Artificial Intelligence and Robotics: Catalysts or Threats in the Development of Healthcare
Dimitris Karaferis*, Dimitra Balaska and Yannis Pollalis
Department of Economic Science, University of Piraeus, Piraeus, Greece
Submission: August 29, 2024; Published: September 13,2024
*Corresponding author: Dimitris Karaferis, Department of Economic Science, University of Piraeus, Piraeus, Greece
How to cite this article: Dimitris K, Dimitra B, Yannis P. Artificial Intelligence and Robotics: Catalysts or Threats in the Development of Healthcare. Biostat Biom Open Access J. 2024; 11(5): 555825. DOI: 10.19080/BBOAJ.2024.11.555825
Abstract
Background: This article emphasizes the significant and revolutionary impact of artificial intelligence (AI) and robotic technologies in public health. It can be beneficial for the European Union, including Greece, where access to healthcare providers and resources are limited for some segments of the population, especially in rural areas. The article delves into the ethical, legal, technical, and social challenges connected to implementing AI systems and robotics in public health. The article attempts to approach whether the already existing legislation of the European Union provides the possibility for good protection of the health of workers and the performance of their tasks using AI systems and robotics technologies.
Methods: The study was conducted using literature related to AI systems and robotics in healthcare settings, as well as based on current legislation relating to the safety and health protection of employees and patients in the European Union.
Results: There has been a notable increase in the utilization of AI systems and robotics in the healthcare sector recently. Functions such as facilitating hospital logistics, performing routine examinations and assisting in surgery, are just a few of the tasks that can be accomplished very efficiently. Especially, in terms of providing a safe working environment with low-risk conditions of infection for healthcare employees, perfectly organized operational tasks, preventative and exclusive patient care, treatment recommendations and patient engagement. AI systems can now enable patients to monitor and even control their own health and disease progression.
Conclusions: The healthcare sector is considered one of the most vital worldwide, which seeks to accelerate its growth through innovative approaches and modernization. The future of this particular sector lies in a sea change towards the creation of intelligent machines that behave and react like humans. New challenges create new needs to continue adapting European Union legislation to changing realities.
Keywords: Artificial intelligence; Robotics; Big Data; Healthcare; European Union Legislation; Greece
Abbreviations: AI: Artificial Intelligence; ML: Machine Learning; DL: Deep Learning; NLP: Natural Language Processing; LOS: Length of Stay; HER: Electronic Health Record
Background
Over the last two decades, the shift towards patient-centered healthcare has led to a notable demand for the development of artificial intelligence (AI) systems and robotic technologies that facilitate diagnosis, decision-making, treatment, and the digitalization of healthcare. AI systems, combined with robotics and access to big data, form the backbone of rapidly developing and advancing digital healthcare, make it one of the most revolutionary areas for the future of daily life of citizens and society in European Union. The evolving importance of the of AI and robotics perspective, has been demonstrated in several studies, reporting that regardless of the level of exposure, it can make a positive contribution to the medical and healthcare field, potentially staggering and increase the added value of patient access, safety and respectful treatment. Moreover, it can optimize the way resources are allocated and help the healthcare system operate more effectively and deliver high-quality care [1].
Globally, using AI applications and data are challenging. Data quality, quantity, diversity, and privacy of data are key elements of data-driven AI applications, each presenting unique challenges. These obstacles consist of, but are not limited to, meeting important healthcare objectives, like enhancing health outcomes for the population, improving patients’ care experience and safety, caregivers’ experience, and lowering healthcare costs [2]. Fundamental problems such as misdiagnosis, not necessary treatment, unsafe hospital practices, medication errors, and lack of appropriate medical training and expertise exist, although there is variable progress within individual countries. Additionally, the growing demand for health services is primarily caused by a rising and elderly population, along with a growing burden of chronic diseases and comorbid conditions, the need for long-term health services, and the preference of older people to stay in residential care facilities or in their own home to receive healthcare services, are considered as important reasons [3].
Notwithstanding, the large amount of data available in healthcare institutions or data generated in non-medical institutions, the vast majority are inaccessible or unusable, which makes the development of healthcare solutions extremely difficult. Even if the data is available, the dataset is not viable, with systems not able to synthesize data, and communicate with and use information from different systems. Consequently, the absence of interoperability and a unified standard format are among the major obstacles to the widespread adoption of digital health solutions. Technology can be a solution for the healthcare sector to improve its effectiveness and achieve sustainable development goals for quality in health and well-being. Indeed, the emergence of vast amounts of data, robust computing power, and sophisticated machine learning algorithms represented important and advantageous advancements. As the matter of fact, most of the recent technological advances turn out to be beneficial and advantageous. Many technologies complement our work instead of replacing it, reducing the load and saving time for other activities. Already, much literature suggests that AI and robotics are accurate and reliable in many health care organizations and perform many tasks such as genetic testing, robotic surgery, medical imaging, cancer research and data collection. The ubiquity of the aforementioned two technologies could change various areas of health care. Especially, AI and robotics are expected to be used to diagnose patients’ conditions, reduce medical errors and costs, and enhancing quality of life for people with disabilities and to maximize the patient’s chances of survival. Such findings, derived from data analysis and machine learning models, signal the dawn of evidence and probability-driven healthcare and are mostly well-received, yet they also present ethical and relational hurdles for medical ethics and the patient-physician relationship [4].
Some scientists and activists point out that there are dangers associated with the adoption of AI and robotics, especially in the vital and rapidly changing field of healthcare. These risks include privacy and surveillance rights, data protection, human dignity, equality, non-discrimination, possible control, manipulation, potential for bias and discrimination, violation of fundamental rights through disruption of social interactions and values. Therefore, to maximize the utilization of AI and robotics effectively in the European Union, it is essential to establish robust policies concerning sufficient data access, appropriate regulations, fostering innovation in both small and large medical institutions, supporting the integration of new technologies, and dealing with various ethical and legal issues concerning patient rights and protection [5].
This study addresses the following inquiries: a) What are the benefits of AI technologies offer to health systems, caregivers and patients, b) What are the perceived challenges while implementing AI and robotics, c) How to bridge the gap between the advantages and challenges in the advancement of AI and robotics in the healthcare field.
Methods
Purpose of the study
The aim of this article is to provide the benefits of developments in artificial intelligence and robotic technologies in healthcare, risk analysis and threats associated with the development of these two technologies, and the current legal framework for the protection of employees and patients.
