 4 groups according to their blood pressure (B.P) level ( mmHg). The 4 groups were identified as optimal (if BP < 120/80), normal (if BP <130/85 ), high normal ( if BP < 140/90) and hypertensive ( if BP ≥ 140/90 )[37].
According to the objective of the study, the association of each of socioeconomic variable with simultaneous prevalence of obesity retinopathy was investigated, where significant association was decided if p-value of any Chi-square statistic was less than or equal to 0.05. Irrespective of significant or insignificant association, the odds ratio was calculated for adults for whom prevalence of obesity-retinopathy was noted in higher rate for a particular level of a socioeconomic variable. Finally, discriminant analysis was done to discriminate the adults suffering from obesity retinopathy from other adults. In discriminating the respondents the identification of some variables were done which were responsible for this discrimination. The responsible variables were identified by the higher absolute values of correlation coefficients with discriminant function score and variable values [38-40]. All the calculations were done using SPSS Version 25.
Results
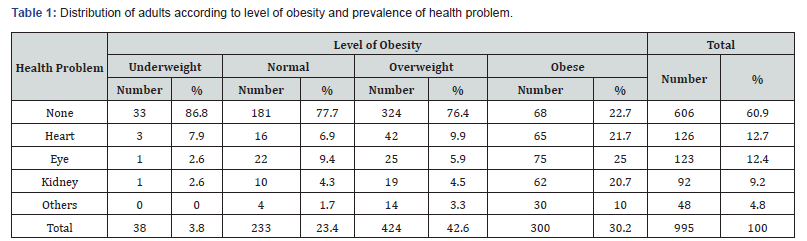
The number of investigated adults was 995, out of which 30.2% were obese, 12.4% were suffering from eye problem. Among obese adults 25% had eye problem. The percentage of adults of eye problem was in increasing trend when the level of body mass index exceeded normal level. Health problem was significantly associated with level of obesity as was observed by Chi-square test [x2 = 275.875, p –value= 0.000, Table 1]. It was seen that prevalence of obesity-eye problem was observed among 75 (6.5%) respondents and the remaining 920 (93.5%) were free of these two health problem simultaneously. The respondents were classified according to prevalence of obesityretinopathy and levels of socioeconomic variables and the risk of the problem for a particular level of socioeconomic characteristic was calculated. In the sample, there were 46.6% urban adults. The prevalence of obesity retinopathy was observed among 7.8% of them. But prevalence rates were similar for both urban and rural residents [ χ 2 =0.061, p –value = 0.805]. Both the groups were similarly exposed to this health hazard. [ O.R.= 1.06 CI{ 0.662,1.697}]. The percentage of female respondents was 49.9 and 8.5% of them were faced the problem of obesity retinopathy. However, the percentages of male and female suffers were not significantly different [χ 2= 1.188, p –value= 0.276]. But females were 30% more exposed to this health problem [ O.R.=1.30, C.I{0.801, 2.089}]. More Muslim adults ( 85.2% ) were included in the sample and 7.7% of them were affected by the disease though Muslim and non-Muslim respondents were not significantly different in respect of rates of prevalence of obesity retinopathy [χ 2 =0.134,p value= 0.715 ]. The Muslim respondents were only 14% more exposed to this health hazard compared to non- Muslim adults [ O.R.= 1.14, C.I {0.572, 2.730}]. The percentage of currently married adults was 93.1 and 7.7% of them were affected by the disease. These group was 85% more exposed to obesity retinopathy [O.R.=1.85, C.I. {0.567, 6.032}]. But the rates of prevalence of the problem among married and single adults were statistically similar [χ 2 =1.082, p-value=0.298]. The percentage (19.7%) of younger adults (< 25 years) was second in higher but maximum number (11.7%) of them were suffering from the problem of obesity retinopathy. This affected group was significantly higher compared to the affected groups of other older respondents [χ 2 = 13.032, p –value = 0.011]. The younger adults were 91% more exposed to this health problem [ O.R.=1.91, C.I{1.138,3.204}]. With the increase in level of education there was almost significantly increase in the prevalence of obesity retinopathy [χ 2 =7.333, p-value=o.062]. Maximum affected group (10.1%) was noted among secondary level educated adults (23.8%). For them the chance to be affected was 2.80 times as it was in other educated adults [ O.R.=2.80, C.I. {1.196, 5.682}}. The percentage of service persons was 30.7 and 8.9% of them were facing the problem of obesity retinopathy. In the sample, 12.3% were retired persons and 8.2% of them were suffering from this health hazard. These two groups were 32% more exposed to this problem compared to other professionals [ O.R.= 1.32, C.I. {0.825, 2.113}]. However, the prevalence rates of the disease for different occupational groups were not significantly different [ χ 2 =4.120, p –value= 0.390]. Housewives were 23.1% and 8.7% of them were suffering from this health hazard. Their risk of the problem was 1.21 times as it was in others [ R.R.=1.21].
