Insidious Occurrence of Erythema Annulare Centrifugum in Non-Insulin Dependent Diabetes Mellitus (NIDDM) Type-2 /Adult Onset Diabetes Mellitus: An Intractable Bizarre Cutaneous Manifestations
Virendra N Sehgal1* and Sonal Sharma2
1 Dermato-Venereology (Skin/VD) Center, Sehgal Nursing Home, India
2Department of Pathology, University College of Medical Sciences and Associated Guru Teg Bahadur Hospital, India
Submission: November 20, 2018; Published: February 06, 2019
*Corresponding author: Virendra N Sehgal, Dermato Venerology (Skin/VD) Centre Sehgal Nursing Home, A/6 Panchwati, Delhi-110 033, India
How to cite this article: Virendra N S, Sonal S. Insidious Occurrence of Erythema Annulare Centrifugum in Non-Insulin Dependent Diabetes Mellitus (NIDDM) Type-2 /Adult Onset Diabetes Mellitus: An Intractable Bizarre Cutaneous Manifestations. Curre Res Diabetes & Obes J. 2019; 9(5): 555771. DOI: 10.19080/CRDOJ.2019.09.555771
Abstract
Erythema annulare centrifigum emphasizing the role of beta cell of head of pancreas in its plausible causation is describe, the features of which conformed to non-insulin dependent diabetes mellitus type 2.
Keywords:Erythema annulare centrifigum; Polyglandular autoimmune syndrome; Diabetes mellitus; Finasteride; Cancer; Graves disease; Endocrine functions; Fasting blood sugar; Epidermis; Dermis
Abbreviations: APECED: Autoimmune Polyendocrinopathy-Candidiasis-Ectodermal Dystrophy; Hb: Hemoglobin; EAC: Erythema Annulare Centrifugum; H&E: Hematoxylin and Eosin; SR: Sustained-Release; NIDDM: Non- Insulin Dependent Diabetes Mellitus; ACTH: Adrenal Function Test; PTH: Parathyroid Hormone; PSA: Prostate Specific Antigen; TSH: Thyroid Simulating Hormones
Introduction
Erythema annulare centrifigum [1,2] is an intriguing entity right from the word go. Its origin is largely elusive. Nevertheless, it has been incriminated as a skin marker in variety of systemic disorders including food, contact dermatitis fungal, bacterial and viral infections, drugs including finasteride, cancer, graves disease, appendicitis, lupus, pregnancy, hormone and lyme disease it may be a cutaneous manifestation extraordinary of an autoimmune systemic disorder [3], polyglandular autoimmune syndrome type 1 is one of them. Its insidious occurrence in NIDDM (type- 2) adult onset diabetes mellitus is unique and thus far unreported entity hence the current report.
Case-Report
A 49-years-old man had asymptomatic, spontaneous episode of erythema to scaly round eruptions affecting the trunks and extremities marked by remissions and recurrences ever since. Their innocuous nature hardly warranted any attention. Accordingly, the condition eluded diagnosis. Nevertheless, the frequency of recurrence of the episode continued over the years forcing the patient to seek medical advice time and again. He was erroneously treated for superficial fungal infection, without any tangible results. The ups and downs in the clinical condition continued unabated.
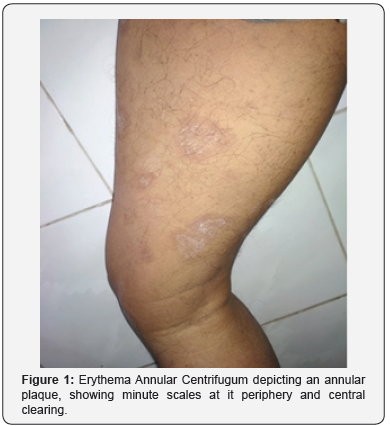
Ultimately, in the course of medical checkup for life insurance in the year 2016 he was found to be suffering from non- insulin dependent diabetes mellitus (NIDDM) type- 2. The fasting blood sugar was 213 (70 to 100 mg/dl), post-parandial 403 mg/dl (less than 140 mg/dl) and Glycosylated hemoglobin (hbA1c) 9.2 % (4% to 5.6%). Besides, endocrine functions of adrenal glands, parathyroid glands prostate gland (Table 1), testes and thyroid gland were under taken to take stock of the endocrine glands. He was also subjected to skin biopsy from the representative lesions for histopathological examination to form the precise diagnosis. He is now being administered Glycomet (metformin) SR (Sustained-release) 500mg half an hour prior to lunch and dinner along with pioz (pioglitazone) 15 once a day in the morning on regular daily treatment for NIDDM.
