Is There an Association Between Body Mass Index and Cervical Length?
Hawzheen Q Jalal* and Srwa Khalid Ismail
Consultant Gynecologist and Obstetrician, Iran
Submission: June 10, 2019; Published: September 13, 2019
*Corresponding author: Hawzheen Q Jalal, Consultant Gynecologist and Obstetrician, Iran
How to cite this article: Hawzheen Q Jalal, Srwa Khalid Ismail. Is There an Association Between Body Mass Index and Cervical Length?. Curr Res Diabetes Obes J. 2019; 12(1): 555829. DOI:10.19080/CRDOJ.2019.11.555829
Abstract
Objective: The purpose of this study is to assess the relationship between maternal body mass index and second trimester cervical length.
Methodology: This is a prospective study conducted on 100 single ton gestation women aged between 18 to 34 years with mean age of 24.03 ± 4.34 from 2017 to 2019, all these women have their BMI measured in 1st trimester according to WHO criteria and cervical length measured in 2nd trimester (16-24 weeks).
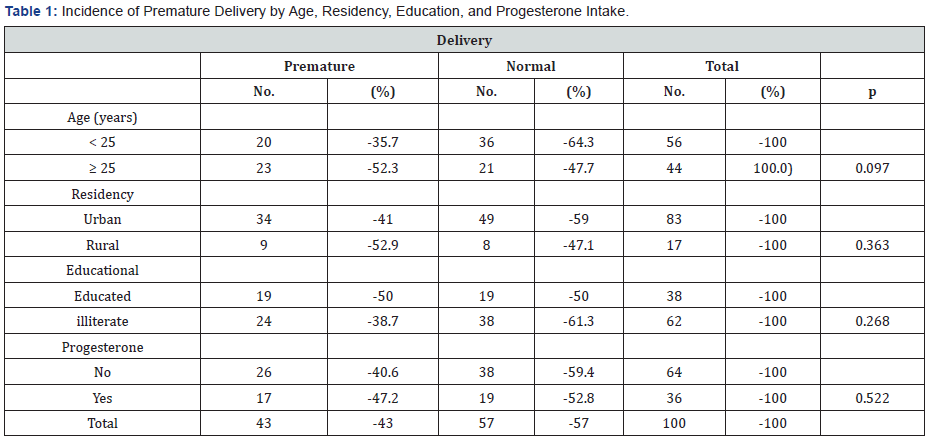
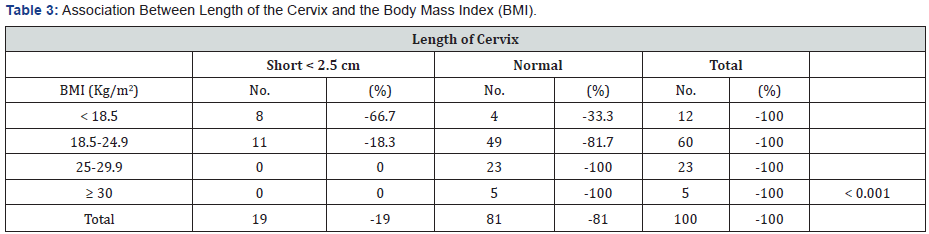
Results: Hundred women participated in the study. Their mean age + SD was 24.03 + 4.34 years, ranging from 18 to 34 years. the rate of premature delivery among women aged ≥ 25 years was 52.3% compared with 35.7% among those aged less than 35 years (p = 0.097). The rate of premature delivery among women living in rural areas was 52.9%, compared with 41% among women living in urban areas (p = 0.363). The more the body mass index (BMI), the less the rate of premature delivery (p = 0.002) where it was 50% among thin women and 0% among obese women. premature delivery was 89.5% among women with short cervical length and 32.1% among women with normal cervical length (p < 0.001). 19% of the women of the whole sample had short cervix but none of the women with normal weight or obese had short cervix. It is evident in the table that 66.7% of thin women had short cervix (p < 0.001).
Conclusion: This study demonstrates a relationship between BMI and cervical length suggesting that obesity may be associated with longer cervical length. These results will need to be replicated in larger cohorts undergoing universal cervical length assessment.