The family income of 6.1% adults were Taka 100 thousand to less than 150 thousand. Among these adults 11.5% were affected by obesity retinopathy. These adults were 65% more exposed to the problem compared to adults belonged to families of other income levels [O.R.=1.65, C.I. {0.723,3.766}]. There was no significant increasing trend in the rate of affected persons with the increase in level of family income [ χ 2=4.050, p –value=0.256]. Similar was the case with family expenditure (Table 2). It was also observed that there was an increasing trend in the rate of this health problem with the increase in level of family to expenditure up to expenditure up to Taka less than 80 thousand. Highest affected group (11.2%) was noted among adults of families spending Taka 60 thousand but less than taka 80 thousand (14.4%). This group was 69% more exposed to this health problem compared to others[ O.R.=1.69, C.I.{ 0.944, 3.025}; χ 2 =3.927,p-value= 0.269 [ Among the adults 36.5% were habituated in taking process food and 8.0% of them were affected by the problem. This group was 11% more exposed to obesity eye problem compared to the adults who were not habituated in taking process food. [O.R.=1.11,C.I.{ 0.655, 1.727}]. However, insignificant variation in the rates of prevalence of the problem was noted due to variation in the habit of taking process food [ χ 2=0.167,p-value=0.632}]. Among the respondents 66.9% were non-smokers and 7.8% of them were affected by the disease. They were 13% more exposed to the problem compared to smokers [O.R.=1.13].
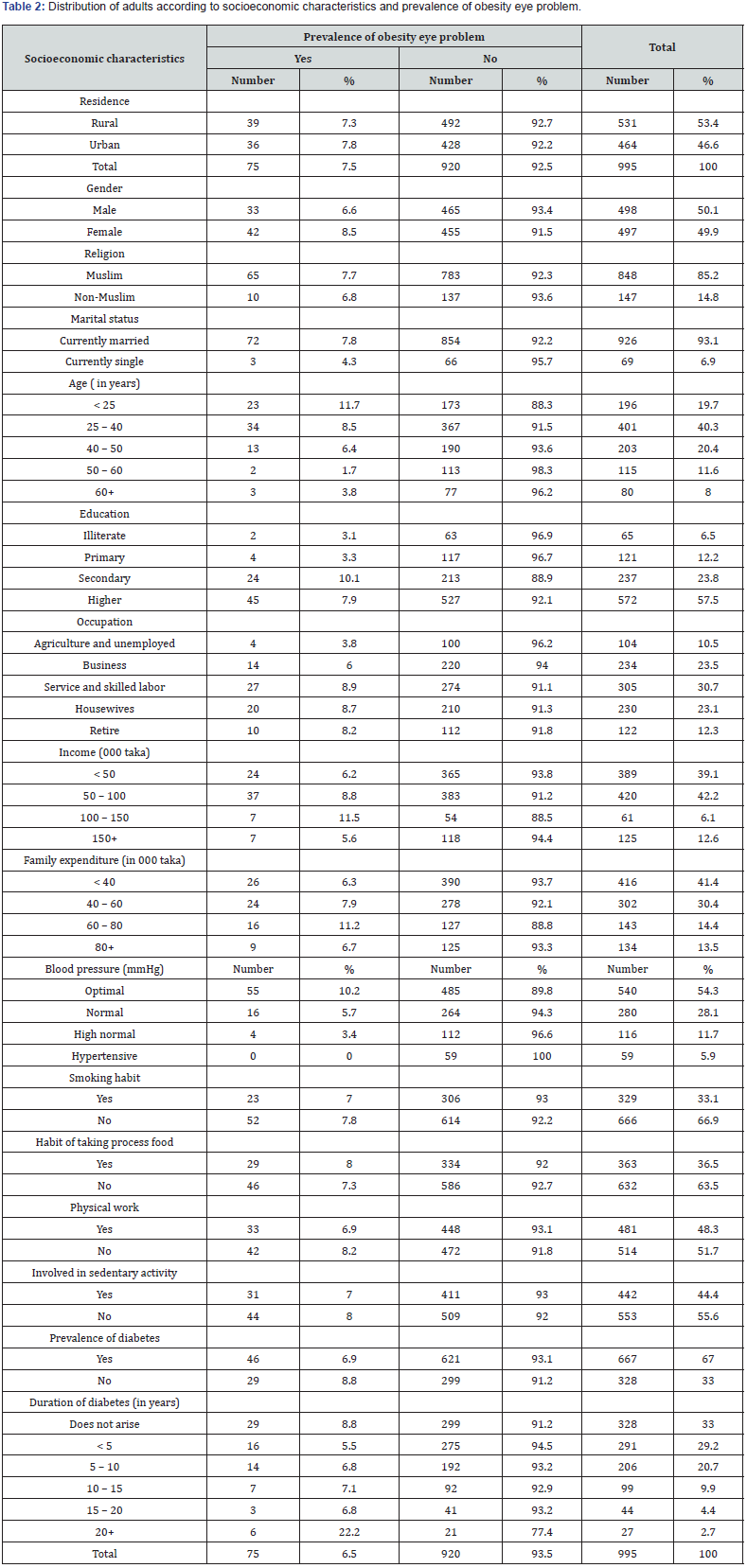
But smoking habit and prevalence of obesity retinopathy was not significantly associated [χ 2 =0.211, p-value=0.646]. The percentage of adults not involved in sedentary activity was 55.6 and 8.0% of them were facing the problem of this health problem. They were 15% more exposed to this problem compared to other group [ O.R.