Maintenance of Motivation for Lifestyle Change in Overweight and Obese Adolescents: A 6-Month Follow-Up Study
Carolina Domingues Segalla*, Raquel de Melo Boff, Ana Maria Pandolfo Feoli, Andreia da Silva Gustavo, Márcio Vinícius Fagundes Donadio and Margareth da Silva Oliveira
Pontifícia Universidade Católica do Rio Grande do Sul, Brazil
Submission: April 01, 2019; Published: April 25, 2019
*Corresponding author: Carolina Domingues Segalla, Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS), Av. Ipiranga, 6681 – 9th floor, Brazil
How to cite this article: Carolina Domingues Segalla, Raquel de Melo Boff, Ana Maria Pandolfo Feoli, et al. Maintenance of Motivation for Lifestyle Change in Overweight and Obese Adolescents: A 6-Month Follow-Up Study. Curre Res Diabetes & Obes J. 2019; 10(4): 555794. DOI: 10.19080/CRDOJ.2019.10.555794
Abstract
Background: Obesity prevalence has increased significantly in recent decades, affecting millions of children and adolescents worldwide.
Method/Subjects: The present study aimed to evaluate the maintenance of effect of an interdisciplinary intervention group of 12 weeks based on the Transtheoretical Model of Change, on the motivation for behavior modification in overweight and obese adolescents. A total of 135 participants were randomly assigned to a psychoeducational Control Group (CG) or motivational Intervention Group (IG). The dropout rate was of 51.9%.
Results: Evaluation of self-efficacy to keep practicing physical activity and follow a diet in the face of obstacles showed a significant interaction effect for all variables (p <0.05). The IG participants showed a significant improvement over time in the variables of motivation to modify eating habits and practice physical exercise, and self-efficacy and decision-making for weight loss, in comparison to the CG. No significant time or group effect was found for the anthropometric and metabolic variables.
Conclusion: The intervention proved to be highly effective for its main outcome, and could positively enhance long-term changes in anthropometric variables through modification of lifestyle habits.
Keywords: Obesity; Adolescence; Intervention; Follow-up; Transtheoretical model of change; Motivation for change; Anthropometric variables; Physical activity; Psychoeducational control group; Childhood and adolescence; Cardiovascular diseases; Overweight adolescents; Lifestyle change; Healthy eating; Promotion of regular exercise
Abbreviations: CG: Control Group; IG: Intervention Group; CBT: Cognitive-Behavioral Therapy; TTM: Transtheoretical Model; ICF: Informed Consent Form; TTM: Transtheoretical Model; TG: Triglycerides; TC: Total Cholesterol; HDL: High-Density Lipoprotein; LDL: Low-density lipoprotein; GEE Generalized Estimating Equation
Introduction
The prevalence of obesity in childhood and adolescence has risen considerably worldwide, having quadrupled in the last 30 years [1]. This condition poses different health risks to individuals, being associated with chronic diseases such as type 2 diabetes mellitus, alterations in blood pressure and lipid level abnormalities, which are risk factors for the development of cardiovascular diseases [2]. In addition, obesity in this population is related to psychosocial difficulties, such as low self-esteem, greater body dissatisfaction, bullying, and mental health problems [3,4]. Left untreated, overweight adolescents are more likely to become overweight or obese young adults, with difficulties in survival [5-7]. Based on this understanding and an expectation of increasing rates for such conditions, the number of studies focused on possible preventive interventions is increasing.
When considering preventive measures for the development of obesity, various researchers point out that results having a better effect and longer-term maintenance of such are seen in interventions that involve the environment in which the individual is inserted, as well as different areas of knowledge. Therefore, when considering the complexity of obesity treatment in adolescence, the relevance of multi- or interdisciplinary approaches that address concepts of lifestyle change, healthy eating, promotion of regular exercise, and involvement of the parents or guardians of the young people involved is undeniable, as well as addressing their school environment, and adopting effective techniques for the age group [8-11].
Different clinical trials have used the techniques of Cognitive-Behavioral Therapy (CBT) and Motivational Interviewing (MI) as a theoretical basis [12,13] with the purpose of promoting behavioral changes related to a healthy lifestyle. The Basic Attention Notebook nº38 developed by the Brazilian Ministry of Health aims to present strategies for the care and treatment of overweight or obese individuals, and places the Transtheoretical Model (TTM) of change and CBT among the effective interventions [14], corroborating previous studies.
The TTM was developed by authors Prochaska and DiClemente [15] with the objective of explaining the phenomenon of behavioral change, understanding this process as being temporal and involving many dimensions [16]. From this perspective, the TTM has been widely adopted as an approach in weight loss interventions through lifestyle behavioral modifications for the obese adolescent population [17-19].
