Emotional -Affective Disorders and Quality of Life in Young Adult Patients with Diabetes Mellitus Type 1
Shimkina NF* and Barantsevich ER
Department of Neurology and Manual Medicine, Pavlov First Saint Petersburg State Medical University, Russia
Submission: January 15, 2018; Published: February 02, 2018
*Corresponding author: Shimkina NF, Department of Neurology and Manual Medicine, Pavlov First Saint Petersburg State Medical University, Saint Petersburg, Russian Federation, Russia, Tel: +7(911)093-57-75; Email: dr.shimkinanf@mail.ru
How to cite this article: Shimkina N, Barantsevich E. Emotional -Affective Disorders and Quality of Life in Young Adult Patients with Diabetes Mellitus Type 1. Curre Res Diabetes & Obes J. 2018; 5(4): 5556699. DOI: 10.19080/CRDOJ.2018.05.555669.
Abstract
Introduction:Diabetes Mellitus type 1 is associated with the development of emotional and affective disorders, varying in intensity and nature, the severity of which reduces the quality of life associated with the health condition.
Materials and Methods:Young adult patients with 14±6 years DM 1 duration, the level of glycated hemoglobin of 8-11%, the first group (N=50) were treated with CSII, the second group (N=50) -MDII, was investigated using standardized scales: HADS, 4DSQ, SF-36.
Data analysis:the information received from the subjects was analyzed in terms of frequency of violations. Results: In the studied groups a certain frequency of changes in emotional-affective reactions and decrease in the
Discussion:the analysis of the severity of emotionally-affective disorders showed the presence of disorders in the type of depression of 25%, distress of 20%, anxiety of 15% and 12% of somatization.
Conclusion:there is a certain structure of emotional-affective disorders in patients with type 1 diabetes, affected the self-esteem of the health status of patients with diabetes mellitus type 1. In patients with DM 1, with a duration of the disease of 14±6 years, the quality of life according to the SF-36 scale was reliably reduced, to a greater extent in the mental component of health.
Keywords: Diabetes mellitus type 1; Emotional-affective disorders; Quality of life
Abbrevations: CSII- Continuous Subcutaneous Insulin Infusion; DM 1- Diabetes Mellitus Type 1; QoL: Quality Of Life; MDII: Multiple Daily Insulin Injections
Introduction
High incidence rates of diabetes mellitus type 1 determine the need to search for and introduce new approaches to diagnosis and treatment of long-term complications of the disease. The presence of emotional-affective disorders in type 1 diabetes is undeniable [1,2]. A number of authors studied disorders in pediatric patients [3-5] and expressed psychoemotional disorders [6] in diabetes mellitus 1. In studies, various data were obtained on the prevalence of anxiety or depression [7]. Probably, the differences are related to the study of cohorts of patients that differ in the duration of the course of the disease, the level of metabolic compensation, or other parameters. In this study, the presence and severity of psychoemotional disorders, such as depression, distress, anxiety and somatization, in young patients with 14±6 years disease duration using Continuous Subcutaneous Insulin Infusion and Multiple Daily Insulin Injections and their impact on the quality of life associated with health condition [8] were investigated.
Material and Methods
The study included 100 patients aged 28 (21; 36) years with a duration of the disease of 14±6 years, the level of glycated hemoglobin - 8-11%, with no signs of macrovascular complications. Exclusion criteria were the presence of trauma to the nervous system, mental, neurological, somatic and infectious diseases leading to the development of cognitive or emotional-affective disorders. The first group (N =50) included patients who received CSII for the last 6 (5.6; 7) years, the mean age was 27 (21; 36) years, the duration of diabetes was 16 (11; 20) years, the level of glycated hemoglobin 9 (8.6; 9.7)%. The second group (N=50) included patients with MDII, the mean age was 28 (22; 37) years, the experience of the disease was 12 (9;16) years, glycated hemoglobin 9 (8.7; 9.6)%. By age and glycated hemoglobin, there were no statistically significant differences between the groups. The duration of the disease in the group of СSII was significantly greater. The evaluation was conducted using standardized scales: the presence of emotional and affective disorders was evaluated by HADS, 4DSQ [9-12]. Quality of life of patients - according to SF-36 [13,14].
