Use of Nutrient-Dense Functional Foods in the Management of Type 2 Diabetes Mellitus
Nicholas G Morehouse1, Kate Bauer2, Vasuki Wijendran2, Pei-Ra Ling3, Charles Marsland4 and Stacey J Bell5*
1Lead Clinical Research Scientist, Nutrient, USA
2Senior Clinical Research Associate, Nutrient, USA
3Consultant, Nutrient, USA
4Founder and Vice Chairman, Nutrient, USA
5Chief Science Officer, Nutrient, USA
Submission: October 10, 2019; Published: October 21, 2019
*Corresponding author: Stacey J Bell, Chief Science Officer, Nutrient, 110 Woodland Street, Reno, NV 89523, USA
How to cite this article: Nicholas G Morehouse, Kate Bauer, Vasuki Wijendran, Pei-Ra Ling, Charles Marsland, Stacey J Bell. Use of Nutrient- Dense Functional Foods in the Management of Type 2 Diabetes Mellitus. 2019; 12(2): 555834. DOI:10.19080/CRDOJ.2019.11.555834
Abstract
Background: A poor diet, lacking in nutrients and rich in sugar, salt, and saturated fats, promotes obesity, which increases the risk of type 2 diabetes and, if present, makes management harder. Nutrient-dense, portion-controlled functional foods have shown promise in helping people lose weight. The purpose of this single arm, prospective, two-month study was to assess the effect of nutrient-dense functional foods on glycemic management in patients with type 2 diabetes, who were overweight or obese.
Methods: Subjects were recruited via social media and if they met the entry criteria were provided five, easy-to-prepare nutrient-rich functional foods each day. Self-reported measurement of body weight, fasting blood glucose (two times weekly), post-prandial blood glucose (two times weekly), and quality of life ratings were provided weekly; waist circumference was measured at baseline and monthly thereafter.
Results: Thirty-four subjects enrolled in the study and 18 completed it (53%). The mean age was 55± 8 years and the body mass index (BMI) average was 34±4; most were obese (85%). Most participants consumed three nutrient-dense meals daily (47%), while 17% consumed four meals and 17% five meals daily. Non-significant decreases occurred in mean body weight over the first four weeks (98±18 kg to 93±15 kg) and remained mostly unchanged at week 8 (92±15 kg). Weight loss at week 8 was 6%, which is considered to be medically significant. BMI decreased more between baseline and week 4 (34±4 to 32±3 kg/m2) compared to change between week 4 and week 8. Compared to baseline, BMI at week 4 (P = 0.01) and week 8 (P = 0.003) were significantly lower. Waist circumference decreased for both women (107±13 cm at baseline to 102±15 cm at week 8), and men (110±16 cm at baseline to 100±11 cm at week 8). Compared to baseline, at week four, post-prandial blood glucose, but not fasting concentrations, were significantly lower (216±72 vs. 172±54 mg/dL; p = 0.02). By week 8, both fasting blood glucose (P = 0.007) and post-prandial concentrations (P = 0.003) were significantly lower than at baseline. At baseline (n=33), the mean HgbA1c was 8.6±1.9 %. By week 8, the percent decrease exceeded what would be expected from oral antidiabetic agents (n=5; 0.5-1.25%). Each quality of life attribute improved significantly (P < 0.05) over the eight weeks, except gastrointestinal symptoms, with the greatest benefits were for improved diet quality, increased energy, better sleep, better appearance, and generally feeling better.
Conclusions: Eating well and controlling blood sugar go hand-in-hand. However, the diet of patients with type 2 diabetes is nutrient-poor and laden with harmful additives such as sugar, salt, and saturated fats, making management of the condition difficult. Inclusion of up to five, nutrient-dense functional foods that are low harmful additives was beneficial to individuals with type 2 diabetes by significantly improving glycemic control, for both fasting blood glucose and post-prandial concentrations. The decrease in HgbA1c exceeded what would have been expected from oral antidiabetic agents. These improvements were coupled with a 6% weight loss and decreases in waist circumference. New dietary strategies are needed for patients with type 2 diabetes and nutrient-dense functional foods may be a good option.