Material and analysis
The examination made use of literature concerning artificial intelligence and robotics in healthcare. Findings from forensic science were also utilized, along with literature on workplace health and safety. The study was conducted in accordance with the existing legal guidelines in the European Union concerning the protection of workers’ health. The methodologies of the publications were validated and qualified based on how well they aligned with the subject matter. The literature review utilized the specified databases and online journals, among others: Scopus, PubMed, Elsevier Direct, Medline, EBSCO, CINAHL, and Web of Science. Sources of information were found through keyword-based searches in such databases, online repositories and digital libraries, while considering the publication date, author and the article type. The literature chosen consisted of research articles deemed important for addressing the research inquiries raised in this study.
Results
Urgent challenges in the health care systems
Unlike other fields, public health care is not a simple process but a straight forward cut. Traditional medicine, health professionals, diseases, patients, behaviors and systemic problems are just some of the features of this complex puzzle. Hence, there is always a need for health care processes to adapt to new changes to effectively deal with growing health care demands [3,6]. Basic pressing challenges and unmet needs that form a peculiar environment for each health care system are:
i. Growth and ageing population, the world population is growing in a fast pace, by about 82 million people each year. At this rate, the world population is estimated to reach 9 billion in 2037 and 10 billion in 2057. In European Union countries, the proportion of people aged 65 and above in the total population will increase from 19% in 2016 to 29% by 2070 [7]. Similarly, as the population ages more and more, this has a direct consequence on healthcare systems that are constantly strained.
ii. Mental health, conditions related to mood and mental health are increasing. WHO has expressed its concerns about this issue, since in the surveys carried out one in four people in the world face poor health and co-morbidities [8].
iii. Reduced cost and errors, managing patients requiring complex care which is expensive and requires the health care sector to shift from cure to prevention.
iv. Communication and interaction within hospitals, primary healthcare centers and patients, in many European countries, pressures on healthcare have led to shorter consultation times and less dialog between physicians and patients.
v. Sustainability, as countries’ infrastructures age and demand for more beds increases, hospital executives and governments need to reconsider how to optimize wall-free inpatient settings.
vi. Remote treatment, telemedicine and virtual care can be incorporated into any healthcare system to enhance the efficiency of the services provided [9].
vii. Rise of chronic diseases, resulting in diminished quality of life and functionality, greater reliance on healthcare services, elevated death rates, and increased healthcare expenses [10].
viii. Lack of health personnel, the healthcare public sector is experiencing staff shortages in almost every country in Europe, and the workforce gap is expected to widen globally.
ix. Lack of interoperability and standardization among medical IT systems. Reasons enough, then, for healthcare to look for smart ways to work more efficiently.
Artificial intelligence in healthcare
With its infinite power, artificial intelligence is already having an impact on healthcare and is hastening breakthroughs, with new hopes for even greater advances emerging every day. Precisely, AI has been utilized in medicine and healthcare since the 1960s, as physicians began experimenting with computer-assisted programs to enhance diagnosis processes [11]. Terminologically, Artificial intelligence (AI) systems encompass a variety of applications and refers to describe the use of computers (both software and sometimes hardware) and technology to imitate intelligent behavior and critical thinking similar to humans. Actually, these systems, when faced with an intricate objective, observe their surroundings by gathering data in either a physical or digital form, analyze the structured or unstructured data they gather, and conduct analysis based on their acquired knowledge. It operates by analyzing the data and using that information to determine the most effective course of action to achieve the objective goal. Ultimately, AI involves a machine replicating human behavior, regardless of the methods employed. Incomplete patient medical histories and high caseloads, especially in emergencies, can lead to fatal human errors. By treating these variables, AI enables most medical professionals to diagnose, treat, and manage any disease at a much faster rate. By doing this, personalized and precise healthcare can shift from an idea to an actuality, patient results can be greatly enhanced, healthcare providers will gain fresh authority, and effectiveness can increase throughout the healthcare sector. Utilizing big data (defined large data sets), including variability, velocity, variety, volume, quantity and accuracy, AI has rapidly developed into the foundation of medical research and healthcare worldwide. Despite their advanced problem-solving capabilities, computers do not possess the human skills required for intricate social interactions like persuasion or forming emotional connections, leading to limitations in creating original ideas and fostering relationships [12-15].
Subfields of Artificial Intelligence in Healthcare
AI is a wide term that encompasses various computational technologies, techniques, processes, applications, and models. It is therefore understandable that it is a collection of different cognitive functions, like Machine Learning (ML), Deep Learning (DL), Natural Language Processing (NLP) and Robotic technologies have the potential to benefit public health by leveraging the increased generation and accessibility of health data [16].
Big data and cloud computing are currently employed in the field of mobile health (mHealth), where wearable sensor devices utilize cellular network technology to transmit health data to hospital databases and seamlessly it to cloud storage systems. Machine learning (ML) techniques allow AI applications to utilize the vast amount of digital data and experience collected and available from cognitive input to automatically improve algorithms. Parameter selection and screening is one of the main objectives of machine learning. Exploiting big data and AI algorithms can be used to either improve our understanding of the current environment or make informed predictions based on what they has been learned in the past and what they have been trained on, so a system have the opportunity to be faster, smarter and more accurate by understanding learning data and help professionals gain unprecedented insights into treatment variations, creating medical care regulations and even more perform highly complex activities, care processes, diagnoses and patient outcomes. Yet, by analyzing patient records and medical images to discover new treatments, the data science behind ML provides more opportunities to healthcare professionals to identify any abnormalities and underlying causes, conduct risk assessments, improve treatment and reduce costs. Essentially, ML systems work according to input rules and allow the system to think and learn for patterns. Despite this, ML systems classify input data and through patterns make predictions-outputs. Unlike the human brain, ML technology does not have a limit to how much it can learn, does not panic, does not deplete, and has unlimited information storage capabilities [17-19].
Deep learning (DL) is a subset of machine learning that relies on artificial neural networks. These networks consist of layers of nodes that can be connected to each other and learn to recognize patterns from extensive quantities of data. The greater the amount of data available to the DL system, the more operations it carries out, which increases predictability and accuracy, leading to better and more accurate results. For this reason, DL networks specialized to recognize complex patterns, such as images, text, and audio. After being trained, the algorithm can assist in customizing treatment plans for individual patients in areas like oncology, examining medical images (such as X-rays, CT or MRI scans) and ultrasound imaging of chronic illnesses, resulting in significant improvements in healthcare outcomes and revolutionizing the use of medical imaging in diagnosing and managing treatments. Ultimately, DL requires significantly less artificial input and is self-correcting when high prediction accuracy is required [20-22].
