Evaluation of Dietary Habits Effect among Saudi Patients with Type II Diabetes Mellitus
Saja Al Omiri and Amani A Alrasheedi*
Food and Nutrition Department, King Abdul Aziz University, Saudi Arabia
Submission: February 26, 2018; Published: March 28, 2018
*Corresponding author: Amani A Alrasheedi, Nutrition and Food Science, Food and Nutrition- Home Economics, King Abdul Aziz University, PO Box 18886, Jeddah 21425, Saudi Arabia, Email: aalrasheedi@kau.edu.sa
How to cite this article: Saja A O, Amani A A. Evaluation of Dietary Habits Effect among Saudi Patients with Type II Diabetes Mellitus. Curre Res Diabetes & Obes J. 2018; 6(4): 555695. DOI: 10.19080/CRDOJ.2018.06.555695.
Abstract
Improving the dietary habits of type two diabetes mellitus patients could decrease the disease complications.
Aim:This study aimed to evaluate the effect of dietary habits of a sample of Saudi patients on type two diabetes mellitus.
Methodology:cross-sectional study was carried out on 200 patients (100 male and 100 female) using the first item of the validated version of Personal Diabetes Questionnaire (PDQ).
Results:most of the study participants (73.5%) were up to 50 years old and (87%) were obese or overweight. Half of the study participants (50%) had a good level of diet knowledge and skills, only (6%) of them taken the good decision, (62%) taken a fair decision. Most of the study participants (71.0%) did not have any eating problems or diet barriers (47.5%).
Conclusion: modifying lifestyle of T2DM patients and controlling weight control help to reduce the national burden of this disease and improving the health for T2DM patient.
Keywords: Diabetes mellitus; Dietary habits; Personal diabetes questionnaire
Abbrevations: DM: Diabetes Mellitus; T2DM: Type Two Diabetes Mellitus; KAUH: King AbdulAziz University Hospital; PDQ: Personal Diabetes Questionnaire; HbA1C: Glycosylated Hemoglobin; BMI: Body Mass Index; SPSS: Statistical Package for Social Science
Introduction
Diabetes mellitus (DM) is one of the most important global health problems growing swiftly. The international diabetes federation estimated that 382 million people have diabetes worldwide and 3.8 million in Saudi Arabia in 2014 [1].
Type II DM has a complex etiology associated with irreversible risk factors that includes age, ethnicity, race and genetics; as well as reversible risk factors including diet, smoking and physical activity. The major factors that contribute to the rapidly rising incidence of DM in developing countries are dietary habits and sedentary lifestyles [2]. T2DM has several consequences, associated with increased risks of hypertension, premature atherosclerosis, retinopathy, renal failure, neuropathic diseases [3] and cardiovascular diseases [4,5].
The gulf area experienced a dramatic change during the past four decades pertaining the living conditions that resulted in an unhealthy obesogenic environment and physical inactivity [6,7]. These new nutritional habits are owned to the proliferation of westernized life style and food [8,9] therefore dietary management and food choices are unsatisfactory [10,11]. The T2DM management requires lifestyle interventions that are specifically designed to influence the individual’s food intake and physical activity [12,13]. All individuals should receive a standard diabetes education that specifically focuses on dietary interventions with increasing the physical activities valuable importance. Moreover, promoting a therapeutic lifestyle is fundamental at the diagnosis stage; periodic counseling should be integrated into the treatment program. Improving glycemic control and other cardiovascular risk factors through weight reduction attained by either dietary means alone or with adjunctive medical or surgical intervention. The individuals physical activity should be encouraged to ideally aim for at least 150min/week of moderate intensity that include flexibility, aerobic and resistance training [14]. The study aims to evaluate a sample of Saudi national patient’s dietary habits of both genders with type II diabetes mellitus in Jeddah, Saudi Arabia.
Study Methodology
It was a cross-sectional study carried out in the department of internal medicine-King Abdulaziz University Hospital (KAUH) for a period of two months from September through October 2016. Ethical approval was obtained from Research Ethics Committee of Biomedical Ethics, in addition to Research Ethic committee of KAU faculty of Medicine. It was applied on two hundred Saudi nationality patients diagnosed with type II diabetes millets: 100 male and 100 female, aged between 30-65 years.
Sample selection criteria
All diabetic patients who fulfilled the inclusion criteria constituted the study population.