Keywords: Type 2 diabetes; Diet; Functional foods; Nutrient-dense foods; Blood sugar management; Diet and diabetes
Abbrevations: BMI: Body Mass Index; CVD: Cardiovascular Disease; HbA1c: Hemoglobin A1c; DV: Daily Value; AI: Adequate Intakes; FBG: Fasting Blood Glucose; GI: Gastrointestinal Symptoms
Introduction
According to the American Diabetes Association about 9.4% of the population has type 2 diabetes mellitus (about 30 million people) [1]. Of this, about 25% are undiagnosed. However, including those who have prediabetes and are undiagnosed, the prevalence has been reported to be closer to 50% of the population [2]. Diabetes is a group of chronic diseases characterized by hyperglycemia, which damages the body [3]. Generally, the injurious effects of hyperglycemia are separated into macrovascular complications (coronary artery disease, peripheral arterial disease, and stroke) and microvascular complications (diabetic nephropathy, neuropathy, and retinopathy). The relationship between dementia risk and hemoglobin A1c (HgbA1c) has recently been identified [4]. Over ten years, HgbA1c levels were linearly associated with subsequent cognitive decline irrespective of diabetes status at baseline.
The American Diabetes Association acknowledges that the most challenging part of a diabetes treatment plan is determining what to eat and then following a healthy meal plan [5]. The most comprehensive study, Look AHEAD, lasting nearly ten years compared an intensive lifestyle management program (i.e., diet, exercise, behavior) to a much less aggressive dietary and educational intervention [6]. Despite showing no difference between the two groups for cardiovascular events (the primary outcome), there were numerous benefits of the intensive intervention group including: improved biomarkers of glucose and lipid control, less sleep apnea, lower liver fat, less depression, improved insulin sensitivity, less urinary incontinence, less kidney disease, reduced need of diabetes medications, maintenance of physical mobility, improved quality of life, and lower costs. However, a newer analysis of these data showed that a subset of participants experienced deleterious effects from the combination of intensive lifestyle management and weight loss [7].
It may be that the inability to reduce cardiovascular disease (CVD) risk and avoid harm in some patients was that these things were not considered: the genotypes of subjects, the numerous anti-diabetes medications used that affect the metabolome differently, and variations in the gut microbiome [8]. Future studies need to appreciate these variables, so that the findings allow clinicians to design personalized nutritional approaches for type 2 diabetes management.
Up to 90% of type 2 diabetes can be prevented by adopting a healthy diet and lifestyles including engaging in physical activity, getting adequate sleep, and not smoking [9]. A healthy diet is defined by one that is nutrient-dense, especially rich in plant-based oils and proteins, fiber, and containing all essential nutrients. Foods of high diet quality to include are vegetables, fruits, nuts and legumes, long-chain fats, and whole grains. Others of poor quality should be limited: sugar-sweetened beverages, red and processed meat, saturated fat, and sodium; and moderate alcohol consumption. Adoption of these dietary recommendations was strongly associated with a lower type 2 diabetes risk. This eating pattern is supported based on a metaanalysis including 48 studies [10].
Despite the overwhelming evidence of what constitutes a healthy diet, paradoxically, it is rarely adopted by those with type 2 diabetes [11,12]. Most individuals with type 2 diabetes overconsume what should be limited (e.g., salt, sugar, and saturated fats) and under-consume the aforementioned healthy foods. The poor diet is mainly from ultra-processed and addictive foods, thus disallowing someone to lose weight and reduce disease risk [12]. Admittedly, these ultra-processed foods are less expensive, tastier, have a long shelf life (i.e., will not spoil like the recommended healthy foods), and are easier to prepare than those that have been shown to reduce disease risk.