Natural Language Processing (NLP) technology is a branch of machine learning applied in the development of clinical question-answering systems to extract valuable information from linguistic and textual data and utilizing it for various tasks. By extracting significant insights from unstructured textual information that may be found in clinical texts, medical literature, guidelines, physician’s notes, electronic health records (EHRs) or patient reports, these systems have the inherent ability to interpret and answer medical queries based on medical ontologies, identify trends, generate hypotheses, and have a major impact on expediting the decision-making process. NLP techniques makes human language accessible to computers while at the same time enabling healthcare professionals to receive contextualized and sensitive recommendations, warnings, and nuanced guidelines at the point of care, and as a consequence NLP has excellent potential in the field of patient care. For instance, interactive chatbots could be used to cover conversations with patients about repetitive and frequently asked questions, freeing up healthcare providers’ resources to deal with more complex cases. Apart from that, it can also help to increase patients’ health awareness, improve quality of care and identify patients in need of critical care. These examples merely scratch the surface of the immense potential for NLP technology to revolutionize clinical text analysis. As the rapidly advancing field of NLP in healthcare keeps growing, novel techniques and applications continue to emerge to improve healthcare delivery, facilitate cutting-edge research methods and ultimately improve patient outcomes [23-25].
Robotic technologies in surgery have gained a lot of popularity, as it helps surgeons, patients and healthcare providers. Integrated with cameras, 3-dimensional view, mechanical arms and the required surgical instruments, robots have pioneered a new era in surgical procedures, increasing the knowledge, skills, and experience of the physicians. Robotic surgery gives physicians the opportunity to minimize the risk of errors, reduce invasive surgeries, provide better control, flexibility and visualization, scale movement and improve the convenience of surgeries to all parties involved in the process, if implemented appropriately. Robotic-assisted surgery implemented with artificial intelligence usually results in fewer complications, relatively less pain for the patient, and a faster recovery rate. Likewise, robotic caregivers can help patients, the unwell, and senior citizens with a range of tasks to provide healthcare services that are more precise and secure. Also, intelligent carrier robots can move patients from bed to wheelchair or assist them to repositioning when needed or even can provide bed baths. Nurses, who were previously responsible for all these activities, will have the opportunity to engage more with their patients [26-30].
As the scope of AI in healthcare is wide-ranging, for this reason various applications of medical AI exist for different medical fields, encompassing clinical, diagnostics, rehabilitation, surgery and predictive care. Other examples include the use of ΑΙ to measure patient feedback, behavior and engagement, or its use for administrative tasks such as billing, drug dosages, coding, or other business applications.
Improvements from the utilization of Artificial Intelligence in Healthcare
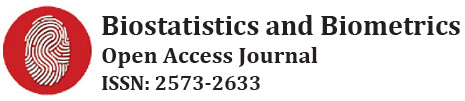
There is high hope that implementing artificial intelligence (AI) can result in major enhancements across different healthcare sectors and result in incredible advances in the medical scene, from back-office tasks to patient care, categorized into (Figure 1):
i. Accurate diagnosis and treatment, the utilization of AI will allow healthcare professionals to discover previously unseen correlations between diseases in medical data and detect subtle changes in vital signs that signal potential problems. Fortunately, there is no AI tool that can mimic the human connection. However, the advent use of AI technology and automation will significantly improve research, disease diagnosis and medical outcomes. The possible uses of AI in healthcare are vast and extensive, ranging from analyzing radiological images and overseeing lab results to anticipate outcomes using electronic health records. AI-driven predictive models in medical facilities have the potential to improve the healthcare system by enhancing productivity, efficiency, and intelligence, particularly in predicting readmission risks, complication risks, and mortality. This in turn will allow physicians to spend more time treating patients directly, recommend tailored treatment plans, and choose the best policy to treat patients with incurable diseases and other health problems [31-34]. Notably, in many countries, it is estimated that 10-20% of all serious injuries in healthcare have an incorrect, delayed or unstable diagnosis as the cause. Diagnostic errors are most common especially in emergency departments and in working environments described as stressful [35,36].
ii. Risk assessment and future disease, the pandemic COVID-19 has challenged nearly all of global healthcare, highlighting the risk of rapid escalation of human-to-human transmission of the virus in the absence of prior immunity. Productive AI models are rapidly becoming invaluable in investigating the large-scale impacts of catastrophic events, helping to model and predict new pandemics, and recommending prevention strategies based on past pandemic data. AI is currently being utilized as a demonstration in medical areas like pathology, radiology, and dermatology, which share similarities with ophthalmology as they are heavily reliant on diagnostic imaging, which is the foremost application of AI in health and medicine. Moreover, AI analytics models combined with social media can be used to determine the risk of mental illness using human behavioral data and identify risks of mental illnesses [37,38]. Additionally, Chatgpt can influence mental health support through conversations with individuals experiencing emotional or psychological distress. In reality, Chatgpt is not a substitute for professional therapy, but it provides a listening ear, offers resources, and helps individuals better understand their feelings [39].
iii. Administrative assistance, medical professionals regularly encounter fresh obstacles because of changing duties and frequent disruptions in a dynamic and constantly shifting medical environment. Physicians are believed to dedicate approximately half of their usual daily practice hours to administrative duties and desk work [40]. AI can not only automate administrative tasks like appointment scheduling and reminders, follow-up communications, record-keeping but also can minimize the burden on hospitals due to unnecessary medical interventions, resource consumption, hospital overcrowding and loss of time and effort. AI can also help reduce clinician burnout by minimizing administrative burdens such as documentation [41]. The utilization of AI and automation can help with many routine tasks, making processes more efficient and freeing up providers’ time for other activities. Physicians and other medical professionals have the ability to verbally dictate notes without using their hands, allowing them to spend more time directly interacting with patients. AI technology assists healthcare providers in ensuring that medical documentation is thorough by offering suggestions and recommendations. Ultimately, AI can assist in precise coding, exchanging information between departments, and handling billing.