=1.15, C.I. {0.649,1.687}]. But sedentary activity was not significantly associated with prevalence of obesity retinopathy [ χ 2=0.313, p –value=0.576]. The percentage of adults not doing any physical labor was 51.7 and 8.2% of them were affected by the disease. They were 11% more exposed to the problem compared to adults doing physical labor [ O.R.=1.11, C.I. {0.622,1.784]]. Physical labor and prevalence of obesity retinopathy was not significantly associated [χ 2 =0.612, p value= 0.434].
There were 33.0% non-diabetic adults and 8.8% of them were the patients of obesity eye problem. This group was 31% more exposed to this health problem. [O.R.=1.31, C.I. {0.807,2.126}]. But prevalence of diabetes and prevalence of obesity retinopathy was not significantly associated [χ 2=1.113, p value = 0.276]. Duration of diabetes was a risk factor for prevalence of obesity retinopathy [χ 2=11.117, p value=0.049}. Only 2.7% adults were suffering for 20 years and more and they were exposed by more than 2.72 times to this health hazard [ O.R.=3.72, C.L {1.455, 5.892}]. The percentage of adults of optimal blood pressure was 54.3 and 10.2% of them were suffering from obesity eye problem. This group was highly exposed to this health hazard [ O.R.=2.47, C.I. {1.458, 4.185}]. There was significantly decreasing trend in the rate of prevalence of the problem with the increase in level of blood pressure [ χ 2 =14.360, p – value = 0.002].
Discriminant Analysis
This analysis was done to identify the most responsible factor for the prevalence of obesity retinopathy in discriminating the obese-retinopathy adults from others (Table 3). The variables included in the analysis were residence, religion, gender, marital status, age, education, occupation, family income, family expenditure, smoking habit, habit of taking process food, physical labor, prevalence of diabetes, duration of diabetes and blood pressure. These variables significantly discriminated the two groups of adults [Λ = 0.945, χ 2=55.443, p-value=0.000].