New dietary strategies are needed that are healthy and will be incorporated into the lives of those with type 2 diabetes. One popular approach is adhering to a ketogenic diet [13]. The results are promising, showing that being in ketosis was safe and can improve HbA1c, weight, and other biomarkers, while reducing diabetes medication use. However, a ketogenic diet appears to offer no advantage in glycemic management compared to other diets [14]. In addition, adherence to a very low-carbohydrate diet is tedious, and without careful management, could lead to micronutrient deficiencies.
Functional foods that meet healthy dietary criteria may be a useful way to lose weight and manage blood glucose levels. These are foods enhanced with bioactive ingredients and have demonstrated health benefits [15]. Functional foods usually have demonstrated beneficial physiological effects in the prevention, management, and/or treatment of chronic disease that is beyond basic nutrition. The functional foods can come from conventional foods or from the addition of a bioactive constituent in conventional food like vitamins and minerals. Novel nutrient-dense, functional foods and beverages like those used in this study have already been shown to produce a medically significant weight loss [16,17].
The purpose of this prospective, single-armed study is to evaluate the effect of nutrient-dense, portion-controlled, functional foods and beverages in patients with type 2 diabetes.
Materials and Methods
Subjects
For this single-armed, prospective dietary study in type 2 diabetes, subjects were recruited by third-party patient recruitment specialists, who used print ads and digital advertising (i.e., social media). This group facilitated the process of identifying, scheduling, and forwarding potential participants to the study’s clinical research coordinators. Entry criteria included those 50 years of age and older, were overweight or obese, had type 2 diabetes for more than five years, and the hemoglobin A1c (HbA1c) was greater than 5.7%. Subjects provided written informed consent in which they agreed to regularly test their blood glucose levels and consume five nutrient-dense, functional foods daily for eight weeks. All data were self-reported and submitted electronically on to HIPAAprotected area. Each participant was provided regular coaching by one of us (NM), which occurred at least weekly to assist with compliance.
Diet
Subjects were provided five nutrient-dense, portioncontrolled functional foods daily over two months. Foods were provided at no charge and were easy-to-prepare; most required just the addition of hot or cold water or milk. Participants could choose from a variety of options such as shakes, cold and hot cereals, food bars, and hot meals (e.g., beans and rice, noodles and cheese sauce) (http://nutrientfoods.com). Each functional food contained at least 25% of the Daily Value (DV) for every vitamin and mineral, except sodium and chloride. At least 25% Adequate Intakes (AI) for omega-3s were also included in each offering. Free nutrition coaching was provided to assist with questions about the dietary intervention and aid compliance. Each week, the participants reported how many of the five functional foods they consumed and how much of each.
In addition to consuming the nutrient-dense foods, the participants were counseled according to American Diabetes Association guidelines for healthy eating. Recipes that complied with these guidelines were also provided for using the nutrientdense foods.
Anthropometric and blood testing
Body weight and waist circumference were measured at baseline and then weight was tracked weekly and waist measured, monthly. Disease risk for chronic diseases (i.e., hypertension, type 2 diabetes, and CVD) was determined from body weight and waist circumference at baseline and the end of the study [18].
At baseline, subjects submitted fasting blood glucose, postprandial glucose, and HbA1c obtained from their doctor within the past three months. Once the dietary intervention began, on two different days each week, participants measured fasting blood glucose (FBG) after at least an 8-hour overnight fast, and post-prandial blood glucose after any meal but within 60 minutes of finishing it. Change in HgbA1c and reported as a percentage was determined by subtracting the week 8 value from the baseline one.
Quality of life questionnaire
At baseline and weekly, subjects answered eight questions about their quality of life. Each was rated using a scale of one to five, with 5 being the best and 1 being the worst. Questions probed: general feeling, fullness, mood, energy level, any gastrointestinal symptoms (GI), sleep quality, appearance, and overall diet quality. The percentage change between the mean at baseline and week 8 was calculated.