Data Analysis
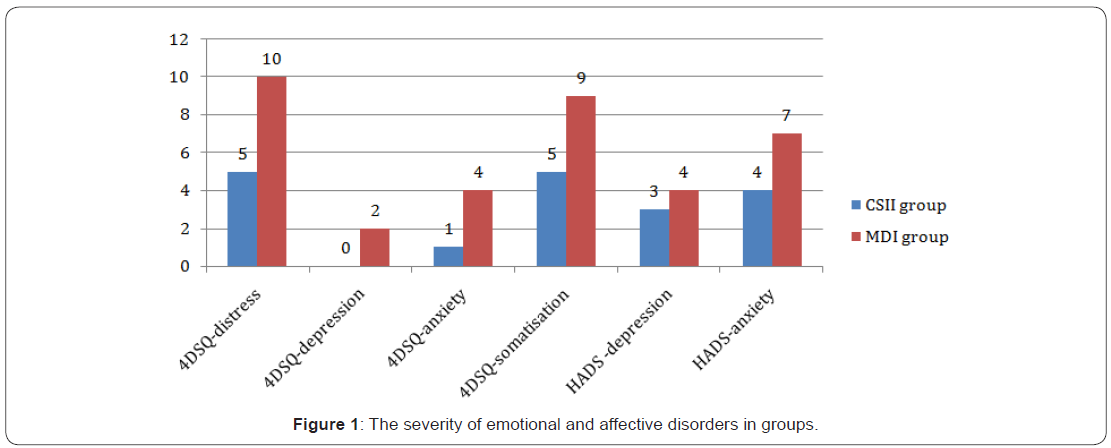
Frequency of violations was calculated and presented as a median and quartiles of indicators and is reflected in the tables and figure.
Results
In the studied groups of patients with DM 1, a certain frequency of changes in emotional-affective reactions was detected. Depressive disorders occurred in 25% of the examined, distress in 20%, anxiety - 15% and 12% signs of somatization. The lower frequency and severity of the disorders were in patients receiving CSII therapy (Table 1& 2) (Figure 1).
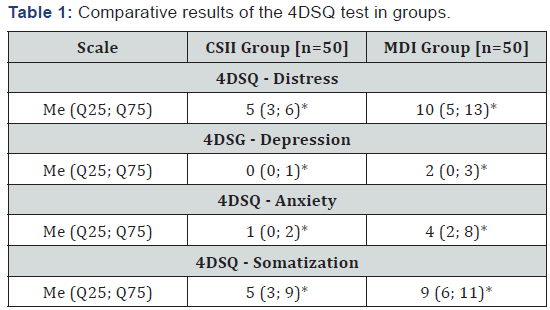
Note: n: number of patients; *: statistically significant differences between groups (p<0.05).
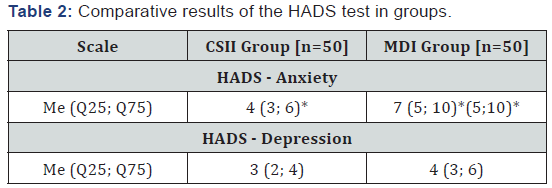
Note: n: number of patients; *: statistically significant differences between groups (p<0.05).
Note: n: number of patients; *: statistically significant differences between groups (p<0.05).