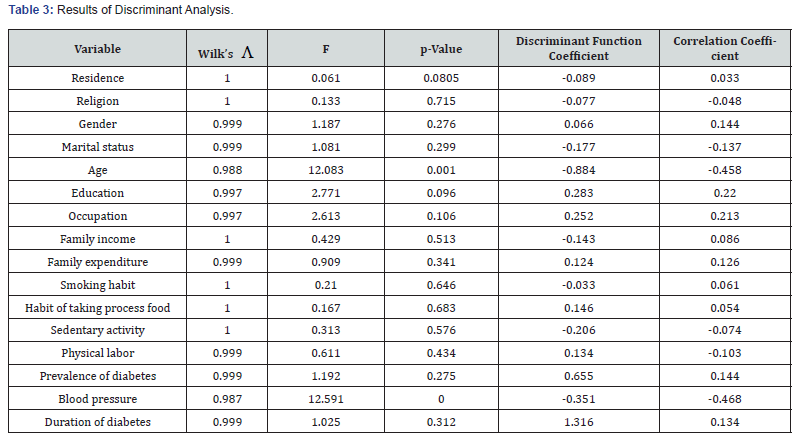
The most important variable for discrimination was blood pressure followed by age, education and occupation.
Discussion
Obesity is the predominant risk factor of retinopathy and CVD [13]. The risk of prevalence is developing after longer duration of detection of diabetes and the risk is associated with modifiable factors such as obesity, glycemic control, elevated blood pressure, older age, tobacco use and some other biological factors [14– 17,22, 41]. Again, obesity was in increasing trend worldwide [1-5]. Thus, it is expected that prevalence of retinopathy due to obesity will be in increasing trend . On that expectation, it was decided to identify some responsible variables for obesity- retinopathy among 995 Bangladeshi adults of 18 years and above residing in both urban and rural localities.
The present analysis was based on data recorded from 49.9% males [34]. Among them 8.5% were suffering from obesityretinopathy. They were 30% more exposed to this health hazard. In the sample, there were 30.2% obese adults and 25% of them had the problem of retinopathy. The chance of facing the problem of retinopathy by overweight and obese adults was 14% more as it was in others [R.R.=1.14]. The percentage of adults suffering from obesity-retinopathy was 7.5 in the sample. There were 46.6% urban adults and 7.8% of them were suffering from the disease. But urban and rural adults were similarly exposed to this health problem. In the sample, there were 85.2% Muslim and they were 14% more exposed to this health hazard. The percentage of married adults was 93.1 and they were 85% more exposed to obesity-retinopathy. The largest group of adults belonged to the age group less than 40 years. For them the chance to be affected by this problem was 2.08 times as it was in others. Similar findings were noted in earlier studies [14,17]. The respondents having at least secondary level education were more exposed to obesity-eye problem. In the sample, there were 43% service and retired persons and they were 32% more exposed to this health problem compared to other professionals. Some noncommunicable diseases were termed as lifestyle health hazard [4,42-45]. Again, lifestyle changes with the change in family income and family expenditure and these two variables enhance the change in food habit, smoking habit and working habit of the family members [4,41.42,46]. In the sample, 6.1% adults were from richer families. They were 65 % more exposed to obesity retinopathy. Another richer group (spending monthly Taka 60 – 80 thousand) was 69% more exposed to the problem. But prevalence of obesity retinopathy was significantly associated with neither family income nor family expenditure. Each of the variable viz. consumption of process food, smoking habit, physical activity and sedentary activity was independent of prevalence of obesity retinopathy. But the process food consumers, smokers, and physically inactive adults were more exposed to this health problem.
Among obese persons diabetes and hypertension are dominant [42,43,47,48]. Again, diabetes, duration of it and hypertension are the causes of retinopathy [14,15,48,49]. This study also indicated that prevalence of obesity eye problem was significantly associated with blood pressure and duration of diabetes. However, adults of optimal blood pressure were more exposed to this health hazard. Similar finding was reported in one study [47]. Those who were suffering for longer duration from diabetes they were also more exposed to the problem.