Keywords: Premature delivery; Body mass index; Cervical length; Pregnancy; Morbidity; Fetal acrosomia; Prenatal mortality; Oxytocin; Obese patients; Vaginal ultrasonography; Gestation
Introduction
Obesity and cervical insufficiency are leading causes of morbidity in pregnancy [1]. Over the past two decades in the United States, the rate of obesity has more than doubled from 15 to 33% [2]. It is estimated that more than one in five women of reproductive age are obese (body mass index, BMI > 30 kg/m2), and the rate of obesity continues to rise [3]. Obesity is defined by the National Institutes of health as a body mass index (BMI) of R30 kg/m2 [1]. The prevalence of obesity among adults in the United States has increased from 12% in 1991 to 20.9% in 2001 [4]. Obese women appear to have a lower rate of spontaneous preterm birth than normal weight women [5]. Prior data suggest that maternal obesity in pregnancy is associated with an increased need for labor induction, longer duration of labor, higher oxytocin and misoprostol requirements, and importantly, more frequent cesarean sections [6]. Obesity before pregnancy is associated with an increased risk of fetal acrosomia and prenatal mortality. The mother’s being leaner than average (underweight), on the other hand, is associated with an increased risk of delivering an infant who is small for gestational age and perhaps also the risk of preterm delivery [7]. Pregnancies among underweight or over-weight women are therefore often regarded as high risk pregnancies, and thin women are frequently advised to gain weight before becoming pregnant [8]. Nonetheless, the optimal weight or body-mass index for women who wish to become pregnant is not known [7].
However, evidence regarding the association of maternal obesity and spontaneous preterm birth (SPB) is conflicting [4]. Although some studies suggest that obesity does not influence the rate of preterm birth at !37 weeks of gestation, other studies have found reduced rates of preterm birth in obese and morbidly obese patients [4]. The prevalence of overweight and obesity is increasing among women of childbearing age [9]. An estimated 22% of non-pregnant women 18–49 years of age in the United States are considered overweight (body mass index _BMI_ 25–29.9 kg/m2) and an additional 22% are classified as obese (BMI _ 29.9 kg/m2) [10]. Throughout pregnancy the cervix plays an important role in maintaining the fetus in utero and preventing premature delivery [11]. Currently there are 250,000 preterm deliveries in the United States. The majority of these deliveries are caused by preterm labor and cervical incompetence [11]. Documentation of cervical shortening and dilatation is crucial in the diagnosis and management of cervical incompetence and premature labor.’ Unfortunately, evaluation of the cervix by vaginal examination is subjective and inaccurate because anatomically one half of the cervix is not palpable [12].
The length of the cervix may be useful in predicting the risk of premature delivery, with a shorter cervix predicting a higher risk. Traditional methods to evaluate the cervix in pregnancy are limited and unsatisfactory [13]. Digital examination, the standard method, suffers from large variation among examiners. In contrast, transvaginal ultrasonography is a reproducible method of examination during pregnancy [13]. In a multicenter, population-based study, we used vaginal ultrasonography to measure the length of the cervix and examined the relation of this measurement to the risk of prematurity [14]. Neonates born preterm are at increased risk of both short term complications, attributed to immaturity of multiple organ systems, and longterm adverse health outcomes, such as neuro developmental disabilities, behavioral problems, childhood asthma, cardiovascular disease, diabetes and depression, in adult life [15]. In addition, preterm birth is associated with a substantial economic cost and adverse psychosocial and emotional effects on families [15]. A short cervix, traditionally defined as a transvaginal sonographic cervical length (CL) ≤25mm in the mid-trimester of pregnancy, is an important risk factor for preterm birth and has emerged as one of the strongest and most consistent predictors of preterm birth in asymptomatic women with a singleton or twin gestation [16]. The current study assessed the relationship between first trimester BMI and cervical length measured between 16 and 24 weeks of gestation [17].
Objective of study
To assess the relationship between maternal body mass index and second trimester cervical length.