iv. assessment, many researchers have found that patients are satisfied with the use of AI, with responses provided by nurses available 24/7. AI-powered wearable devices have been utilized for monitoring and analyzing essential signs in patients, including blood pressure, heart rate, saturation, body temperature, blood glucose levels, and quality of sleep. Nurses are no longer burdened with constant manual monitoring and do not have to perform numerous interventions with patients, resulting in improved care quality and increased patient satisfaction [42,43]. AI virtual nursing assistants, such as AI-driven chatbots, applications, and other interfaces, can be utilized to assist individuals and older individuals with various tasks. For instance, they can be relied upon to answer medication questions, respond to routine patient inquiries via phone or email, report to physicians or surgeons, schedule appointments, and send patients reminders for follow-up and clinical appointments, etc. Ultimately, all these procedures can benefit both patients, healthcare providers and institutions by reducing the frequency of hospital visits. Such routine monitoring and scheduling allow staff to spend more time to personally socialize with patients, where human judgment and interaction matter most [44-46].
v. Staying in hospitals, telehealth monitoring not only reduces the need for hospitalization of patients, but can also enable some patients to stay at home while their health conditions monitored by machine-learning algorithms. Hospital length of stay (LOS) is a crucial aspect of healthcare effectiveness as it directly affects healthcare costs [47]. Alternatively, LOS may result in higher expenses and potential medical issues linked to a heightened likelihood of acquiring hospital-acquired infections. AI systems at home can be used to monitor patients with insulin irregularities, heart arrhythmias, swallowing problems, and other medical issues instead of relying on physicians.
vi. Dosage error reduction, AI-based decision support systems have been proven to improve patient safety through error identification, patient categorization, and medication oversight across all stages, including prescribing, administering, and dispensing. Considering unique patient traits and customizing treatment can reduce errors related to incorrect dosing with the help of AI. With the help of wireless sensing AI technology, devices in the patient’s environment can detect mistakes in the way the patient uses insulin pens and inhalers. Even an extra dose of a drug or medicine can have disastrous consequences for the body of patient, it is therefore very important that patients take the prescribed dose of medication correctly and on time [48].
vii. Safer surgeries, the field of surgery has witnessed tremendous and continuous technological advances in recent years. AI-powered robots are present throughout the entire surgical process, from the beginning to the end. Additionally, AI helps surgeons work in tighter spaces as opposed to traditional open surgery, navigating around delicate organs and tissues in confined areas, reducing blood loss, complications, and post-operative discomfort. Until now, studies in neurosurgery, orthopedics, ophthalmology, and urology have shown the significance of AI in improving the diagnosis and outcomes of medical operations like total joint replacement, prostate cancer, and brain tumor treatment. As a consequence, robotic surgery often results in reduced scarring and faster recovery times compared to conventional surgery [49,50].
viii. Fraud prevention, fraud is widespread in healthcare; AI can assist in identifying abnormal or questionable activity in claims, like billing for costly services or procedures through unbundling, unnecessary tests to exploit insurance payments [51].
ix. Medical training and education, Chatgpt serves as a training aid for healthcare professionals, assisting them in improving their expertise and abilities. The ability to simulate patient interactions, allows healthcare providers to practice clinical decision-making, diagnostic reasoning, and communication skills in a virtual environment. Simulation also allows clinicians be trained quickly on a series of trials before moving on to real-life circumstances. Using computational simulation is way more effective than physically manipulating the simulation environment, and the advancement in computing power is creating virtual simulation environments to improve the accuracy of real-world modeling. This obviously benefit medical education, training programs, and continuous professional development [52, 53].
x. Patient engagement and training, three quarters of patients believe that scientific progress should prioritize the needs and concerns of patients and their families. A consensus is developing that patient engagement and education are crucial in healthcare delivery and safety [54].
xi. costs, technology has the potential to reduce hospital admissions and hospitalizations repetitive tasks by focusing healthcare professionals on critical thinking and clinical creativity [55].
In 2023 (Figure 2), the top four applications of AI in healthcare worldwide were robot-assisted surgery (21.56%), virtual nursing assistant (16.45%), administrative workflow assistant (14.08%), and medical imaging & diagnosis (12.55%).

Artificial intelligence during the Covid-19 outbreak
The hospitalization of a large number of patients during the Covid-19 pandemic caused the global health system to collapse. Shortage of healthcare professionals due to illness, exhaustion and burnout, scarce hospital resources, limited access to Covid testing and protective equipment, and the need for real-time speed, responsiveness, proactivity, accuracy, analytical capacity and precision, become even more pronounced. Due to these constraints, governments, the private sector, and public health systems are increasingly interested in developing AI systems, telemedicine and robotics to improve patient management [56-58].
In this context, data and artificial intelligence have come to the fore as key solutions in the fight against the pandemic, both as medicine to find vaccines, drugs or cures, and as the development of public sensing applications to identify potentially infected individuals. In this sense, AI applications have been focused on strong analysis, diagnosis, and treatment (e.g., prevention and self-treatment), by minimizing in-person interactions and hospital appointments, thus decreasing the potential transmission of Covid-19 and other viral pandemics. Furthermore, has worsened the accessibility situation for many people, particularly in disadvantaged areas, who have lost their jobs and some or all of their income and as a consequence the access to health insurance. More than ever, AI-related technologies are more central than ever in tackling this worldwide health emergency. Thanks to advances in computing and AI, telemedicine makes it possible to give physicians the opportunity to treat patients and prescribe medicines. Telemedicine is also being recognized more than ever as a valuable technology that can provide home healthcare to the vast majority of people. Furthermore, machine learning and DL technologies and tools have sped up medical research on drug discovery, quick genome sequencing to gain a better understanding of viruses, and predict patient outcomes. Moreover, quick identification of medical images has played a crucial part for artificial intelligence in current difficult circumstances. AI has not just improved diagnostic capabilities, but also played a key role in virus containment efforts [59-61]. Consequently, AI applications has been crucial in helping healthcare professionals respond to the coronavirus outbreak and develop Covid-19 immunization drugs.
Nevertheless, the Covid-19 outbreak presents a possible danger to the privacy, confidentiality, and security of patient and citizen information. The future of technology-driven healthcare’s societal impact is uncertain. These actions could lead to significant outcomes, such as the unauthorized release or exploitation of confidential information that infringes on citizens’ rights, or the repurposing of medical data for non-health-related purposes.