Follow-up studies are relevant for analyzing the stability and maintenance of intervention results, as well understand the variables that can influence them [20]. Great variability in outcomes has been observed in regards to maintaining the results of interventions. Some studies have found no significant differences between groups in follow-up for most of the variables associated with modification of obesity-related behaviors [21], some have obtained good results in the short-term but these were not maintained [22], while others have found sustained results in the long-term [23,24]. In addition, a high drop-out rate between post-intervention and follow-up evaluations has been observed [22,25,26].
Nonetheless, there remain few studies that report follow-up data after the end of interventions, which suggests the need for future research to analyze the maintenance of the intervention effect [27]. The aim of the present study therefore was to evaluate the follow-up results of a TTM-based interdisciplinary intervention on the motivation for behavioral modification in overweight and obese adolescents, as well as considering the possible maintenance of the outcome.
Methods
Study design and ethical statement
The present study is part of a bigger research, the MERC Program, developed by an interdisciplinary team. The Program protocol, randomization and techniques are published in the Clinical Trials Registry (NCT02455973) and Brazilian Registry of Clinical Trials (RBR-234nb5), and the present follow-up study was approved by the Research Ethics Committee of the Pontifical Catholic University of Rio Grande do Sul (PUCRS) (n°10/834.1) [28]. After verifying the eligibility of study participants, the caregivers and adolescents were read and signed the Informed Consent Form (ICF).
Eligible study participants were randomly allocated to either a Control Group (CG) or Intervention Group (IG). The CG main objective was to conduct educational actions and engage in discussion with the adolescents regarding factors of health promotion, quality of life and risk, while the IG, in addition to this knowledge stimulation on health issues, used a motivational approach and TTM theoretical basis to develop empowerment and autonomy for change in the adolescents. Both interventions were conducted by psychology, physiotherapy, nursing and nutrition professionals and comprised of 12 weekly sessions over a 3-month period. In addition a health education session was directed at the responsible caregivers [28]
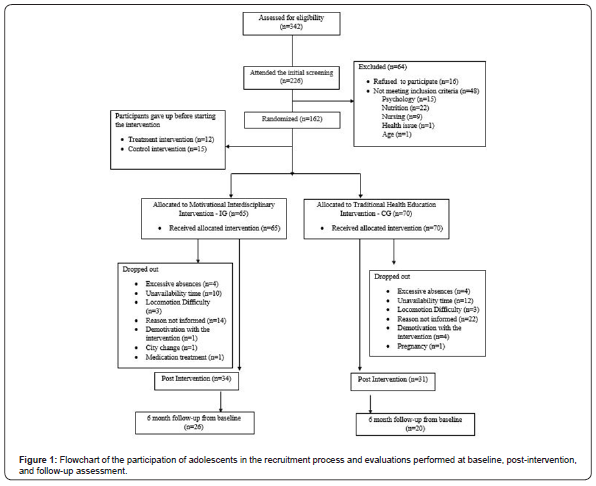
A flowchart showing the participation of adolescents in the recruitment process and evaluations performed at baseline (t0), post-intervention (t1) and follow-up assessment (t2) can be seen in Figure 1.
Measures
Data were collected at three points in time: baseline (t0), post-intervention re-evaluation (t1) and follow-up (t2).
Sociodemographic data questionnaire
A questionnaire was developed to record the sample profile consisting of questions regarding age, gender, race, schooling, employment status, income, and marital status, among others, and issues related to motivation for lifestyle change.
Anthropometric measurements
Anthropometric profile assessment consists of the measurement of body weight, height and waist circumference. Parameters established by the World Health Organization were adopted for the classification of nutritional status [29]. Body weight was measured using a body-weight scale (Cauduro®) with a capacity of 160 kg, duly calibr
ated, with the participant using the minimum of clothing possible. Height was measured using a Sunny® vertical anthropometer. These figures were used to calculate the Body Mass Index (BMI) of each individual, calculated as weight in kilograms divided by height in meters squared².
Lipid and glucose profile evaluation
Analysis of high-density lipoprotein (HDL), total cholesterol (TC), triglycerides (TG) and glucose was performed by enzymatic reactions with the use of Johnson & Johnson kits (Ortho Clinical Diagnostics), dry chemistry methodology and a Vitros 750 Autoanalyzer. Low-density lipoprotein (LDL) was established using the formula LDL = ((TG/5)+HDL) – CT, and insulin resistance (HOMA-IR) by the formula HOMA-IR = fasting glucose x 0.0555 x fasting insulin/22.5.