Data analysis
Data were analyzed using the Statistical Package for Social Sciences (SPSS, version 22). Chi square test of association was used to compare proportions. Fisher’s exact test was used when the expected count of more than 20% of the cells of the table was less than 5. Pearson’s correlation coefficient was calculated to assess the strength of correlation between two numerical variables. A p value of ≤ 0.05 was considered statistically significant
Method
This is a prospective study of 100 women with singleton gestation conducted in Erbil maternal hospital between October 2017 to January 2019. Informed consent were obtained from all of them and the study was approved by KBMS. All of them follow up and delivered in the same hospital. The women who included in this study, their ages were between 18 to 34 years of age with mean age of 24.03±4.34. Gestational age was calculated based on first day LMP and or early first trimester ultrasound. First trimester pregnancy BMI was calculated for women (BMI equal to weight in Kg/height in meter).
Women were classified into two groups according to WHO criteria.
a) Underweight BMI less 18.5. kg/M2.
b) Normal weight BMI 18.5 to 24 .9Kg/m
c) Overweight BMI 25 to 29.9 Kg
d) Class one obesity BMI 30 to 34,9
e) Class two or morbid obesity BMI > 35
Cervical length measured in centimeter by ultrasound scan between 16 and 24 weeks of gestation. Gestational age was based on last menstrual period compared with first trimester ultra-Sonography.
We examined whether there is a relation between cervical length and BMI and their impact on pregnancy outcome.
Inclusion criteria
All primigravida and those with miss carriage only aged between 18-35 years.
5.2. Exclusion criteria
a) Multiple gestations
b) Previous cervical surgeries
c) History of IVF
d) Age less than 18 or more than 35 year
e) No history of any medical diseases.
Results
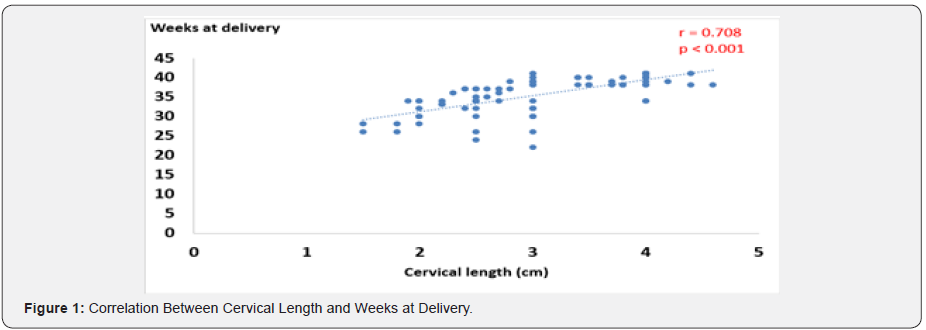
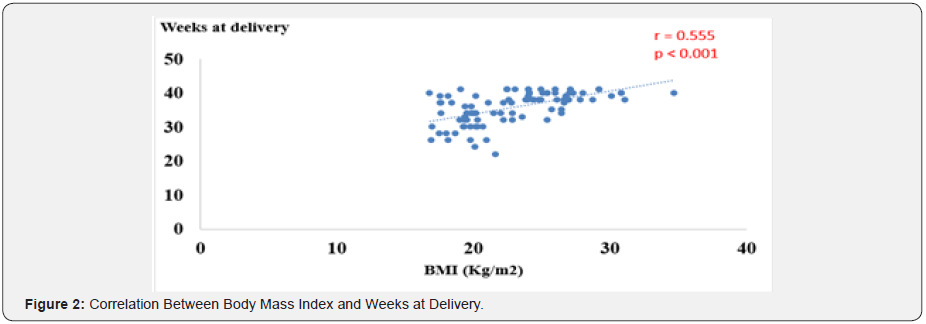
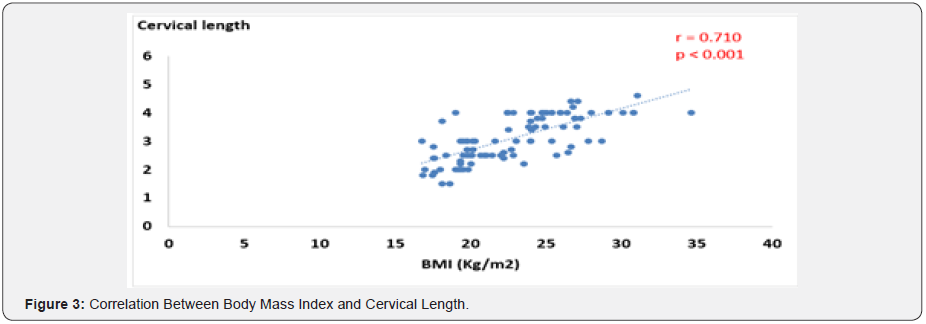
Hundred women participated in the study. Their mean age + SD was 24.03 + 4.34 years, ranging from 18 to 34 years. The median was 23 years. Table 1 shows that the rate of premature delivery among women aged ≥ 25 years was 52.3% compared with 35.7% among those aged less than 25 years (p = 0.097). The rate of premature delivery among women living in rural areas was 52.9%, compared with 41% among women living in urban areas (p = 0.363). No significant association was detected between the rate of premature delivery and the other factors like educational level (p = 0.268), and progesterone intake (p = 0.522) as presented in Table 1. Table 2 shows that the more the body mass index (BMI), the less the rate of premature delivery (p = 0.002) where it was 50% among thin women and 0% among obese women. The same table shows that the rate of premature delivery was 89.5% among women with short cervical length and 32.1% among women with normal cervical length (p < 0.001). Table 3 shows that 19% of the women of the whole sample had short cervix but none of the women with normal weight or obese had short