Inclusion criteria:Male and female Patients with T2DM attending the department of internal medicine- King Abdulaziz University Hospital (KAUH) aged between 30 to 65 years. Patients who suffer from T2DM for at least a year. Saudi Arabian nationality.
Exclusion criteria:All the patients had type I DM, Patients with type II DM not in the age group (30-65) years,Non-Saudi nationality and Pregnant women.
Assessment of the dietary habits
The first item of the validated version of Personal Diabetes Questionnaire (PDQ) was used with T2DM patients to allow them to describe the diabetes self-care behaviors in one major domain and the nutritional management, in addition to assess the dietary habits for them. The scoring scheme for the PDQ was based on grouping items by behavioral domain. Subscales were developed to represent each self-care behavior, or in the case of diet, different aspects on the behavior. A PDQ formatted for self administration may be downloaded from the internet (PDQ survey: http://healthbehavior.psy.vanderbilt.edu/PDQ. pdf) [15].
Glycosylated hemoglobin (HbA1c)
The study participantswere classified as <7 Excellent control, 7.1-8 Good control, 8.1-11 Fair control, ≥11.1 Poor control [16].
Blood pressure (Systolic pressure/Diastolic pressure)
The study participants were classified as low Blood Pressure 70-89\40-59, normal Blood Pressure 90-119\60-79, prehypertension 120-139\80-89, hypertension 140-190\90-100 [17].
Anthropometric measurements
Anthropometric measurement includes weight and heights were measured for all study samples in a screening room and the BMI was calculated.
Weight: Body weight was measured to the nearest 0.5kg by kilograms using a calibrated electronic weighing scale (LAICALC76 electronic scale).
Height: Height measurements was carried out by cm using a portable stadiometer scale in the standing position, without footwear, to the nearest 0.1cm. Height was converted to Meters in order to use it in further calculations.
Body mass index:BMI was calculated using as weight (in kilograms) divided by height (in meters) squared. It was classified as underweight <18.5, normal weight 18.5-24.9, overweight 25.0-29.9 or obese >30.0 [18].
Statistical analysis
Data analysis was carried out using the Statistical Package for Social Sciences (SPSS ver. 22.0). Descriptive statistics were applied (i.e., frequency, percentage, mean and standard deviation) for continuous variable.
Results
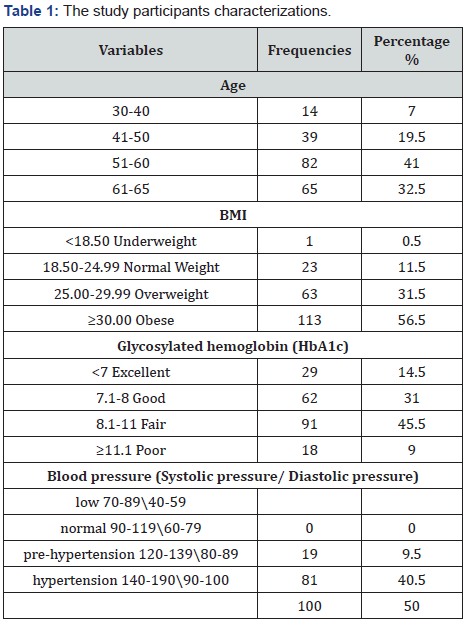
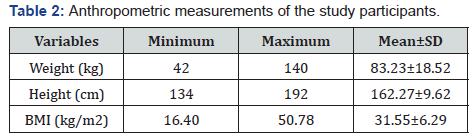
Most of the study participants (73.5%) were up to 50 years old of which (56%) were obese, (31%) overweight and only (11.5%) had normal weight. Most of the study participants (45.5%) had fair level of HbA1c (31%) had good level (14.5%) had excellent level and (9%) had poor level. Half of the study participants (50%) were suffered from high blood pressure (hypertension) and (40.5%) had pre- hypertension, while only (9%) had ideal or normal blood pressure Table 1. Data from Table 2 showed that the study participant’s weight which ranged between 42 and 140kg with mean 83.23±18.52Kg. The mean height was 162.27±9.62Cm. The BMI was ranged between 16.40 and 50.78kg/m2 with mean BMI 31.55±6.29 kg/m2.