Statistics
Data are expressed as means±standard deviations. The P value is estimated by Student-unpaired t-test. Statistical significance is set as P < 0.05.
Results
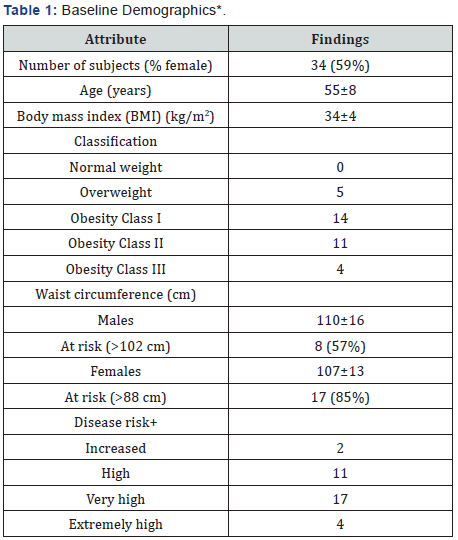
*Data Presented as Mean±Standard Deviation
+Disease Risk for Hypertension, Cardiovascular Disease, and Type 2 Diabetes [18].
Thirty-four subjects enrolled in the study and 18 completed it (53%), of which 59% were female (Table 1). At baseline, the mean age of the participants was 55±8 years, and the body mass index (BMI) average was 34±4 kg/m2. Only 15% were classified as being Overweight and the rest had Obesity. Obesity was further classified according to severity and 14 had the least severe form (Class I), 11 had moderate obesity (Class II), and 4 had the severest form (Class III). Waist circumference was at high risk for 57% of men (> 102 cm) and 85% of women (> 88cm). Using both BMI and waist circumference to calculate disease risk, 2 participants were at Increased risk, 11 had High risk, 17 were at Very High risk, and 4 had Extremely High risk.
Most participants (47%) consumed three of the nutrientdense meals daily; only 17% of the consumed four meals and the same percentage ate five meals daily. About the same (18%) consumed only about 2.5 meals daily.
Of those who responded to the exercise-related questions (n=15), eight excised three hours weekly, five exercised four hours each week, and two did less than two hours weekly, on average. Most people (9/15) exercised for 30 minutes, but the range was 20-90 minutes. Favorite activities included walking, swimming, and spinning.
Anthropometry and disease risk
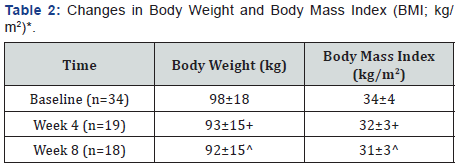
*Data Presented as Mean±Standard Deviation. P is Estimated Using Student’s Unpaired t-test. +Compared to Baseline; P: 0.29 for Weight and P: 0.01 for BMI ^Compared to Baseline; P: 0.23 for Weight and P: 0.003 for BMI
Body weight decreased over the first four weeks by 5 kg going from 98±18 kg to 93±15 kg and stabilized until the end with a mean body weight of 92±15 kg (Table 2). Changes in body weight were not significant over time but represent a 6% decrease, which is medically significant. BMI declined most between baseline and week 4 (34±4 to 32±3 kg/m2). At the end, BMI as nearly the same at week 4 (31±3 k/m2). Compared to baseline, BMI at week 4 (P = 0.01) and week 8 (P = 0.003) were significantly lower.
Waist circumference decreased for both women (107±13 cm at baseline to 102±15 cm at week 8), and men (110±16 cm at baseline to 100±11 cm at week 8) (Table 3). The percentage of women with high risk waist circumferences remained stable throughout the study at around 85% of the group. Men with high risk waist circumferences decreased – 57% were at high risk at baseline and 33% were at week 8.