cervix. It is evident in the table that 66.7% of thin women had short cervix (p < 0.001). Figure 1 shows that there was a strong positive correlation between cervical length and the weeks of delivery. The more the cervical length, the more the weeks at delivery (r = 0.708, p < 0.001). The same pattern is observed in Figure 2 where it is evident that the more the body mass index, the more the weeks at delivery (r = 0.555, p < 0.001). Figure 3 shows a positive significant correlation between the BMI and the cervical length (r = 0.710, p < 0.001).

By Fisher’s Exact Test.
By Fisher’s Exact Test.
Discussion
BMI, which is derived from weight and height measurements, is one of the best markers of nutritional status and is used to classify populations from thin to obese [4]. In our study we found that relation between BMI and cervical length is proportional, those patient who have normal or high BMI, they do have normal cervical length, for example those patients who have BMI > 25 and more all of them have normal cervical length, while those patients who have BMI < 18.5 ,66.7 % of them they do have short cervix. These findings suggest that maternal obesity early in pregnancy may be associated with longer cervical length, and a possible explanation for the decreased rate of spontaneous preterm birth and increased rates of induction of labor and cesarean section among obese women. Importantly, these results will need to be replicated in larger cohorts of pregnant women undergoing universal second-trimester transvaginal ultrasound screening of cervical length before further inferences can be made.
Furthermore in our study we find out that 17 cases (89.5%) who have short cervix, they had premature delivery, and this is in concordance to the other study by Mission JF [18], An explanation for why pregnant women with a higher BMI may have a longer cervical length remains to be elucidated. Obese women may have a different physiology, endocrine environment, and profile of comorbid conditions compared with their normal weight counterparts, which could influence cervical length [19,20]. However in the other study conducted by YS Han [8], they f found that the average length of neonates delivered by obese mothers was significantly shorter than the average length of neonates delivered by mothers of normal weight, because of the high rates of preterm and LBW delivery in the obese group.
Conclusion
This study demonstrates a relationship between BMI and cervical length suggesting that obesity may be associated with longer cervical length. These results will need to be replicated in larger cohorts undergoing universal cervical length assessment.
References
- Venkatesh KK, Cantonwine DE, Zera C, Arjona M, Smith NA, et al. (2017) Is There an Association between Body Mass Index and Cervical Length? Implications for Obesity and Cervical Length Management in Pregnancy. Am J Perinatol 34(6): 568-575.
- Pevzner L, Powers BL, Rayburn WF, Rumney P, Wing DA (2009) Effects of Maternal Obesity on Duration and Outcomes of Prostaglandin Cervical Ripening and Labor Induction. Obstet Gynecol 114(6): 1315-1321.