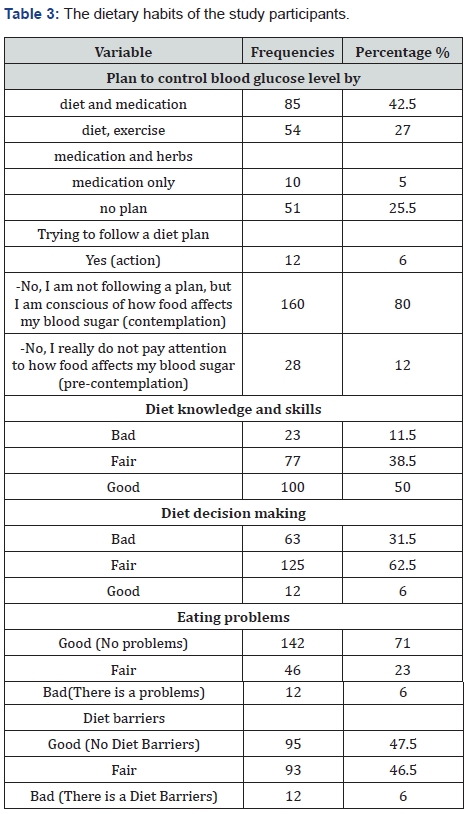
Most of study participants (42.5%) control their blood glucose by diet and medication while (25.5%) by diet, exercise, medication and herbs and (25.5%) with no plan to control their blood glucose. Moreover, only (6.0%) trying to follow a diet plan to control their blood glucose, while (80%) were not following a plan but they conscious of how food affects their blood sugar, (12.0%) not paying attention to how food affects their blood sugar.
Results showed that half of the study participants (50%) had a good level of diet knowledge and skills, (38.5%) with fair level and (11.5%) with bad level. Data of diet decision making showed that only (6%) of them taken the good decision, (62%) taken a fair decision and (31.5%) taken a bad decision. Nevertheless, most of the study participants (71.0%) does not had eating problems or diet barriers (47.5%) Table 3.
Discussion
Age considered as the strongest predictor of T2DM and prediabetes followed by obesity. People aged 50 years or over almost half of them had DM and another (10-15%) had prediabetes leaving only a small proportion of people in this age group with normal glycaemia [19-21]. Obesity is well documented to be associated with increased risk of various chronic diseases, including T2DM [22,23]. A study done in Saudi Arabia founded that obesity and, in particular, abdominal obesity is the second most important predictor of both DM and prediabetes [21]. Glycemic control becomes an important measurement for preventing long-term complications and provides a better quality of life to diabetic patient. Current guidelines for diabetes patients recommend maintain HbA1c of less than (7%) [24].
Hypertension is highly prevalent among Saudi adults 30- 70 years of age, affecting a quarter of the population [25]. In patients with T2DM the risk of diabetic complications was strongly associated with raised blood pressure. In addition, diabetes may leads to developing high blood pressure [9]. The risk of cardiovascular disease expected to rise by a factor of two to three at every level of systolic blood pressure [26]. Male and female diabetics patients but not prediabetes significantly associated with the presence of hypertension [21].
Any reduction in the blood pressure is likely to reduce the risk of DM complications, with the lowest risk being in those with systolic blood pressure less than 120mm Hg [27]. The T2DM and hypertension may be indirectly related to each other [28]. Metabolic and hormonal changes in obesity lead to increased blood pressure [29], and disturbance in lipid metabolism [30] hence there is an association between hypertension, dyslipidemia and T2DM. The effects of obesity need time to become apparent, so it was not noted in people with prediabetes. Obesity seems to be the main culprit in the development of both DM and prediabetes, and its long term effects might have mediated the association of DM with hypertension and dyslipidemia [21].
Interventions to reduce diabetes risk should primarily target weight reduction [31]. The calorie restriction program has an important role on metabolism of obese patients with non-insulin-dependent diabetes mellitus that is independent of weight loss [32]. In addition to reducing calories, exercise training also approved to reduce weight and the complications of diabetes. The results of [33] showed that physical activity in addition to educational programs of healthy lifestyle for diabetics provide significant weight loss and control of HbA1c [34] added obesity affects insulin resistance; therefore, weigh loss is an important therapeutic objective for overweight or obese individuals with pre- diabetes or diabetes. A good diet plan should fit in with diabetic schedule and eating habits. The right diet plan will help patients to improve their blood glucose, blood pressure, and cholesterol level [35].