Conclusion
The study was conducted to identify the variables responsible for prevalence of obesity retinopathy among Bangladeshi adults of 18 years and above. For the purpose, 995 respondents were interviewed. Among them 46.6 % were from urban area. The urban and rural adults were similarly exposed to this health hazard. Percentages of females, Muslims and married adults were 49.9, 85.2 and 93.1, and they were exposed more by 30%, 14% and 85%, respectively. There were 19.7% youngest adults. This group was 91% more exposed to the problem. Percentage of at least secondary level educated respondents was 81.3 and they were 180% more exposed to the problem. Percentage of service persons and retired persons together was 43. These two groups were exposed 32% more compared to other professionals. Percentage of housewives was 23.1 and 8.7% of them were affected by the disease. The chance of prevalence of the disease for them was 37% more as it was for others. Adults (6.1%) coming from higher income and higher expenditure (14.4%) group of families were exposed to this health hazard by more than 65% and 69%, respectively. Adults (36.5%) habituated in taking process food was 11% more exposed to obesity retinopathy. Physically inactive adults were 51.7%. For them the risk of the disease was 11% more. Diabetic adults and smokers were 67% and 33.1%, respectively. These two groups were almost similarly exposed compared to their counter parts. Sedentary activity was not the risk factor for obesity retinopathy. But low level of blood pressure and longer duration of diabetes with intensive glucose control were the risk factors for this health hazard.
The discriminant analysis indicated that the most responsible variable for obesity retinopathy was blood pressure followed by age, education, occupation, gender variation, marital status and prevalence of diabetes.
Bangladesh is a developing country and its economy is in upward trend. Due to this, there is upward social mobility and hence obesity and health hazard of its people cannot be avoided. But obesity is a source of modifiable non-communicable diseases and it can be reduced to a great extent so that some noncommunicable diseases can be controlled. For this, Government and its policy makers can do a lot through health service providers working in both urban and rural areas. Social workers, and medical practitioners can encourage the people in leading healthy lifestyle. People can be advised
a) To do any sort of physical labour and physical exercise so that body weight can be controlled.
b) To avoid restaurant food, can food, process food and salty and fatty food.
c) To take healthy and homemade food as per as possible. To join the blood and eye screening program and blood pressure checking program whenever it is possible..
References
- Dhurandhar NV (2001) Contribution of pathogene in human obesity. Drug News & Perspectives 7(5): 307-313.
- Berg C, Rosengren A, Aires N, G Lappas, K Torén, et al. (2005) Trends in overweight and obesity from 1985 to 2002 in Goteborg, west Sweden. International Journal of Obesity 29(8): 916-924.
- Skliros EA, Merkoures P, Sotiropoulos A, C Xipnitos, Helen Liva, et al. (2008) The relationship between body mass index and hypertension in elderly Greeks; the Nemea Primary Care Study. J Am Geriatr Soc 56(5): 954-955.
- Bhuyan KC, Fardus J (2020) Level of obesity and socioeconomic factors of a group of adult people of Bangladesh: A factor analysis approach. Amer Jour Data Mining and Knowledge Discovery 4(1): 8-14.
- (2011) WHO fact sheet n0
- Bertino G, Ardiri AM, Ali FT, P M Boemi, D Cilio, et al. (2006) Obesity and related diseases : an epidemiologic study in eastern Sicily. Minerva Gastroenterol Dietol 52(4): 379-385.
- Calamusa G, Amodio E, Costantino C, Pasquale MD (2012) Body mass index and factors associated with overweight and obesity: A cross-sectional study of adult subjects living in a small city of Western Sicily (Italy). IJPH 9(3): e7539-1-e7539- 8.
- Bhuyan KC (2020) Identification of socioeconomic variables responsible for diabetic heart diseases among Bangladeshi adults, ARC Jour Dia Endo 5(2): 1 -8.