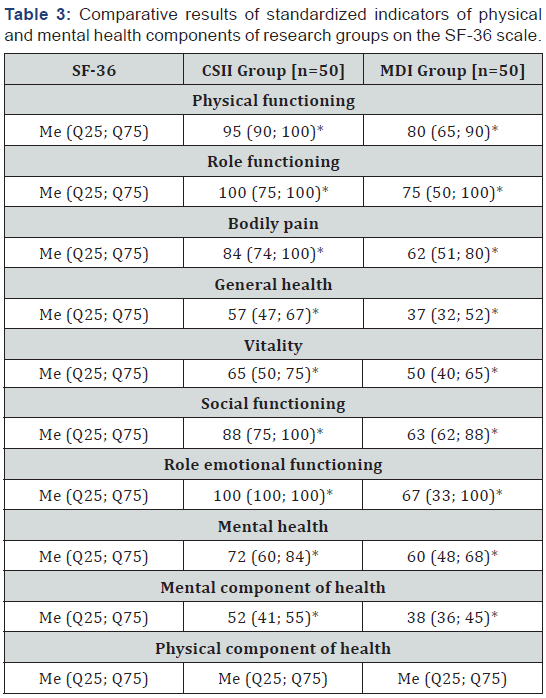
A negative correlation was found between several SF-36 scores and emotional-affective disorders (Table 4). The highest correlation was found between the increase in the level of anxiety and performance QoL (“physical functioning”, “bodily pain”, “general health”, “vitality”, “social functioning”, “role emotional functioning”, “mental health”), as well as a generalized indicator of the physical health component. The increased level of manifestations of distress correlates with “physical functioning”. The presence of manifestations of somatization is correlated with the index of “general health” (Table 4).
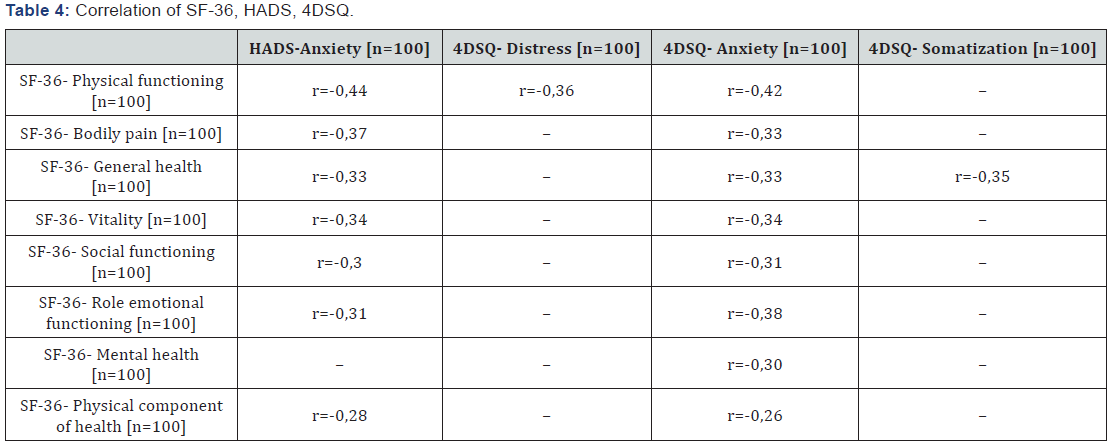
Note: n: number of patients; r: rate of Spearmen’s correlation.
Discussion
Questions relating to the psychoemotional state of patients with chronic somatic illnesses have been studied since the 20th century [1,2,6]. Various data were obtained on the nature of emotional-affective disorders in type 1 diabetes mellitus. Some authors have found that the psychoemotional background normalizes less than a year after the onset of the disease [4,5]. Other researchers argued that disturbance is persist and anxiety is dominative between other [7].
From our point of view, young adults with a DM duration of 1 14±6 years, the most frequently detects depression subclinical severity (25%), slightly lower incidence of distress (20%), anxiety and somatization also had a subclinical degree with approximately equal to the frequency. The study of the quality of life showed a decrease in the mental and physical components of the subjects’ health. However, mental health indicators, such as “vitality”, “mental health”, “social functioning”, were more reduced. In the MPI group, the “role function” indicators associated with the emotional state and “general health” were further reduced. In the infusion group, the indices of the components of physical and mental health were proportional to each other. In the injecting group, there was a more pronounced decrease in the mental health component, which reflects the greater severity of psychoemotional disorders in patients in this group.