One of the barriers for a diet programming of T2DM patients is the presence of psychological problems, such as depression, and the untreated depression for diabetic may lead to negative and harmful behaviors concerning life-style (avoiding physical effort) [36], emotional overeating [37] including night-eating syndrome [38]. This also might leads to nutritional disorders -psychological anorexia and bulimia [39].
Conclusion
Special attention should be given to the role of diabetic awareness programs, in the form of modifying lifestyles; hence, reducing complication of T2DM, obesity and overweight prevalence by weight control. As well as promoting a correct knowledge and skills about diet, improving the right diet decision making and adapting a healthier eating habits which in the long run, help to reduce the national burden of this disease and improving the health for T2DM patient.
References
- IDF International diabetes Federation (2013) Diabetes Atlas. (6th edn), Brussels, Belgium.
- Sami W, Ansari T, Butt NS, Hamid MRA (2017) Effect of diet on type 2 diabetes mellitus: A review. Int J Health Sci (Qassim) 11(2): 65-71.
- Elhadd TA, Al Amoudi AA, Alzahrani AS (2007) Epidemiology, clinical and complications profile of diabetes in Saudi Arabia: a review. Ann Saudi Med 27(4): 241-250.
- Beckman JA, Creager MA, Libby P (2002) Diabetes and atherosclerosis: epidemiology, pathophysiology, and management. JAMA 287(19): 2570-2581.
- Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, et al. (2010) Diabetes mellitus, fasting lood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 375(9733): 2215-2222.
- Al Nozha MM, Al Maatouq MA, Al Mazrou YY, Al Harthi SS, Arafah MR, et al. (2004) Diabetes mellitus in Saudi Arabia. Saudi Med J 25(11): 1603-1610.
- Alqurashi KA, Aljabri KS, Bokhari SA (2011) Prevalence of diabetes mellitus in a Saudi community. Ann Saudi Med 31(1): 19-23.
- Al Nuaim AR (1997) Prevalence of glucose intolerance in urban and rural communities in Saudi Arabia. Diabet Med 14(7): 595-602.
- Badran M, Laher I (2012) Type II diabetes mellitus in Arabic-Speaking Countries. International Journal of Endocrinology, pp. 11.
- Midhet FM, Al Mohaimeed AA, Sharaf FK (2010) Lifestyle related risk factors of type 2 diabetes mellitus in Saudi Arabia. Saudi Med J 31(7): 768-774.
- Mohieldein AH, Alzohairy M, Hasan M (2011) Risk estimation of type 2 diabetes and dietary habits among adult Saudi Non-diabetics in Central Saudi Arabia. Global Journal of Health Science 3(2): 123.
- Anderson JW, Kendall CW, Jenkins DJ (2003) Importance of weight management in type 2 diabetes: review with meta-analysis of clinical studies. J Am Coll Nutr 22(5): 331-339.
- Klein S, Sheard NF, Pi Sunyer X, Daly A, Wylie Rosett J, et al. (2004) Weight management through lifestyle modification for the prevention and management of type 2 diabetes: rationale and strategies: a statement of the American Diabetes Association, the North American Association for the Study of Obesity, and the American Society for Clinical Nutrition. Am J Clin Nutr 80(2): 257-263.
- Boulé NG, Haddad E, Kenny GP, Wells GA, Sigal RJ (2001) Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: a meta-analysis of controlled clinical trials. JAMA 286(10): 1218-1227.
- Stetson B, Schlundt D, Rothschild C, Floyd JE, Rogers W, et al. (2011) Development and validation of The Personal Diabetes Questionnaire (PDQ): a measure of diabetes self-care behaviors, perceptions and barriers. Diabetes Res Clin Pract 91(3): 321-332.
- Al Shammari SA, Nass M, Al Maatouq MA, Al Quaiz JM (1996) Family Practice in Saudi Arabia: Chronic Mortality and Quality of Care. International Journal Quality in Health Care 8: 383-387.
- Blood Pressure Association (BPA) (2008) Blood pressure chart, Blood pressure association, United Kingdom.
- Centers for Disease Control and prevention (CDC) (2018) Body mass index.
- Ramachandran A (2002) Epidemiology of type 2 diabetes in Indians. J Indian Med Assoc 100(7): 425-427.