Considerations in implementation of AI and Robotics Technologies
Without no doubt the potential benefits of AI in healthcare are immense, however there are several challenges, barriers and dilemmas around privacy, trust, transparency and accountability associated to its implementation (Figure 3).
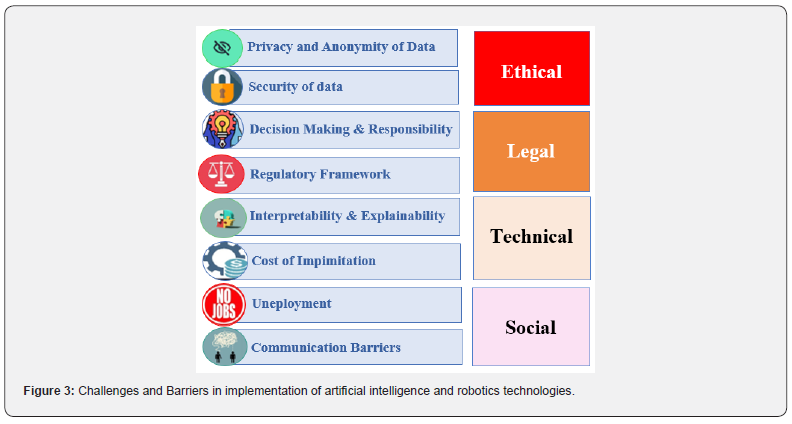
Ethical Considerations
While the potential benefits are immeasurable, the use of ΑΙ and robotics scares many people due to concerns and fear of the various impacts that the development of technology brings to the health care of individuals, the functioning of organizations and society in general. It is obvious that there are difficulties, vigorous skepticism, worries and limits to overcome before it can be implemented. Privacy and anonymity of health data is serious but common concern facing AI in healthcare. Since medical AI technologies rely on medical data, sharing this data across different platforms during the process can potentially compromise individuals’ privacy, while AI software is expected to eventually handle tasks currently requiring human involvement [62-67]. Ensuring data security is another major challenge and is the responsibility of all stakeholders. In particular, healthcare professionals must receive training on the importance of privacy and security measures for healthcare data [68-71].
Legal Considerations
Humans are by nature combine various cognitive processes and abilities to think, reason, examine and adapt to new situations. So, decision making and responsibility are crucial capabilities that are essential for health research. Through knowledge and frequent training, AI can knowledge, but not human thought processes and critical thinking. Medical decision-making has traditionally been carried out by frontline professionals, but the introduction of intelligent machines in decision-making and support brings up concerns regarding privacy, consent, accountability, and transparency. Considering this viewpoint, with AI transitioning from a luxury to an essential component of contemporary digital systems, it is crucial to think about the possible consequences and determine who is responsible for managing it. Health systems should at least consider the following aspects when planning the use of AI for health [72]:
i. Accessing domain expertise and background knowledge is necessary in order to comprehend and establish the essential rules that must be followed when dealing with the dataset.
ii. Access to cloud computing is advanced enough to enable real-time decision-making.
iii. Guidelines for responsible and ethical data access: healthcare and medical data are extremely confidential, variable, substantial, and not ideal for machine learning advancement, assessment, utilization, and integration intentions.
iv. Implementation research of utilization of algorithms and their integration into appropriate workflows
v. An appropriate regulatory framework.
Technical Considerations
The interpretability and explainability of AI’s capabilities should also be considered. Despite the so many advantages of AI, its application in medicine has not been universally accepted because the accuracy of AI algorithms is not completely one hundred percent. This means that AI has the potential for clinical bias and errors. Furthermore, AI’s lack of interpretability is evident in certain instances, with professionals struggling to comprehend the functionality of AI algorithms, thus hindering the ability to elucidate certain AI behaviors. In the field of clinical care, professionals face challenges in conveying the process of decision-making to patients when they lack comprehension about AI’s role in making medical decisions and the resulting outcomes [71,73,74].
Social Considerations
Some healthcare professionals support that the introduction of AI and robotics risks dramatically changing the size of the healthcare workforce, this means that if automation, AI technologies and robotics potentially continue to grow in the healthcare industry is something that could cause the replacement of previously essential workers. Adoption of AI by key stakeholders such as physicians has so far remained low [75-77]. Certainly, different technologies have been introduced over the past century or more, and in many cases the displaced employees have found other employment. There is therefore every reason to believe that this re-displacement of workers will happen again. How to deal with new environmental and technological innovations is a matter of time, resources and policies. The ultimate solution, beneficial for society as a whole, will come from our efforts and initiatives to offset the negative impacts of AI and robotics on our lives and society and embrace the positive ones. When healthcare relies on AI tools, communication barriers may arise between patients and machines; this fact decreases face-to-face interactions between patients and physicians. Many patients way only want human social interaction during the consultation and may not want to change this traditional physician-patient relationship. Patients should reduce their fear of AI devices, and physicians should be competent in interacting with AI systems to ensure effective healthcare delivery [64].
Responsible AI Systems and Robotics technologies
As always, transition to new technologies and adaptation to new environments is complex and changing our working life, with many different dynamics interacting with each other. Despite the massive potential of AI systems and robotics, they are still far from replacing many types of tasks that employees are good at. In a specialized field like healthcare, seems that AI technology and robotics are capable of replacing employees in doing dangerous, heavy, routine, exhausting, repetitive and predictable tasks, as well as in tasks that require great precision at microscopic scales. Usually, technological trends always replace the lowest-paid workers, but AI is now also gradually supporting and possibly replacing analytical tasks. This is because, AI technology and robots will most likely be used alongside human employees, as in no sense, are able to replace the complex nature of decision- making, creativity, innovation or human characteristics such as emotions and compassion, that cannot be easily mimicked, since their skills and abilities cannot be easily programmed and replace abled by robots [75-78].
Developing ethical AI systems is extremely crucial, thus the models need to undergo thorough evaluation for different data and tasks using multiple performance tests and explainability assessments, ensuring data privacy is maintained and preventing algorithmic bias from noisy data or external attacks. Listed are some recommended strategies for ethical AI systems to address the shortcomings of traditional AI in the healthcare field [67,79]:
i. Building efficient and trustworthy user-centered AI systems.
ii. Consistently make system updates based on user feedback and real-time performance, striking a balance between simple and optimal solutions.
iii. Provide the broader community with information, such as tools, databases, research, and other resources.
iv. Remain vigilant for both immediate and distant issues to anticipate the system’s overall performance and forecast user reactions to upcoming improvements.
v. Iterate integration and isolation testing of subsystems, taking into consideration different standard data sets, users, and use cases.
vi. Inform users about the depth and breadth of training while acknowledging the limitations set by the dataset and model.
viii. Utilize various indicators and metrics to comprehend the trade-offs among diverse failures and experiences.