- Chan RSM, Woo J (2010) Prevention of Overweight and Obesity: How Effective is the Current Public Health Approach Int J Environ Res Public Health 7(3): 765-783.
- Hendler I, Goldenberg RL, Mercer BM, Iams JD, Meis PJ, et al. (2005) The Preterm Prediction study: Association between maternal body mass index and spontaneous and indicated preterm birth. Am J Obstet Gynecol 192(3): 882-886.
- Miller ES, Tita AT, Grobman WA (2015) Second-Trimester Cervical Length Screening Among Asymptomatic Women: An Evaluation of Risk-Based Strategies. Obstet Gynecol 126(1): 61-66.
- Kominiarek MA, Vanveldhuisen P, Hibbard J, Landy H, Haberman S, et al. (2010) The maternal body mass index: A strong association with delivery route. Am J Obstet Gynecol 203(3): 264.e1-264.e7.
- Ven S, Nattingius C, Einhold B Ergström R, Ipworth OL (1998) Pre pregnancy Weight and the Risk of Adverse Pregnancy Outcomes 338(3): 147-152.
- Han YS, Ha EH, Park HS, Kim YJ, Lee SS (2011) Relationships between pregnancy outcomes, biochemical markers and pre-pregnancy body mass index. Int J Obes 35(4): 570-577.
- Aina-Mumuney A, Hwang K, Sunwoo N, Burd I, Blakemore K (2016) The Impact of Maternal Body Mass Index and Gestational Age on the Detection of Uterine Contractions by Tocodynamometry. Reprod Sci 23(5): 638-643.
- Zhang J, Troendle JF (2004) Maternal prepregnancy overweight and obesity and the pattern of labor progression in term nulliparous women. Obstet Gynecol 104(5): 943-951.
- Kushnir O, Vigil DA, Izquierdo L, Schiff M, Curet LB (1990) Vaginal ultrasonographic assessment of cervical length changes during normal pregnancy. Am J Obstet Gynecol 162(4): 991-993.
- Hassan SS, Romero R, Berry SM, Dang K, Blackwell SC, et al. (2000) Patients with an ultrasonographic cervical length ≤15 mm have nearly a 50% risk of early spontaneous preterm delivery. Am J Obstet Gynecol 182(6): 1458-1467.
- Iams JD, Goldenberg RL, Meis PJ, Mercer BM, Moawad A, et al. (1996) The Length of the Cervix and the Risk of Spontaneous Premature Delivery. Obstet Gynecol Surv 51(8): 459-460.
- Werner EF, Han CS, Pettker CM, Buhimschi CS, Copel JA, et al. (2011) Universal cervical-length screening to prevent preterm birth: A cost-effectiveness analysis. Ultrasound Obstet Gynecol 38(1): 32-37.
- Romero R, Nicolaides KH, Conde-Agudelo A, O’Brien JM, Cetingoz E, et al. (2016) Vaginal progesterone decreases preterm birth ≤ 34 weeks of gestation in women with a singleton pregnancy and a short cervix: an updated meta-analysis including data from the OPPTIMUM study. Ultrasound Obstet Gynecol 48(3): 308-317.
- Slager J, Lynne S (2012) Assessment of cervical length and the relationship between short cervix and preterm birth. J Midwifery Women’s Heal 57(Suppl 1): 4-11.
- van der Ven J, Kazemier B, van Os M, Kleinrouweler E, Kuiper P (2012) Is cervical length associated with maternal characteristics? Am J Obstet Gynecol 208(1): S288.
- Mission JF, Marshall NE, Caughey AB (2015) Pregnancy Risks Associated with Obesity. Obstet Gynecol Clin North Am 42(2): 335-353.
- Carlhäll S, Källén K, Blomberg M (2013) Maternal body mass index and duration of labor. Eur J Obstet Gynecol Reprod Biol 171(1): 49-53.
- Van Der Ven AJ, Van Os MA, Kleinrouweler CE, De Groot CJM, Haak MC, et al. (2015) Is cervical length associated with maternal characteristics? Eur J Obstet Gynecol Reprod Biol 188: 12-16.






