Psychological and motivational variables
Readiness-to-change scale [30]: An instrument developed to evaluate the readiness of an individual to make changes in their lifestyle, for the behaviors set out in the Brazilian Guidelines for the Treatment of Metabolic Syndrome [31]. It consists of two questions that cover frequency and intensity of physical activity and nine questions involving eating behaviors. The individual responds to each item by placing a point on an analogue scale indicating their readiness to change such behavior at that moment in time.
Exercise self-efficacy scale [32]: This questionnaire comprises of 18 items about situations that could hamper the maintenance of a physical exercise routine, in order to evaluate the strength of an individual’s confidence to overcome the challenges they encounter and to continue exercising. The individual responds on a Likert scale of 0 to 100 for each of the items, and the mean of total scores generates a low, moderate, or high self-efficacy rating for the individual. The Brazilian validation for patients with cardiovascular risk is unifactorial and presents an α = 0.97 (Boff, 2012).
Eating habits self-efficacy scale [32]: A questionnaire composed of 30 items about situations that could hinder the continuance of a healthy eating routine, which aims to evaluate the strength of an individual’s confidence to overcome challenges encountered and maintain a diet. The items are answered on a Likert scale of 0 to 100, and the mean of the total scores generates a classification of low, moderate, or high self-efficacy. The Brazilian validation for patients with cardiovascular risk presented 3 factors: Social Situations (EHSS) (α = 0.93), Physical and Emotional States (EHPES) (α = 0.91) and Generates Craving (EHGC) (α=0.88) [33].
Decisional balance for weight loss [34]: A self-report instrument aimed at evaluating how important the aspects are that influence decision-making for weight loss. Composed of 20 items, responses are given using a Likert scale of 1 to 5. The total score obtained represents the importance of the pros and cons in making the decision to lose weight.
Statistical analysis
Quantitative variables are described by mean and standard deviation or standard error, and qualitative variables by absolute and relative frequencies. Student’s t-test and the Mann Whitney test were used to evaluate the homogeneity of groups at baseline. The comparison between groups at baseline considered the assumption of intention to treat, and a total of 135 participants were included in the analyses performed. Student’s t-tests for independent samples and the Mann Whitney U test were used to compare the continuous variables. Pearson’s Chi-Square test and Fisher’s exact test were used for the categorical variables.
The Generalized Estimating Equation (GEE) was used for analysis of variables over time [35,36] Repeated measures were obtained from follow-up evaluations (baseline, 3 and 6 months). A linear model was applied for variables with a normal distribution and gamma model for those with asymmetric distribution. The significance level adopted was 5% (p <0.05) and the analyses were performed using the Windows software SPSS v23.
Results
Study population
As presented in the Figure 1 flowchart, 135 participants were initially included in the intervention following the first evaluation, of which, 65 completed the program of twelve sessions over three months, a loss of 70 individuals (51.9% of the sample). At the end of this period all participants were instructed to re-attend PUCRS after three months for a postintervention reassessment process. Of those participants who completed the intervention, contact was established and a follow-up evaluation completed for 46 of them, with a further loss of 19 individuals (29.2%). No statistically significant difference was found in the comparison between the groups for the follow-up evaluation (p = 0.351). It is important to point out that from the total sample loss, 50 participants belonged to the CG, and 26 to the IG, suggesting a significantly lower loss in the motivational intervention group.
The predominant nutritional diagnosis in the study sample of 135 adolescents (mean age 16.4 ± 1.09 years; 100 female (74.1%), 35 male (25.9%)) was obesity (84.4%). The ethnic background of the sample was mainly white (69.6%), brown or mulatto (15.6%), Afro-descendant (11.1%), and the minority group Asian or indigenous (2.2%). The predominant socioeconomic level according to the Brazilian socioeconomic classification was class B (51.1%), and 63% of participants had completed or were still in high school at the time of evaluation.
Evaluation results
Table 1 presents the results of the anthropometric, metabolic and psychological variables of the study evaluations, discussed in the text throughout the article.