Artificial intelligence and Robotic technologies in healthcare in Europe
In the European Union’s 27 countries, the proportion of population aged 80 and above is expected to double, from 6.1% in 2020 to 12.5% in 2060. Meanwhile, there is a decline in the number of well-educated and trained young healthcare professionals, leading to a significant shortage of skilled personnel such as physicians, nurses and midwives in several countries across the European Union [80,81]. A fundamental problem, especially in hospitals in Southern Europe, is the lack of communication between patients, physicians, nurses, and other healthcare employees. As hospitals often require shifts of more than twelve hours, it seems that the rate of inadequate care for patients is high when physicians and nurses work more than thirteen hours. Encouraging healthcare professionals is a difficult problem and recruiting them from overseas is not the ideal answer. Furthermore, studies have indicated that nurses are at a higher risk of fatigue, burnout, and job dissatisfaction when they work more than ten hours. Another research study showed that nurses reported more mistakes in decision-making as a result of fatigue, daytime drowsiness, lack of recovery time between shifts, and low quality of sleep, compared to reports from well-rested nurses. Long-term working shifts harm the health and well-being of healthcare personnel, which increases the voluntary turnover rate, and also negatively affects the care of patients [82,83]. Research has shown that the development of AI-enabled health information technology can help healthcare personnel in multi-tasking work environments such as vital sign confirmation and collection, medication management, infectious diseases, etc. In particular, delegating non value-added nursing activities and tasks will alter the role of nurses, allowing them to engage with patients in a more efficient and effective manner. Equally, there is convincing evidence that implementing AI and robots in the workplace will create new opportunities and positive job growth in the long run, this is because many new specializations will be created, coming from data science and engineering in the service sector and applications (e.g., programmers, data scientists, cybersecurity experts and IT specialists) [84-86].
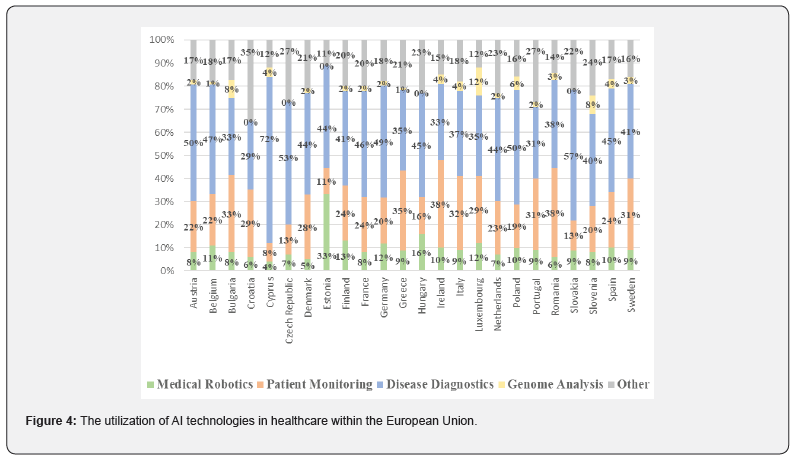
Many European countries have been leading the way in AI research and development, prioritizing patient outcomes while also focusing on cost reduction and enhanced efficiency. In parallel, the European Union has been actively involved in shaping AI policy by creating ethical guidelines and initiating the AI4EU project to drive the rapid growth and acceptance of AI technology across Europe. In Figure 4, it seems that Estonia with 33% leads in the use of medical robotics, Ireland and Romania (38%) have the higher rates in usage of AI technologies for patients monitoring, and Cyprus (72%), Slovakia (57%) and Czech Republic (53%) are at the forefront of using AI for disease diagnosis. Greece has a geographical distribution that includes numerous isolated villages both on the mainland and the islands, leading to challenges in providing healthcare to residents. Additionally, due to the shortage of digital data such as integrations to the Electronic Health Record (EHR), starting any project will require building from the ground up and potentially developing AI systems that prioritize data quality over quantity. This will be based on a dataset that is scalable, customizable, and governable. Healthcare expenditures are not increasing at the same rate as revenue. Additionally, many research studies indicate that primary care is not functioning efficiently, leading to significant issues in hospital emergency departments and resulting in longer wait times and reduced quality of patient care [87,88].
Conclusion
By 2050, estimated that approximately a quarter of total population in Europe, expected to be aged 65 and over. Managing these patients will be costly and healthcare systems will need to shift from a philosophy based on episodic care to one that focuses on more personalized, preventive and long-term care management. Millions of patient information and details, including blood values, medication plans and brain scans, are stored in clinical and practice databases every day. Digitization is generating huge amounts of data. However, the most important thing is not only to collect the data, but also to make the best use of it.
An efficient healthcare system, particularly hospitals, are essential for society as they are key components in providing quality services and resources to patients within a network of various actors. AI has a promising future in healthcare, with advancements in disease classification and AI-monitored surgical robots on the horizon. Given the shortages of skilled healthcare professionals, AI and robotics-based solutions could represent one way to increase quantity and quality of health care, while helping to address a more accurate and more efficient patient pathway. Healthcare systems will find it hard to stay sustainable without significant structural and transformational changes.
Nevertheless, the utilization of AI and robotic technologies in healthcare has sparked concerns regarding relying solely on technology to address healthcare challenges. These concerns include the importance of maintaining transparency and safeguarding data to ensure responsible deployment in sensitive healthcare scenarios. It is crucial to proceed with caution to protect patient privacy and security while also working to alleviate resistance to automated and somewhat unclear methods of assisting in various healthcare services. In the upcoming future, we will need to confront similar moral quandaries. These advantages and constraints indicate that optimizing the role of AI systems and Robotics is possible only through cooperation with human intelligence.
Declaration of Interest: The authors declare no conflict of interest.
Conflict of Interest
Conflict of Interest: Each author declares that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article.
Funding
None.
Author’s contribution
All authors were involved in all steps for preparation of this article, including final proofreading and gave final approval of the version to be published.
References
- Davenport T, Kalakota R (2019) The potential for artificial intelligence in healthcare. Future Healthc J 6(2): 94-98.