Thus, it was found that the factor influencing the formation of a subjective quality of life for young patients with a duration of diabetes mellitus type 1 at the age of 14±6 years, is the expectation of damage associated with the disease and their impact on physical, role and social functioning. The indicators of QOL and emotional disorders are related negatively to each other. In our study, it was found that, in spite of anxiety is not the most frequent defect, it has the greatest impact on the formation of QOL. Increased anxiety in patients with DM 1 reduces the quality of life in terms of parameters associated with physical functioning (“physical functioning”) and more pronounced - related to the emotional state (“the role of emotional functioning”). The increase in the level of the distress is associated with a decrease in the indicator of “physical functioning”, and the manifestations of somatization are associated with a deterioration in patients’ self-esteem “general health”.
Conclusion
There is a certain structure of emotional and affective disorders in patients with type 1 diabetes with a duration of the disease of 14±6 years. Manifestations of depression account for 25% of cases, distress 20%, anxiety 15%, somatization of 12% of cases. The presence of emotionally-affective disorders affects the self-esteem of the health status of patients with diabetes mellitus type 1. A high level of anxiety reduces the assessment of one’s health status. Absence of anxiety is factor determining a higher assessment of the quality of life associated with the state of health. In patients with diabetes mellitus type 1, with a duration of the disease of 14±6 years, the quality of life according to the SF-36 scale was reliably reduced, to a greater extent according to the indicators assessing the mental component of health. The changes are most pronounced in the group of patients receiving insulin therapy by the method of multiple subcutaneous injections.
Conflict of Interest
Without any economic interests or conflicts of interest.
References
- Alberti KG, Zimmet PZ (1998) Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus. Diabet Med 15(7): 539-553.
- Grover J, Vats V, Rathi S (2000) Anti-hyperglycemic effect of Eugenia jambolana and Tinospora cordifolia in experimental diabetes and their effects on key metabolic enzymes involved in carbohydrate metabolism. J Ethnopharmacol 73(3): 461-470.
- Mukherjee P, Maiti K, Mukherjee K, Houghton PJ (2006) Leads from Indian medicinal plants with hypoglycaemic potentials. J Ethnopharmacol 106(1): 1-28.
- Eichler H, Korn A, Gasic S, Pirson W, Businger J (1984) The effect of a new specific α-amylase inhibitor on post-prandial glucose and insulin excursions in normal and Type 2 (non-insulindependent) diabetic patients. Diabetologia 26(4): 278-281.
- Patwardhan B, Vaidya D, Chorghade M (2004) Ayurveda and natural products drug discovery. Current Science 86(6): 789-799.
- Ponnusamy S, Ravindran R, Zinjarde S, Bhargava S, Kumar A (2010) Evaluation of traditional indian antidiabetic medicinal plants for human pancreatic amylase inhibitory effect in vitro. Evid Based Complement Alternat Med.
- Anandharajan R, Jaiganesh S, Shankernarayanan N, Viswakarma R, Balakrishnan A (2006) In vitro glucose uptake activity of Aegles marmelos and Syzygium cumini by activation of Glut-4, PI3 kinase and PPAR. Phytomedicine 13(6): 434-441.
- Joshi C, Priya E, Venkataraman S (2007) Hypoglycemic and antilipidperoxidative effects of a polyherbal formulation, Diakyur, in experimental animal models. Journal of Health Sciences 53(6): 734- 739.
- Meshram G, Yadav S, Dattatraya S, Patil B, Singh D (2011) Antibacterial study and effect of ethanolic extracts of Syzygium cumini seeds powder on glucoamylase in vitro. J Pharm Sci & Res 3(2): 1060-1063.
- Hasan R, Mokarram M, Raushanara A, Mariam J, Ehsanul H, et al. (2009) DPPH free radical scavenging activity of some Bangladeshi medicinal plants. Journal of Medicinal Plants Research 3(11): 875-879.