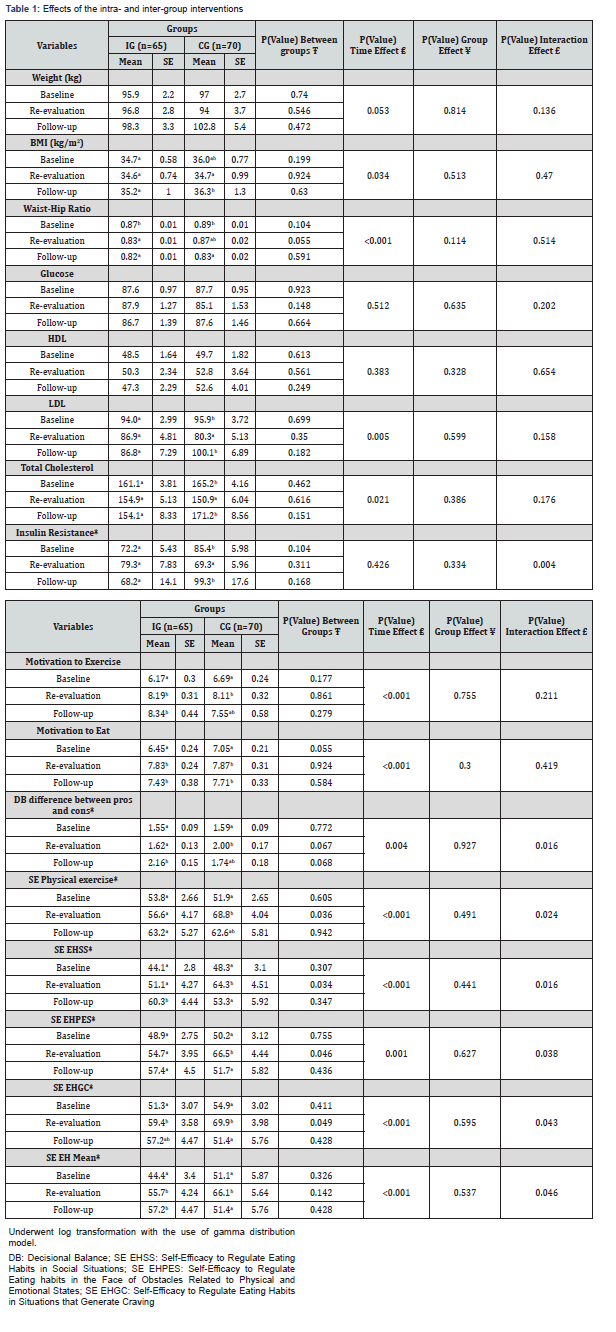
Anthropometric and metabolic results
No significant interaction effect was observed when evaluating the anthropometric variables, demonstrating the behavior of both groups to be similar throughout the follow-up. However, some significant time effects can be seen. Considering BMI (p = 0.034), no significant change over time was found in the IG, whereas there was a significant increase from t1 to t2 in the CG, while remaining stable in the IG. In relation to waisthip ratio (p <0.001), the IG showed a significant reduction at the revaluation point and this was maintained at t2, while the reduction in the CG was only significant at t2.
When analyzing the metabolic variables, a significant time group interaction effect was found for fasting insulin (p = 0.015) and insulin resistance (p = 0.004). No significant change over the course of the follow-up was observed for these two variables in the IG, however, in the CG a significant reduction was seen when re-evaluated at the end of the intervention, which increased significantly at follow-up, returning to baseline levels. No significant interaction effect between group and time was apparent for the other variables. However, there was an isolated time effect for LDL (p = 0.005) and total cholesterol (p = 0.021). For both variables, no significant change was found in the IG over the follow-up and a significant reduction occurred in the CG at re-evaluation, returning to baseline levels by t2.
Results of psychological variables
No statistically significant interaction effect was found when examining the motivational scales for improving eating habits and physical exercise, however, there was an isolated time effect (p <0.001). There was a significant increase in motivation in both groups for these behavioral changes at t1, and maintained at t2. When evaluating the decisional scale to lose weight or not, an interaction effect was observed between group and time (p = 0.016); there was a significant increase for the IG at t2, and for the CG at t1.
Evaluation of self-efficacy to keep practicing physical activity and follow a diet in the face of obstacles showed a significant interaction effect for all variables (p <0.05). No significant change for physical exercise was seen in the follow-up for the IG, while there was a significant increase in the CG at t1. For the selfefficacy to regulate eating habits in social situations (EHSS), the IG presented a significant increase at t2, while the CG presented a significant increase at t1, but returning to baseline levels at follow-up.
When assessing self-efficacy to regulate eating habits in the face of obstacles related to physical and emotional states (EHPES), no significant change was noted throughout the follow-up for the IG, whereas there was a significant increase in the CG at t1, which decreased to baseline levels at t2. In both groups, there was a significant increase at the reevaluation in the self-efficacy variable regulating eating habits in situations that generate craving (EHGC); however, there was a significant reduction in the CG at t2. In the general evaluation regarding the ability of the adolescents to stay on a diet (EH mean), there was a significant increase in the IG at t1 that was maintained at t2, while a significant increase occurred in the CG at t1 only.