- Berwick DM, Nolan TW, Whittington J (2008) The Triple Aim: Care, health, and cost. Health Affairs 27(3): 759-769.
- Atella V, Piano Mortari A, Kopinska J, Federico B, Franceso L, et al. (2019) Trends in age‐related disease burden and healthcare utilization. Aging Cell 18: e12861.
- Aronson S, Rehm H (2015) Building the foundation for genomic-based precision medicine. Nature 526: 336-342.
- Morley J, Floridi L (2020) An ethically mindful approach to AI for Health Care. SSRN Electron J 395: 254-256.
- Bohr A, Memarzadeh K (2020) The rise of artificial intelligence in healthcare applications. Artificial Intelligence in Healthcare 2020: 25-60.
- European Commission (2017) The 2018 Ageing Report: Underlying Assumptions and Projection Methodologies. Publications Office of the European Union; Luxembourg: pp. 1-240.
- Phillips AL, Burr RL, Dunner DL (2018) rTMS effects in patients with co-morbid somatic pain and depressive mood disorders. J Affect Disord 241: 411-416.
- Bokolo Anthony (2020) Use of Telemedicine and Virtual Care for Remote Treatment in Response to COVID-19 Pandemic. J Med Syst 44(7): 132.
- Fortin M, Lapointe L, Hudon C, Vanasse A, Ntetu AL, et al. (2004) Multimorbidity and quality of life in primary care: a systematic review. Health Qual Life Outcomes 2: 51.
- Burton RJ, Albur M, Eberl M, Cuff SM (2019) Using artificial intelligence to reduce diagnostic workload without compromising detection of urinary tract infections. BMC Med Inform Decis Mak 19(1): 171.
- De Mauro A, Greco M, Grimaldi M (2016) A formal definition of Big Data based on its essential features. Library Rev 65(3): 122-135.
- Alowais SA, Alghamdi SS, Alsuhebany N, Tariq A, Abdulrahman IA, et al. (2023) Revolutionizing healthcare: the role of artificial intelligence in clinical practice. BMC Med Educ 23(1): 689.
- Vinny PW, Vishnu VY, Padma Srivastava MV (2021) Artificial Intelligence shaping the future of neurology practice. Med J Armed Forces India 77(3): 276-282.
- Kaplan A, Haenlein M (2020) Rulers of the World, Unite! The Challenges and Opportunities of Artificial Intelligence. Business Horizons 63(1): 37-50.
- Potočnik J, Foley S, Thomas E (2023) Current and potential applications of artificial intelligence in medical imaging practice: A narrative review. J Med Imaging Radiat Sci 54(2): 376-385.
- Enayati M, Sir M, Zhang X, Sarah JP, Elizabeth D, et al. (2021) Monitoring Diagnostic Safety Risks in Emergency Departments: Protocol for a Machine Learning Study. JMIR Res Protoc 10(6): e24642.
- Ahsan MM, Luna SA, Siddique Z (2022) Machine-Learning-Based Disease Diagnosis: A Comprehensive Review. Healthcare (Basel) 10(3).
- Habehh H, Gohel S (2021) Machine Learning in Healthcare. Curr Genomics 22(4): 291-300.
- Qin Z, Ye H, Li GY, Juang BHF (2019) Deep learning in physical layer communications. IEEE Wirel Commun 26(2): 93-99.
- Miotto R, Wang F, Wang S, Jiang X, Dudley JT (2018) Deep learning for healthcare: review, opportunities and challenges. Brief Bioinform 19(6): 1236-1246.
- Ramirez-Alcocer UM, Tello-Leal E, Romero G, Macías-Hernández BA (2023) A Deep Learning Approach for Predictive Healthcare Process Monitoring. Information 14(9): 508.
- Hossain E, Rana R, Higgins N, Soar J, Barua PD, et al. (2023) Natural Language Processing in Electronic Health Records in relation to healthcare decision-making: A systematic review. Comput Biol Med 155: 106649.
- Sim JA, Huang X, Horan MR, Stewart CM, Robison LL, et al. (2023) Natural language processing with machine learning methods to analyze unstructured patient-reported outcomes derived from electronic health records: A systematic review. Artif Intell Med 146: 102701.
- Gonzalez-Hernandez G, Sarker A, O'Connor K, Savova G (2017) Capturing the Patient's Perspective: a Review of Advances in Natural Language Processing of Health-Related Text. Yearb Med Inform 26(1): 214-227.
- Fairag M, Almahdi RH, Siddiqi AA, Fares AK, Badran SA, et al. (2024) Robotic Revolution in Surgery: Diverse Applications Across Specialties and Future Prospects Review Article. Cureus 16(1): e52148.
- Reddy K, Gharde P, Tayade H, Patil M, Reddy LS, et al. (2023) Advancements in Robotic Surgery: A Comprehensive Overview of Current Utilizations and Upcoming Frontiers. Cureus 15(12): e50415.
- Maalouf N, Sidaoui A, Elhajj IH, Asmar D (2018) Robotics in Nursing: A Scoping Review. J Nurs Scholarsh 50(6): 590-600.
- Gibelli F, Ricci G, Sirignano A, Turrina S, De Leo D (2021) The Increasing Centrality of Robotic Technology in the Context of Nursing Care: Bioethical Implications Analyzed through a Scoping Review Approach. J Healthc Eng 2021: 1478025.
- Łukasik S, Tobis S, Kropińska S, Suwalska A (2020) Role of Assistive Robots in the Care of Older People: Survey Study Among Medical and Nursing Students. J Med Internet Res 22(8): e18003.
- Arjoune Y, Nguyen TN, Doroshow RW, Shekhar R (2023) Technical characterization of digital stethoscopes: towards scalable artificial intelligence-based auscultation. J Med Eng Technol 47(3): 165-178.
- König IR, Fuchs O, Hansen G, von Mutius E, Kopp MV (2017) What is precision medicine? Eur Respir J 50(4): 1700391.
- Uysal G, Ozturk M (2020) Hippocampal atrophy based Alzheimer's disease diagnosis via machine learning methods. J Neurosci Methods 337: 108669.
- Miller DD, Brown EW (2018) Artificial Intelligence in Medical Practice: The Question to the Answer? Am J Med 131(2): 129-133.
- Slawomirski L, Klazinga N (2020) The economics of patient safety: from analysis to action. Paris: Organisation for Economic Co-operation and Development.