- Thabit H, Burns N, Shah S, Brema I, Crowley V, et al. (2013) Prevalence and predictors of diabetes and cardio metabolic risk among construction workers in Ireland: the Construction Workers Health Trust screening study. Diab Vasc Dis Res 10(4): 337-345.
- Bahijri SM, Jambi HA, Al Raddadi RM, Ferns G, Tuomilehto J (2016) The prevalence of diabetes and prediabetes in the adult population of Jeddah, Saudi Arabia-a community-based survey. PLoS One 11(4): e0152559.
- Xu H, Barnes GT, Yang Q, Tan G, Yang D, et al. (2003) Chronic inflammation in fat plays a crucial role in the development of obesityrelated insulin resistance. J Clin Invest 112(12): 1821-1830.
- WHO World Health Organization (2014) Global Health Estimates: Deaths by Cause, Age, Sex and Country, 2000-2012. World health organization, Geneva, Switzerland.
- ADA American Diabetes Association (2012) Standards of medical care in Diabetes. Diabetes care 35(1): 11-63.
- Al Nozha MM, Abdullah M, Arafah MR, Khalil MZ, Khan NB, et al. (2007) Hypertension in Saudi Arabia. Saudi Med J 28(1): 77-84.
- Stamler J, Vaccaro O, Neaton JD, Wentworth D (1993) Diabetes, other risk factors, and 12 yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention Trial. Diabetes Care 16(2): 434-444.
- Adler AI, Stratton IM, Neil HA, Yudkin JS, Matthews DR, et al. (2000) Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ 321(7258): 412-419.
- Sugerman HJ, Wolfe LG, Sica DA, Clore JN (2003) Diabetes and hypertension in severe obesity and effects of gastric bypass-induced weight loss. Ann Surg 237(6): 751-756.
- MacMahon S, Cutler J, Brittain E, Higgins M (1987) Obesity and hypertension: epidemiological and clinical issues. Eur Heart J 8(suppl B): 57-70.
- Lumeng CN, Saltiel AR (2011) Inflammatory links between obesity and metabolic disease. J Clin Invest 121(6): 2111-2117.
- Hamman RF, Wing RR, Edelstein SL, Lachin JM, Bray GA, et al. (2006) Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes care 29(9): 2102-2107.
- Kelley DE, Wing R, Buonocore C, Sturis J, Polonsky K, et al. (1993) Relative effects of calorie restriction and weight loss in noninsulindependent diabetes mellitus. J Clin Endocrinol Metab 77(5): 1287- 1293.
- Gamiochipi M, Cruz M, Kumate J, Wacher NH, DIMSS Study Group (2016) Effect of an intensive metabolic control lifestyle intervention in type-2 diabetes patients. Patient Educ Couns 99(7): 1184-1189.
- Ong KL, Waters DD, Messig M, DeMicco DA, Rye KA, et al. (2014) Effect of change in body weight on incident diabetes mellitus in patients with stable coronary artery disease treated with atorvastatin (from the treating to new targets study). The Am J Cardiol 113(10): 1593-1598.
- Meng Y, Bai H, Wang S, Li Z, Wang Q, et al. (2017) Efficacy of low carbohydrate diet for type 2 diabetes mellitus management: a systematic review and meta-analysis of randomized controlled trials. Diabetes Res Clin Pract 131: 124-131.
- Lin EH, Katon W, Von Korff M, Rutter C, Simon GE, et al. (2004) Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care 27(9): 2154-2160.
- Ciechanowski P (2011) Diapression: An Integrated Model for Understanding theExperience of Individuals with Co-Occurring Diabetes and Depression. Clinical Diabetes 29(2): 43-49.
- Morse SA, Ciechanowski PS, Katon WJ, Hirsch IB (2006) Isn’t this just bedtime snacking? The potential adverse effects of night eating symptoms on treatment adherence and outcomes in patients with diabetes. Diabetes Care 29(8): 1800-1804.
- Colton P, Olmsted M, Daneman D, Rydall A, Rodin G (2004) Disturbed eating behavior and eating disorders in preteen and early teenage girls with type 1 diabetes: a case controlled study. Diabetes Care 27(7): 1654-1659.






