Discussion
The application of the MERC Program had statistically significant results linked to the dimensions that make up behavioral change according to the TTM, in that the adolescents showed great advances in psychological variables, which are considered the most relevant for long-term improvement and are the desired primary outcome in the present study. The main result of this study pertains to variables related to motivation for behavioral change. Motivation is seen as a necessary first step towards this change [37-39] and studies indicate this concept as being an important predictor of long-term practice of physical exercise [40,41].
In terms of motivation for behavioral change, a growing rise in motivation rates to increase the practice of exercise was observed in both groups and an improvement in eating habits over time. However, the IG mean scores maintained constant growth in the Motivation Scales pertaining to change, suggesting that the intervention was effective in stimulating intrinsic motivators, with these being the personal internal factors of the individual. Based on the MERC Program proposal to focus on motivation and understanding that such a variable defines behavioral change in the long-term, the results suggest the IG participants are more motivated and have progressed further in the stages of readiness for change.
In relation to the decision-making process for weight loss, the MERC Program presented significant interaction results between group and time, in a way that IG participants showed continuous growth in the evaluation of importance of actually losing weight, observing more harm than benefits in staying as they were (2.16), in relation to the CG (1.74). The TTM points to the Decisional Scale as one of the main conduits for behavioral change, since it can aid in the resolution of healthrelated problems through conscious decision-making [19,42]. Therefore, the MERC program proved to be effective in its goal of evoking intrinsic motivators for adolescents to evaluate the advantages and disadvantages, which are the most relevant for the maintenance of decision-making.
In a similar way, it is known that confidence in one’s own ability to perform an action, which is one of the main mechanisms for executing change, plays an essential role in maintaining diets and regular physical activity [43], with this being one of the main constructs addressed in the MERC Program. In the present study, the IG participants presented continuous growth in perception of self-efficacy to keep practicing physical exercise, from baseline to t2, a result not observed in the CG. A significant improvement was also seen in the IG adolescents for self-efficacy to regulate eating habits in the face of obstacles related to social situations, and physical and emotional states, as well as situations that can generate cravings. Increased growth in self-efficacy is an important predictor and mediator of success for weight control, regular physical exercise and long-term eating habits [40,44], and therefore, it is our understanding that the intervention in the present study achieved important success in the goal of preparing the adolescents to face these future obstacles [45-48].
Due to the developmental stage of the participants and to previous reviews [49,50], the improvement in anthropometric and metabolic variables were considered a secondary outcome of the MERC Program. Analysis of the anthropometric variables showed an increase in weight and BMI, and decrease in the Waist-Hip Ratio over time in both groups. Even if modifications to regulate eating habits and physical activity have been addressed in the MERC Program, the evidence suggests the adaptation of intervention regarding factors that prevent weight gain, such as homeostatic, environmental and behavioral processes [51]. Similarly, the metabolic variables did not present improvements, bearing in mind that a series of different variables can influence and have an impact on these results, which were not controlled in the program.
Conclusion
The present study aimed to evaluate the maintenance of behavioral changes related to lifestyle improvement in overweight and obese adolescents, from a comparison between a TTM-based health intervention with a motivational (IG) and psychoeducational (GC) approach. The intervention proved to be effective in relation to its main outcome, namely, the motivation variables for change of eating habits and the practice of exercise, in the evaluation of decision-making for weight loss and in self-efficacy. In addition, it is important to highlight the greater adherence of the adolescents participating in the motivational intervention, which suggests they have a higher level of motivation, a significant factor for subsequent modifications in habit for a healthy lifestyle.
Among the initial limitations of the present study is the development of the interventions, which had many similarities in their approach, suggesting a possible methodological reformulation of the Waiting List + IG to better verify possible intervening variables [51,52-54]. Furthermore, the groups being conducted by different therapists could be a bias on the outcome.
Another possible drawback could be in only having a 12-week intervention in the view of much of the research [10,39,46,50,55,56] and the limited number of sessions with the parents. The impact of parental modeling on child and adolescent learning Armitage et al. [46] considers the need to conduct an intervention that includes greater contact with those adults responsible for the parental care of participants [57-59].
Evaluations for the measurement of food intake modifications and for the practice of physical exercise have not yet been performed. Therefore, it is concluded that future researches for the program should include indicators of diet quality and a cardiorespiratory capacity test to establish a correlation of the data.