- Rahman MA, Moon SS (2007) Antioxidant polyphenol glycosides from the Plant Draba nemorosa. Bulletin of the Korean Chemical Society 28(5): 827-831.
- Liang LZ, Yi ML (2009) Antioxidant tannins from Syzygium cumini fruit. African Journal of Biotechnology 8(10): 2301-2309.
- Stanely Prince M, Kumar MR, Selvakumari CJ (2011) Effects of gallic acid on brain lipid peroxide and lipid metabolism in streptozotocininduced diabetic Wistar rats. J Biochem Mol Toxicol 25(2): 101-107.
- Meguro S, Nagao T, Hase T, Otsuka K, Komikado M, et al. (2009) A catechin-rich beverage improves obesity and blood glucose control in patients with type 2 diabetes. Obesity (Silver Spring) 17(2): 310-317.
- Rizvi SI, Zaid MA, Anis R, Mishra N (2005) Protective role of tea catechins against oxidation-induced damage of type 2 diabetic erythrocytes. Clin Exp Pharmacol Physiol 32(1-2): 70-75.
- Van Dam RM (2006) Coffee and type 2 diabetes: from beans to betacells. Nutr Metab Cardiovasc Dis 16(1): 69-77.
- Jung UJ, Lee MK, Park YB, Jeon SM, Choi MS (2006b) Antihyperglycemic and Antioxidant Properties of Caffeic Acid in db/db Mice. J Pharmacol Exp Ther 318(2): 476-483.
- Ruan ZP, Zhang LL, Lin YM (2008) Evaluation of the antioxidant activity of Syzygium cumini leaves. Molecules 13(10): 2545-2556.
- Balasubashini M, Rukkumani R, Menon V (2003) Protective effects of ferulic acid on hyperlipidemic diabetic rats. Acta Diabetol 40(3): 118- 122.
- Nomura H (2001) Acceleration of ferulic acid and related compounds on insulin secession. Research report of Wakayama industrial technology center, pp. 17-19.
- Jung EH, Kim SR, Hwang IK, Ha TY (2006a) Hypoglycemic effects of a phenolic acid fraction of rice bran and ferulic acid in C57BL/KsJ-db/db mice. J Agric Food Chem 55(24): 9800-9804.
- Hussain SA, Ahmed ZA, Mahwi TO, Aziz TA (2012) Quercetin dampens postprandial hyperglycemia in type 2 diabetic patients challenged with carbohydrates load. International Journal of Diabetes Research 1(3): 32-35.
- McCune L, Johns T (2002) Antioxidant activity in medicinal plants associated with the symptoms of diabetes mellitus used by the indigenous peoples of the North American boreal forest. J Ethnopharmacol 82(2-3): 197-205.
- Jo SH, Ka EH, Lee HS, Apostolidis E, Jang HD, et al. (2009) Comparison of antioxidant potential and rat intestinal α-glucosidases inihibitory activities of quercetin, rutin, and isoquercetin. International journal of applied research in natural products 2(4): 52-60.
- Rosen OM (1987) After insulin binds. Science 237(4821): 1452-1458.
- Gajera HP, Gevariya Shila N, Hirpara Darshna G, Patel SV, Golakiya BA (2017) Antidiabetic and antioxidant functionality associated with phenolic constituents from fruit parts of indigenous black jamun (Syzygium cumini L.) landraces. J Food Sci Technol 54(10): 3180-3191.
- Gajera HP, Gevariya Shila N, Patel SV, Golakiya BA (2018) Nutritional profile and molecular fingerprints of indigenous black jamun (Syzygium cumini L.) landraces. Journal of Food Science and Technology 55(2): 730-739.
- Ayyanar M, Subash Babu P (2012) Syzygium cumini (L.) Skeels: A review of its phytochemical constituents and traditional uses. Asian Pac J Trop Biomed 2(3): 240-246.






