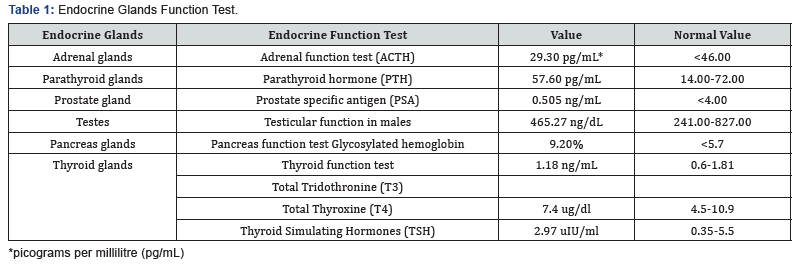
Examination of the skin surface revealed and erythema to scaly, plaque of annular configuration erythema and scales were minute confined to the periphery of the annular lesion, central clearing was characteristics (Figure 1). The lesions were bizarre and multiple distributed on the neck, upper and lower extremities and trunk. They were bilateral and asymmetrical.
Histopathology
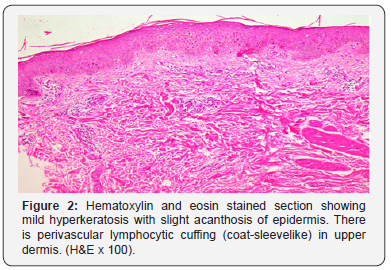
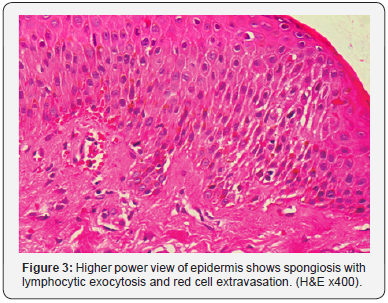
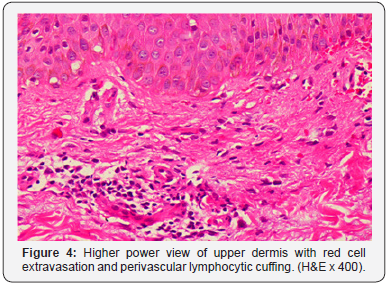
Hematoxylin and eosin (H&E) stained section(s) showed changes both in epidermis and dermis. The epidermal changes were apparent in the form of mild hyperkeratosis and acanthosis while the dermal changes were marked by focal spongiosis, lymphocytic and red cell around the blood vessel in the upper dermis exocytosis depicting pattern simulating coat sleeve (Figures 2-4). Red cells extravasation and perivascular lymphocytic infiltrate were also seen upper dermal vessels.
Discussion
Erythema annulare centrifugum (EAC), an excellent descriptive nomenclature, recognize for the first time by Darier1 as far back as 1916, characterized by a scaling or non-scaling, non-pruritic, annular or arcuate, erythematous eruption. It tends to spread peripherally while clearing centrally. It is an intractable, bizarre an rare condition invariably a part component of underlying systemic disease, NIDDM (type-2) adult onset diabetes mellitus, later being an autoimmune disease 2,3 in the case study under review. The concomitance of EAC and NIDDM type 2 is an overture extraordinary/innovation. However, it is imperative to perform histopathology to supplement the clinical diagnosis [4-6]. EAC histopathology has features such as; mound-like parakeratosis, focal spongiosis and /or edema of papillary dermis [4]. It is an extraordinary symptom complex, seemingly a part component of a dispensation, multiple/ overlap autoimmune syndrome [7,8] warranting evaluation of thyroid and para thyroid gland, adrenal cortex, male gonad and pancreas through endocrine function test.