Even though the anthropometric and metabolic variables were not the desired outcome of the intervention in the present study, an evaluation of the effectiveness of the strategies and skills covered in the MERC Program should be carried out in order to improve the program.
Sources of Funding
This study was made financially possible by the Brazilian government through the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) with Universal Edits 483257/2013-3 and Universal 455106/2014. It also had financing from the Infrastructure Publication of PUCRS/PRAIAS (01/2014).
Disclosure of Potential Conflicts
There are no potential conflicts, real or perceived, for any of the named authors while contributing and producing this study.
Clinical Trials Registry Site and Number
MERC is a randomized clinical trial (RCT) carried out in southern Brazil, with approval of the Committee of Ethics in Research of the Pontifical Catholic University of Rio Grande do Sul (CAAE: 36209814.6.0000.5336). The study protocol is registered with the Brazilian Registry of Clinical Trials (RBR- 234nb5) and the Clinical Trial Registry (NTC02455973)
References
- (2018) Obesity and overweight. World Health Organization.
- Craig LCA, Love J (2008) Overweight and Cardiovascular Risk Factors in 4- to 18-Year-Olds. Obes Facts 1(5): 237-242.
- Gibson LY, Allen KL, Davis E, Blair E, Zubrick SR, et al. (2017) The psychosocial burden of childhood overweight and obesity: evidence for persisting difficulties in boys and girls. Eur J Pediatr 176(7): 925-933.
- Yen CF, Liu TL, Ko CH, Wu YY, Cheng CP (2014) Mediating effects of bullying involvement on the relationship of body mass index with social phobia, depression, suicidality, and self-esteem and sex differences in adolescents in Taiwan. Child Abus Negl 38(3): 517-526.
- Lee H, Pantazis A, Cheng P, Dennisuk L, Clarke PJ, et al. (2016) The Association Between Adolescent Obesity and Disability Incidence in Young Adulthood. J Adolesc Heal 59(4): 472-478.
- Simmonds M, Llewellyn A, Owen CG, Woolacott N (2016) Predicting adult obesity from childhood obesity : a systematic review and meta-analysis. Obes Rev 17(2): 95-107.
- Singh AS, Mulder C, Twisk JWR, Mechelen W Van, Chinapaw MJM (2008) Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev 9(5): 474-488.
- Nixon CA, Moore HJ, Douthwaite W, Gibson EL, Vogele C, et al. (2012) Identifying effective behavioural models and behaviour change strategies underpinning preschool- and school-based obesity prevention interventions aimed at 4 – 6-year-olds : A systematic review. Obes Rev 13(1): 106-117.
- Wang Y, Wu Y, Wilson R (2013) Childhood Obesity Prevention Programs : Comparative Effectiveness Review and Meta-Analysis.
- Boff RM, Liboni RPA, Batista IP de A, de Souza LH, Oliveira M da S (2017) Weight loss interventions for overweight and obese adolescents: a systematic review. Eat Weight Disord 22(2): 211-229.
- Lobstein T, Jackson-Leach R, Moodie ML, Hall KD, Gortmaker SL, et al. (2015) Obesity 4 Child and adolescent obesity: part of a bigger picture. Lancet 385(9986): 2510-2520.
- Boff RM, Liboni RPA, Batista IP de A, de Souza LH, Oliveira M da S (2017) Weight loss interventions for overweight and obese adolescents: a systematic review. Eat Weight Disord 22(2): 211-229.
- Tsiros MD, Sinn N, Brennan L, Coates AM, Walkley JW, et al. (2008) Cognitive behavioral therapy improves diet and body composition in overweight and obese adolescents. Am J Clin Nutr 87(5): 1134-1140.
- (2014) Ministério da Saú Cadernos de Atenção Básica.
- Prochaska JO, DiClemente CC (1983) Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol 51(3): 390-395.
- Prochaska JO, DiClemente CC, Norcross JC (1992) In search of how people change. Applications to addictive behaviors. Am Psychol 47(9): 1102-1114.
- Han H, Gabriel KP, Kohl HW (2015) Evaluations of Validity and Reliability of a Transtheoretical Model for Sedentary Behavior among College Students. Am J Health Behav 39(5): 601-609.
- Pirzadeh A, Feizi A, Ghofranipour F, Mostafavi F (2015) Improving physical activity and metabolic syndrome indicators in women: A transtheoretical model-based intervention. Int J Prev Med 6(1): 28.
- Prochaska JO, Norcross JC, Fowler JL, Follick MJ, Abrams DB (1992) Attendance and outcome in a work site weight control program: processes and stages of change as process and predictor variables. Addict Behav 17(1): 35-45.