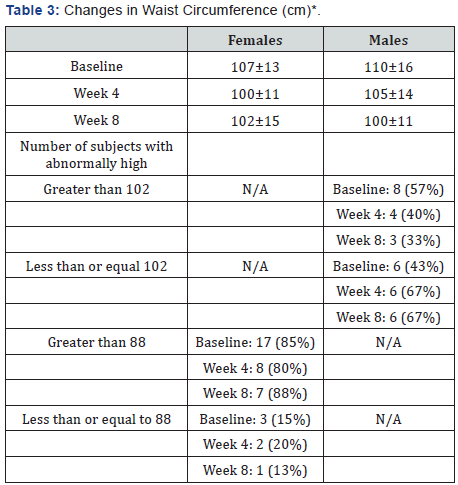
*Data Presented as Mean±Standard Deviation
Disease risk using BMI and waist circumference were available for 17 subjects for baseline and week 8. Of these, 4/17 participants experienced a decrease in disease risk (3 males; 1 female), 2/17 increased disease risk (1 male, 1 female), and 13/17 had no change (5 males; 6 females).
Glycemic measurements
Compared to baseline, week 4 fasting blood glucose concentrations were not significantly lower, but post-prandial levels were (baseline: 216±72; week 4: 172±54 mg/dL; p = 0.02). By week 8, both fasting blood glucose and post-prandial concentrations were significantly lower than at baseline. At baseline, mean fasting blood glucose concentration was 161±49 mg/dL, and at week 8 the mean was 130±25 mg/dL (P = 0.007). Similarly, the mean post-prandial blood glucose concentration was 216±72 mg/dL at baseline and decreased to 161±44 mg/dL at week 8 (P = 0.003) (Table 4).
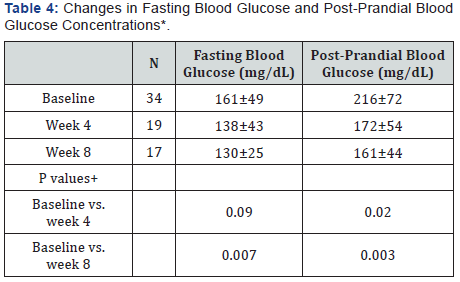
*Mean±S.D. +P is estimated by Student-Unpaired t-test. The statistical significance is determined by P < 0.05.
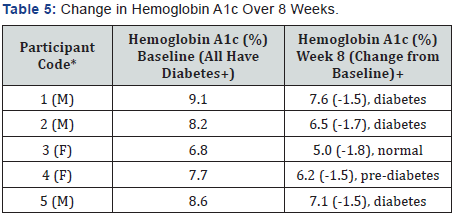
Gender: M: Male; F: Female +According to the Centers for Disease Control [19], Hemoglobin A1c is Defined as: Normal < 5.7%, Pre-diabetes: 5.7% to 6.4%, Diabetes ± 6.5%
At baseline (n=33), the mean HgbA1c was 8.6±1.9 %. By week 8, data were only available for five participants (Table 5). At baseline, these five participants were classified as having diabetes according to the HgbA1c percentage [19]. At week 8, all experienced a decrease in HgbA1c with three subjects experiencing a reduction of 1.5%; one had a decrease of 1.7%, and one decreased 1.8%. At the end based on HgbA1c, one normalized, one became pre-diabetic, and three continued with diabetes. Weight loss was not related to percentage decrease in HgbA1c (data not shown).
Quality of life
Each quality of life attribute improved significantly (P≤0.05) over the eight weeks, except gastrointestinal symptoms, which remained unchanged (Table 6). The greatest improvements (> 30%) determined by the percentage increase between week 8 and baseline were observed for: improved diet quality, increased energy, better sleep, better appearance, and generally feeling better.