This aspect in particular was worked up in the case under review. Interestingly, the endocrine function test in all the endocrine glands were found to be within normal limits, except for that of pancreas; glycocylated hemoglobin (HbA1c) was found to be fairly high in contrast to that of normal. This particular aspect was taken cognizance of revealing high blood sugar level from time to time supplemented by high glycosylated hemoglobin level, indicating absolute implication of beta cells of pancreas thus reducing the release the quantum of insulin in the blood in response to rising glucose in the bloodstream in consequence to consumption of carbohydrates [9] (glucogenesis) and / or fat and proteins [10] (gluconeogenesis). Insulin is released from the beta cells in pancreas in response to rising glucose in bloodstream. After eat a meal, any carbohydrates eaten are broken down into glucose and passed into the bloodstream. The pancreas detects this rise in blood glucose and starts to secrete insulin, the sequence conforming to NIDDM type-2 [11] / adult onset diabetes mellitus [12,13].
Besides, polyglandular autoimmune syndrome should also be considered in differential diagnosis. polyglandular autoimmune syndrome type 1 being colossal sporadic disorder. It is therefore worthwhile to recall the salient feature of this sparingly reported syndrome to create a focus attention of the audience. It is usually presenting in childhood and is characterized by autoimmune destruction of several glands including the parathyroid glands, adrenal cortex, gonads, pancreatic β cells, gastric parietal cells, and the thyroid gland [14]. Autoimmune polyendocrinopathycandidiasis- ectodermal dystrophy (APECED) is an autosomalrecessive syndrome that causes polyglandular failure syndrome type 1. Implication of endocrine gland following to autoimmune phenomenon is vital and is required to be thoroughly investigated, especially laying emphasis on endocrine functions.
Diabetic dermopathy, necrobiosis lipoidica diabeticorum, diabetic bullae (bullosis diabeticorum), certain acquired perforating dermatoses, diabetic thick skin, scleredema adultorum, Dupuytren’s contractures, certain xanthomas, carotenoderma, rubeosis faciei, and acanthosis nigricans are a few of the other NIDDM related dermatoses [15].
References
- J Darier (1916-1917) De l’érythème annulaire centrifuge (érythème papulo-circineé migrateuse et chronique) et de quelques éruptions analogues. Annales de dermatologie et de syphilographie 5: 57-58.
- Garty B (1998) Erythema annulare centrifugum in a patient with polyglandular autoimmune disease type 1. Cutis 62(5): 231-232.
- Pouran Layegh, M Abadian, N Zabolinejhad, Seyed Reza Mousavi (2013) Erythema annulare centrifugum: Association with autoimmune polyglandular syndrome type 1. Iranian Journal of Dermatology 16(64): 73-76.
- Kim KJ, Chang SE, Choi JH, Sung KJ, Moon KC, et al. (2002) Clinicopathologic analysis of 66 cases of erythema annulare centrifugum. J Dermatol 29(2): 61-67.
- Weyers W, Diaz-Cascajo C, Weyers I (2003) Erythema annulare centrifugum: results of a clinicopathologic study of 73 patients. Am J Dermatopathol 25(6): 451-462.
- Launay P, Blanc D, Paris B, Quencez E, Drobacheff C, et al. (1988) Erythema annulare centrifugum disclosing hyperthyroidism. Ann Dermatol Venereol 115(6-7): 721-723.
- Humbert P, Dupond JL (1988) Multiple autoimmune syndromes. Ann Med Interne (Paris)139(3): 159-168.
- Sehgal VN, Malhotra R (2018) Multiple /Overlap Autoimmune Syndrome: An overlap of Systemic Lupus Erythematosus, Dermato-Polymyositis and Non-Insulin Dependent / Adult Onset Diabetes Mellitus Concomitant Herpes (Varicella) Zoster /Shingles, an innovation. Journal of Dermatitis.
- (2009) Glycogenesis.
- Silva Pedro (2009) The Chemical Logic Behind Gluconeogenesis.
- Velloso LA, Eizirik DL, Cnop M (2013) Type 2 diabetes mellitus-an autoimmune disease? Nat Rev Endocrinol 9(12): 750-755.
- (2013) Diabetes Fact sheet N°312". WHO.
- (2014) About diabetes. World Health Organization.
- Guo CJ, Leung PSC, Zhang W, Ma X, Eric Gershwin M (2017) The Immunobiology and clinical features of type 1 autoimmune polyglandular syndrome (APS-1). Autoimmun Rev 17(1): 78-85.
- Sehgal VN, Srivastava G, Aggarwal AK, Gupta M, Bhattacharya SN, et al. (2011) Noninsulin-dependent, type II diabetes mellitus-related dermatoses: part II. Skinmed 9(5): 302-308.






