- Breakwell Glynis M, Hammond Sean, Fife-Schaw, Chris Smith JA (2010) Research methods in psychology. (3rd edn,). Sage Publications, pp. 524.
- Neumark-Sztainer D, Story M, Hannan PJ, Rex J (2017) New Moves: a school-based obesity prevention program for adolescent girls. Prev Med 37(1): 41-51.
- Rohm I, Schaarschmidt M, Figulla HR, Lichtenauer M, Goebel B, et al. (2014) Effect of a weight loss program in obese adolescents; a long-term follow-up. Nutr Hosp 30(2): 367-374.
- Lloyd-Richardson EE, Jelalian E, Sato AF, Hart CN, Mehlenbeck R, et al. (2012) Two-Year Follow-up of an Adolescent Behavioral Weight Control Intervention. Pediatrics 130(2): 281-288.
- Reinehr T, Temmesfeld M, Kersting M, de Sousa G, Toschke AM (2007) Four-year follow-up of children and adolescents participating in an obesity intervention program. Int J Obes 31(7): 1074-1077.
- Adam S, Westenhoefer J, Rudolphi B, Kraaibeek HK (2013) Three- and five-year follow-up of a combined inpatient-outpatient treatment of obese children and adolescents. Int J Pediatr 2013: 856743.
- Zambon MP, Ângela M, Antonio RGM, Mendes RT, De Azevedo A (2008) Crianças e adolescentes obesos: dois anos de acompanhamento interdisciplinar.
- Waters E, de Silva-Sanigorski A, Hall BJ, Brown T, Campbell KJ, et al. (2011) Interventions for preventing obesity in children. Cochrane database Syst Rev (12): CD001871.
- Ribeiro FA, Boff RM, Feoli AMP, Gustavo AS, Donadio MVF (2016) Randomized clinical trial of a motivational interdisciplinary intervention based on the transtheoretical model of change for lifestyle modification in overweight/obese adolescents: MERC study protocol. Int J Clin Trials 3(4): 225.
- (2006) The World Health Report 2006 - working together for health. (1st edn,). World Health Organization. Geneva, UK.
- Velasquez MM, Maurer GG, Crouch C, DiClemente CC (2001) Group treatment for substance abuse: A stages-of-change therapy manual. Group treatment for substance abuse: A stages-of-change therapy manual.
- (2010) Associação Brasileira para o Estudo da Obesidade e da Síndrome Metabó Diretrizes Brasileiras Da Obesidade 2009/2010.
- Bandura A (2006) Self-efficacy beliefs of adolescents. In: Pajares F, Urdan T, (Edt,). Guide for Constructing Self-Efficacy Scales. Information Age Publishing, pp. 307-337.
- Boff RM (2012) Evidências Psicométricas das Escalas de Auto-Eficácia para Regular Hábito Alimentar e Auto-Eficácia para Regular Exercício Fís Pontifícia Universidade Católica do Rio Grande do Sul.
- Prochaska JO, Velicer WF, Rossi JS, Goldstein MG, Marcus BH, et al. (1994) Stages of Change and Decisional Balance for 12 Problem Behaviors. Health Psychol 13(1): 39-46.
- Costa PR de F, Assis AMO, Silva M da CM, Santana MLP, Dias JC (2009) Mudança nos parâmetros antropométricos : A influência de um programa de intervenção nutricional e exercício físico em mulheres adultas. Cad Saúde Pública 25(8): 1763-1773.
- Guimarães L, Hirakata V (2012) Uso do Modelo de Equações de Estimações Generalizadas na análise de dados longitudinais. Rev HCPA 32(4): 503-511.
- Deci EL, Ryan RM (2000) The “What” and “Why” of Goal Pursuits: Human Needs and the Self-Determination of Behavior. Psychol Inq 11(4): 227-268.
- Reinehr T (2011) Symposium III: Metabolic health, weight management and obesity prevention in childhood and adolescence Effectiveness of lifestyle intervention in overweight children. Proc Nutr Soc 70: 494-505.
- Ryan RM, Deci E (2006) Self-Regulation and the Problem of Human Autonomy : Does Psychology Need Choice, self-determination, and will? J Pers 74(6): 1557-1585.
- Teixeira PJ, Carraça EV, Marques MM, Rutter H, Oppert JM, et al. (2015) Successful behaviour change in obesity interventions in adults: a systematic review of self-regulation mediators. BMC Med 13: 84.