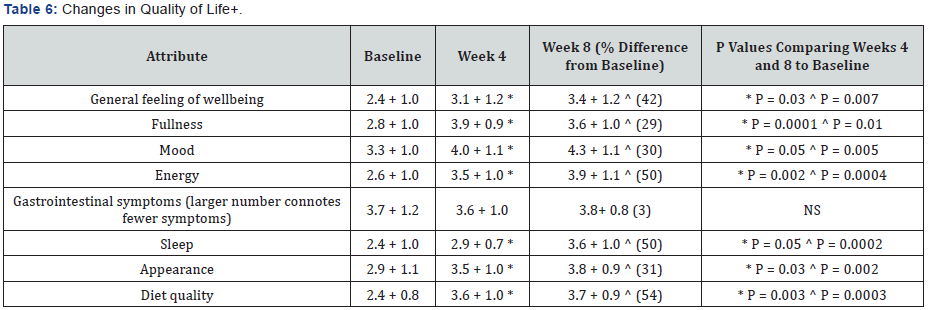
+Rating Scale used was 1 to 5, with 1 being the Worst and 5 being the Best. Data presented as Means±S.D. Statistical significance determined by Student-Unpaired t-test, p ≤ 0.05. *Week 4 Compared to Baseline ^Week 8 Compared to Baseline
Discussion
Type 2 diabetes, like other chronic conditions, is caused by a poor diet and lifestyles. Participants with type 2 diabetes in this study stated that they wanted to eat better, and agreed to consume five, healthy nutrient-dense, easy-to-use, portioncontrolled, functional foods for eight weeks. Use of five of these meals daily was shown to promote weight loss in overweight subjects, who did not have type 2 diabetes [16,17].
Most of the participants in this study ate an average of three meals daily, and still experienced a 6% weight loss and a significant decrease in BMI by week 8 (P = 0.003). More importantly was that glucose management improved, exemplified by significant decreases in fasting blood glucose and post-prandial levels (P < 0.05). In addition, the five subjects who provided HgbA1c data at the beginning and end of the study, experienced decreases that exceeded what would be expected from oral antidiabetic agents. quality of life indicators [20]. The participants had decreases over eight weeks of HgbA1c of 1.5% to 1.8%; oral agents typically reduce it by 0.5% to 1.25% after 12 weeks.
The participants found incorporation of nutrient-dense, portion-controlled, functional foods into their lives fairly easy, but regular nutritional counseling was required to assure compliance. One of us (NM) had at least weekly contact with the participants and shared ideas how to prepare the nutrientdense meals and what else to eat. The participants that completed the study were pleased with their results and had significant improvements in all quality of life indicators except gastrointestinal symptoms, which did not change.
One limitation of the study is the self-reporting of data, but it is customary for patients with type 2 diabetes to monitor their blood glucose levels and report their readings to their physicians. Admittedly the drop-out rate was high and seems to be related to the difficulty of people with type 2 diabetes to change their diets. However, those that remained benefited in a variety of ways including weight loss, glycemic management, and quality of life.
Conclusions
The diet of patients with type 2 diabetes is nutrient-poor and rich in harmful additives like salt, sugar, and saturated fats, making management of the condition difficult. Inclusion of up to five, nutrient-dense, functional foods that are low harmful additives was beneficial to these patients by significantly improving glycemic control, both for fasting blood glucose and post-prandial concentrations. The decrease in HgbA1c exceeded what would have been expected from oral antidiabetic agents. These improvements were coupled with a 6% weight loss and decreases in waist circumference. New dietary strategies are needed for patients with type 2 diabetes and nutrient-dense, functional foods may be a good option.
Funding
Nutrient, Reno, Nevada, supported this study by providing food at no charge to the participants and for salary support for all co-authors except Nicholas Morehouse.
Acknowledgment
The authors are grateful to the participants who dutifully completed their weekly data collections forms and carefully monitored their blood glucose levels. It is difficult to change one’s diet, but these patients with type 2 diabetes did and were pleased with the results.
Declaration of Conflicting Interest
Nicholas Morehouse oversaw this study in partial fulfillment of a Master of Science degree. Dr. Ling was the statistical consultant. The other co-authors are full-time employees at Nutrient, the company that manufactures and sell the nutrientdense functional foods used in this study.