- van Leiden HA, Dekker JM, Moll M, Stehuwer CDA, Polak BCP (2002) Blood pressure, lipids, and obesity are associated with retinopathy, The Hoorn. Diabetic Care 25: 1320-1325.
- Prasad SB, Fahrtash F, Malaiapan Y, Ian T Meredith, James Cameron, et al. (2009) Obesity and the metabolic syndrome in patients with acute myocardial infraction. International Journal of Cardiology 144(3): 450-451.
- Redon J, Cifkova R, Laurent S, Peter Nilsson, Krzysztof Narkiewicz, et al. (2008) The metabolic syndrome in in hypertension: European Society of hypertension position statement. J Hypertens 26(10): 1891-1900.
- Basen Engquist K, Chang M (2011) Obesity and cancer risk: recent review and evidence. Curr Oncol Rep 13(1): 71-76.
- Price SA, Gorelik A, Fourlanos S, Colman PG, Wentworth JM (2014) Obesity is associated with retinopathy and macrovascular disease in type 1 diabetes. Obes Res Clin Pract 8(2): e178-e182.
- Klein R, Klein BR, Moss CE, Dvies MD, DeMets DL (1984) The Wisconsin Epidemiologic Study of Diabetic Retinopathy. III Prevalence and risk of diabetic retinopathy when age at diagnosis is 30 or more years. Rch Opthalmol 102: 527-532.
- Stratom IM, Kohner EM, Aldington SJ, Turner RC, Holman RR, et al. (2001) UKPDS 50: risk factors for incidence and progression of retinopathy in type ii diabetes over 6 years from diagnosis. Diabetologia 44: 156-163.
- Dirani M, Xie J, Fenwick E, Benarous R, Rees G, et al. (2011) Are obesity and anthropometry risk factors for diabetic retinopathy? Invest Ophthalmol Vis Sci 52(7): 4416-4421.
- Yu T, Mitchel P, Berry G, Li W Wang J (1998) Retinopathy in older persons without diabetes and its relationship with hypertension, Arch Opthalmol 116: 83-89.
- World Health Organization (1997) Global initiative for the elimination of avoidable blindness. An informal consultation, pp. 97 -61.
- World Health Organization (2006) Consultation of Diabetes Mellitus.
- Lee VS, Kingsley ET (1993) The diagnosis of diabetic retinopathy. Opthalmoscopy vs fundus photography. Opthalomogy 100(10): 1504-1512.
- World Health Organization (2017) Nepal Tackles Diabetic Retinopathy.
- World Health Organization (2020) Monitoring Health for SDGs, WHO.
- Maya GP (2020) Diabetic retinopathy and blindness: An epidemiological overview. Intech Open.
- Ahmed KR, Karim MN, Bhomik B, Habib SH, Bukht MS, et al. (2012) Incidence of diabetic retinopathy in Bangladesh: a 15 year follow-up study. J Diabete 4(4): 386-391.
- WHO (2007) The challenge of obesity in the WHO European region and the strategies for response. In: Branca F, Nikogosion H, Lobstein T, Copenhagen, USA.
- Srinivasan S, Dehghani C, Pritchard N ( 2018) Opthalmic and clinical factors that predict four-year development and worsening of diabetic retinopathy in type – diabetes. Jour Diabetes Complications 32: 67-74.
- Hietala K, Forsblom C, Summanen P (2008) Heritability of proliferative diabetic retinopathy. Diabetes 5: 2176-2180.
- Rema M, Saravanan G, Deepa R, V Mohan (2002) Familial clustering of diabetic retinopathy in South Indian type-2 diabetic patients. Diabetic Med 19(11): 910-916.
- Cheung CY, Hui EY, Lee CH (2016) Impact of genetic loci identified in genome- wide association studies on diabetic retinopathy in Chinese patients of type – 2 diabetes. Diabetes Invest Opthalmol Vis Sci 57(13): 5518- 5524.
- Kempen JH, O’ Colmain BJ, Leske MC, Steven M Haffner, Ronald Klein, et al. (2004) The prevalence of diabetic retinopathy among adults in the United States. Arch Opthalml 122(4): 552-563.