- Young MD, Plotnikoff RC, Collins CE, Callister R, Morgan PJ (2015) Impact of a male-only weight loss maintenance programme on social-cognitive determinants of physical activity and healthy eating: A randomized controlled trial. Br J Health Psychol 20(4): 724-744.
- Prochaska JO, DiClemente CC, Velicer WF, Ginpil S, Norcross JC (1985) Predicting change in smoking status for self-changers. Addict Behav 10(4): 395-406.
- Ferreira MSG, Bakos DS, Habigzang LF (2015) A influência das crenças de autoeficácia na manutenção do emagrecimento. Aletheia 46: 202-210.
- Kelly S, Stephens J, Hoying J, McGovern C, Melnyk BM, et al. (2017) A systematic review of mediators of physical activity, nutrition, and screen time in adolescents: Implications for future research and clinical practice. Nurs Outlook 65(5): 530-548.
- Parkinson J, David P, Rundle-Thiele S (2017) Self-efficacy or perceived behavioural control: Which influences consumers’ physical activity and healthful eating behaviour maintenance? J Consum Behav 16(5): 413-423.
- Armitage CJ, Wright CL, Parfitt G, Pegington M, Donnelly LS, et al. (2014) Self-efficacy for temptations is a better predictor of weight loss than motivation and global self-efficacy: Evidence from two prospective studies among overweight/obese women at high risk of breast cancer. Patient Educ Couns 95(2): 254-258.
- Burke LE, Ewing LJ, Ye L, Styn M, Zheng Y, et al. (2015) The SELF trial: A self-efficacy-based behavioral intervention trial for weight loss maintenance. Obesity 23(11): 2175-2182.
- Choo J, Kang H (2015) Predictors of initial weight loss among women with abdominal obesity: A path model using self-efficacy and health-promoting behaviour. J Adv Nurs 71(5): 1087-1097.
- Al-Khudairy L, Loveman E, Colquitt JL, Mead E, Johnson RE, et al. (2017) Diet, physical activity and behavioural interventions for the treatment of overweight or obese adolescents aged 12 to 17 years. Cochrane Database Syst Rev 6: CD012691.
- Rancourt D, Thurston IB, Sonneville KR, Milliren CE, Richmond TK (2017) Longitudinal impact of weight misperception and intent to change weight on body mass index of adolescents and young adults with overweight or obesity. Eat Behav 27: 7-13.
- Greenway FL (2015) Physiological adaptations to weight loss and factors favouring weight regain. Int J Obes 39(8): 1188-1196.
- Berkowitz RI, Rukstalis MR, Bishop-Gilyard CT, Moore RH, Gehrman CA, et al. (2013) Treatment of Adolescent Obesity Comparing Self-Guided and Group Lifestyle Modification Programs: A Potential Model for Primary Care. J Pediatr Psychol 38(9): 978-986.
- Naar-King S, Ellis D, Kolmodin K, Cunningham P, Jen KLC, et al. (2009) A Randomized Pilot Study of Multisystemic Therapy Targeting Obesity in African-American Adolescents. J Adolesc Heal 45(4): 417-419.
- Nguyen B, Shrewsbury V, O ’Connor J, Steinbeck K, Hill A, et al. (2013) Two-year outcomes of an adjunctive telephone coaching and electronic contact intervention for adolescent weight-loss maintenance: the Loozit randomized controlled trial. Int J Obes 37(3): 468-472.
- Walpole B, Dettmer E, Morrongiello BA, McCrindle BW, Hamilton J (2013) Motivational Interviewing to Enhance Self-Efficacy and Promote Weight Loss in Overweight and Obese Adolescents: A Randomized Controlled Trial. J Pediatr Psychol 38(9): 944-953.
- Carvalho M, Menezes D, Aparecida S, Silva C, Deus R De, et al. (2015) Intervention based on Transtheoretical Model promotes anthropometric and nutritional improvements - A randomized controlled trial. Eat Behav 17: 37-44.
- Marchesini G, Montesi L, El Ghoch M, Brodosi L, Calugi S (2016) Long-term weight loss maintenance for obesity: a multidisciplinary approach. Diabetes Metab Syndr Obes 9: 37-46.
- Berge JM, Everts JC (2011) Family-Based Interventions Targeting Childhood Obesity: A Meta-Analysis. Child Obes 7(2): 110-121.
- Quattrin T, Roemmich JN, Paluch R, Yu J, Epstein LH, et al. (2014) Treatment Outcomes of Overweight Children and Parents in the Medical Home. Pediatrics 134(2): 290- 297.






