References
- http://diabetes.org/diabetes-basics/statistics/
- Menke A, Casagrande S, Geiss L, Cowie CC (2015) Prevalence of and Trends in Diabetes Among Adults in the United States, 1988-2012. JAMA 314(10): 1021-1029.
- Fowler MJ (2008) Microvascular and Macrovascular Complications of Diabetes. Clinical Diabetes 26(2): 77-82.
- Zheng F, Yan L, Yang Z, Zhong B, Xie W (2018) HbA1c, diabetes and cognitive decline: the English Longitudinal Study of Ageing. Diabetologia 61(4): 839-848.
- (2019) Lifestyle Management: Standards of Medical Care in Diabetes 2019. Diabetes Care 42(Suppl 1): S46-S60.
- Pi-Sunyer X (2014) The Look AHEAD Trial: A Review and Discussion of Its Outcomes. Curr Nutr Rep 3(4): 387-391.
- de Vries TI, Dorresteijn JAN, van der Graaf Y, Visseren FLJ, Westerink J (2019) Heterogeneity of treatment effects from an intensive lifestyle weight loss intervention on cardiovascular events in patients with type 2 diabetes: data from the Look AHEAD trial. Diab Care 42(10): 1988-1994.
- Wang DD, Hu FB (2018) Precision nutrition for prevention and management of type 2 diabetes. Lancet Diabetes Endocrinol 6(5): 416-426.
- Ley SH, Ardisson Korat AV, Sun Q, Tobias DK, Zhang C, et al. (2016) Contribution of the Nurses’ Health Studies to Uncovering Risk Factors for Type 2 Diabetes: Diet, Lifestyle, Biomarkers, and Genetics. Am J Public Health 106(9): 1624-1630.
- Jannasch F, Kro J, Schulze MB (2017) Dietary Patterns and Type 2 Diabetes: A Systematic Literature Review and Meta- Analysis of Prospective Studies. J Nutr 147(6): 1174-1182.
- (2015) Dietary Guidelines for Americans 2015-2020. (8th edn).
- Hall KD, Ayuketah A, Brychta R, Cai H, Cassimatis T, et al. (2019) Ultra-Processed Diets Cause Excess Calorie Intake and Weight Gain: An Inpatient Randomized Controlled Trial of Ad Libitum Food Intake. Cell Metab 30(1): 67-77.
- Hallberg SJ, McKenzie AL, Williams PT, Bhanpuri NH, Peters AL, et al. (2018) Effectiveness and Safety of a Novel Care Model for the Management of Type 2 Diabetes at 1 Year: An Open-Label, Non-Randomized, Controlled Study. Diabetes Ther 9(2): 583-612.
- van Wyk HJ, Davis RE, Davies JS (2016) A critical review of low-carbohydrate diets in people with type 2 diabetes. Diabet Med 33(2): 148-157.
- https://www.canada.ca/en/health-canada/services/food-nutrition/food-labelling/health-claims/nutraceuticals-functional-foods-health-claims-foods-policy-paper.html
- Bell SJ, Ling PR, Marsland C (2016) Nutrient-Dense, Portion-Controlled Meals and Snacks Promote Weight Loss. J Food Technol Nutr Sci 2(1).
- Bell SJ, Ling P-R, Baker RA, Marsland C (2018) Use of self-reported data to determine the effect of nutrient-dense meals on body weight and quality of life. Journal of Nutrition & Food Sciences 8: 3.
- https://www.nhlbi.nih.gov/health/educational/lose_wt/BMI/bmi_dis.htm
- https://www.cdc.gov/diabetes/managing/managing-blood-sugar/a1c.html
- Sherifali D, Nerenberg K, Pullenayegum E, Cheng JE, Gerstein HC (2010) The Effect of Oral Antidiabetic Agents on A1C Levels: A systematic review and meta-analysis. Diabetes Care 33(8): 1859-1864.






