- Gavin S Tan, Alfred Gan, Charumathi Sabanayagam, Yih Chung Tham, Kumari Neelam, et al. ( 2018): Ethnic differences in the prevalence and risk factors of diabetic retinopathy : The Singapore Epidemiology of Eye Diseases Study. Opthalmology 125: 529-536.
- Huang YC, Li JM, Lin HJ, Ching-Chu Chen, Shih-Yin Chen, et al. (2011) Genome- wide association study of diabetic retinopathy in a Taiwanese population. Opthalmology 118(4): 642-648.
- Ma RC (2016) Genetics of cardiovascular and renal complications in diabetes. Jour Diabetes Investig 72(2): 139-154.
- Bangladesh Bureau of Statistics (2018): Statistical Year Book of Bangladesh, 2017, BBS, Dhaka , Bangladesh.
- Biswas T, Garnett P Sarah, Rawal B Lal (2017) The prevalence of underweight, overweight, and obesity in Bangladesh: Data from a national survey. PLoS One 12(5): e0177395.
- (2004) Appropriate Body Mass Index for Asian Population and its Implications for Policy and Intervention Strategies, WHO Expert Consultation, Public Health, Lancet, pp. 363.
- Jan AS, Yan Li, Azusa H, Kei A, Eamon D (2017) Blood pressure measurement anno 2016. Amer Jour Hypertens 30(5): 453.
- McLachlan GJ (2004) Discriminant analysis and Statistical Pattern Recognition, Wiley Interscience.
- Garson GD (2008) Discriminant function analysis.
- Bhuyan KC (2020) A note on the application of discriminant analysis in medical research. Archives of Diabetes and Obesity 2(2): 142-146.
- Diabetes Research and Clinical Practice (2020) Obesity, Hyperglycemia and Tobacco use are Modifiable Risk Factors for Retinopathy.
- Bhuiyan D, Bhuyan KC (2020) Discriminating Bangladeshi adults by non-communicable diseases, Rehabilitation Science 4(3): 35-43.
- Bhuyan KC, Mortuza A, Fard J (2018) Discriminating patients suffering from non-communicable diseases: A case study among Bangladeshi adults, Biomed J Sci & Tech.
- Md Mortuza A, Bhuyan KC, Fardus J (2018) A study on identification of socioeconomic variables associated with non-communicable diseases among Bangladeshi adults. Amer J Biomed Sci and Engineering 4(3): 24-29.
- Bhuyan KC (2020) Discriminating Bangladeshi adults by simultaneous prevalence of obesity diabetes. Ser Endocrinology Diabetes and Metabolism 2(2): 19-26.
- Dinsa GD, Goryakin Y, Fumagalli E, Suhrcke M ( 2012) Obesity and socioeconomic status in developing countries: A systematic review. Obesity Reviews 13(11): 1067-1079.
- Beutens JWJ, Patel A, Vingerling JR, Cruickshank JK, Hughes AD, et al. (2009) Effects of blood pressure lowering and intensive glucose control on the incidence and progression of retinopathy in patients with type 2 diabetes mellitus: A randomized controlled trial. Diabetologia 52(10): 2027-2036.
- Henderson AD, Bruce BB, Newman NJ, Biousse V (2011) Hypertension –related eye abnormalities and the risk of stroke, Rev Neurol Dis 8(1-2): 1-9.
- Singh NS, Phuritshaban C (2020) Assessment, prevalence and risk factors of hypertensive retinopathy -A clinical Study. International Archives of Biomed Clin Res 5(4).
- Bhuyan KC (2020) Factors responsible for elevated blood pressure among Bangladeshi adults. BJSTR 29(5): 22755- 22761.
- Henderson AD, Bruce BB, Newman NJ, Biousse V (2011) Hypertension-related eye abnormalities and the risk of stroke. Rev Neural Dis 8(1-2): 1-9.
- Singh NS, Phuritshabam C (2020) Assessment of prevalence and risk factors of hypertensive retinopathy: A Clinical Study. International Archives of Biomed Clin Res 5(4).






