- Hussain F, Cooper A, Carson-Stevens A, Liam D, Peter H, et al. (2019) Diagnostic error in the emergency department: learning from national patient safety incident report analysis. BMC Emerg Med 19(1): 77.
- Wang F, Preininger A (2019) AI in Health: State of the Art, Challenges, and Future Directions. Yearb Med Inform 28(1): 16-26.
- Ferrara M, Bertozzi G, Di Fazio N, Aquila I, Di Fazio A, et al. (2024) Risk Management and Patient Safety in the Artificial Intelligence Era: A Systematic Review. Healthcare 12(5): 549.
- Raile P (2024) The usefulness of ChatGPT for psychotherapists and patients. Humanit Soc Sci Commun 11: 47.
- Sinsky C, Colligan L, Li L, Prgomet M, Reynolds S, et al. (2016) Allocation of Physician Time in Ambulatory Practice: A Time and Motion Study in 4 Specialties. Ann Intern Med 165(11): 753-760.
- Hilliard RW, Haskell J, Gardner RL (2020) Are specific elements of electronic health record use associated with clinician burnout more than others? J Am Med Inform Assoc 27(9): 1401-1410.
- Tawfik DS, Profit J, Lake ET, Liu JB, Sanders LM, et al. (2020) Development and use of an adjusted nurse staffing metric in the neonatal intensive care unit. Health Serv Res 55(2): 190-200.
- Ellahham S, Ellahham N, Simsekler MCE (2020) Application of Artificial Intelligence in the Health Care Safety Context: Opportunities and Challenges. Am J Med Quality 35(4): 341-348.
- Reddy S, Fox J, Purohit MP (2019) Artificial intelligence-enabled healthcare delivery. J R Soc Med 112(1): 22-28.
- Ng ZQP, Ling LYJ, Chew HSJ, Lau Y (2022) The role of artificial intelligence in enhancing clinical nursing care: A scoping review. J Nurs Manag 30(8): 3654-3674.
- O'Connor S, Yan Y, Thilo FJS, Felzmann H, Dowding D, et al. (2023) Artificial intelligence in nursing and midwifery: A systematic review. J Clin Nurs 32(13-14): 2951-2968.
- Cournane S, Byrne D, O’Riordan D, Silke B (2015) Factors associated with length of stay following an emergency medical admission. Eur J Internal Med 26(4): 237-242.
- Naeem M, Coronato A (2022) An AI-Empowered Home-Infrastructure to Minimize Medication Errors. J Sensor Actuator Networks 11(1): 13.
- Amin A, Cardoso S, Suyambu J, Hafiz AS, Rayner PC, et al. (2024) Future of Artificial Intelligence in Surgery: A Narrative Review. Cureus 16(1): e51631.
- Andras I, Mazzone E, van Leeuwen FWB, Geert De N, Matthias NO, et al. (2020) Artificial intelligence and robotics: a combination that is changing the operating room. World J Urol 38(10): 2359-2366.
- Nabrawi E, Alanazi A (2023) Fraud Detection in Healthcare Insurance Claims Using Machine Learning. Risks 11(9): 160.
- Peden RG, Mercer R, Tatham AJ (2016) The use of head-mounted display eyeglasses for teaching surgical skills: A prospective randomised study. Int J Surg 34: 169-173.
- Pakkasjärvi N, Luthra T, Anand S (2023) Artificial Intelligence in Surgical Learning. Surgeries 4(1): 86-97.
- Swartwout E, Drenkard K, McGuinn K, Grant S, El-Zein A (2016) Patient and Family Engagement Summit: Needed Changes in Clinical Practice. J Nurs Adm 46(3 Suppl): S11-18.
- Meskó B, Drobni Z, Bényei É, Gergely B, Győrffy Z (2017) Digital health is a cultural transformation of traditional healthcare. Mhealth 3: 38.
- Morgantini LA, Naha U, Wang H, Simone F, Omer A, et al. (2020) Factors contributing to healthcare professional burnout during the COVID-19 pandemic: A rapid turnaround global survey. PLoS One 15(9): e0238217.
- Ćwiklicki M, Schiavone F, Klich J, Kamila P (2020) Antecedents of use of e-health services in Central Eastern Europe: a qualitative comparative analysis. BMC Health Serv Res 20(1): 171.
- Smith AC, Thomas E, Snoswell CL, Helen H, Ateev M, et al. (2020) Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare 26(5): 309-313.
- Metsky HC, Siddle KJ, Gladden-Young A, James Q, David KY, et al. (2019) Capturing sequence diversity in metagenomes with comprehensive and scalable probe design. Nat Biotechnol 37(2): 160-168.
- Huang S, Yang J, Fong S, Zhao Q (2021) Artificial intelligence in the diagnosis of COVID-19: challenges and perspectives. Int J Biol Sci 17(6): 1581-587.
- Council_of_Europe (2022) AI and control of Covid-19 coronavirus. Council of Europe.
- Elendu C, Amaechi DC, Elendu TC, Jingwa KA, Okoye OK, et al. (2023) Ethical implications of AI and robotics in healthcare: A review. Med 102(50): e36671.
- Mavroforou A, Michalodimitrakis E, Hatzitheo-Filou C, Giannoukas A (2010) Legal and ethical issues in robotic surgery. Int Angiol 29(1): 75-79.
- Esmaeilzadeh P (2020) Use of AI-based tools for healthcare purposes: a survey study from consumers' perspectives. BMC Med Inform Decis Mak 20(1): 170.
- Akinci D'Antonoli T (2020) Ethical considerations for artificial intelligence: an overview of the current radiology landscape. Diagn Interv Radiol 26(5): 504-511.
- Price WN, Cohen IG (2019) Privacy in the age of medical big data. Nat Med 25(1): 37-43.
- Naik Nithesh, Zeeshan BM Hameed, Dasharathraj KS, Dishant S, Milap S, et al. (2022) Legal and ethical consideration in artificial intelligence in healthcare: who takes responsibility?" Front Surg 9: 862322.
- Scherer MU (2016) Regulating artificial intelligence systems: risks, challenges, competencies, and strategies. Harv J Law Technol 29: 354-400.
- Bouhouita-Guermech S, Gogognon P, Bélisle-Pipon JC (2023) Specific challenges posed by artificial intelligence in research ethics. Front Artif Intell 6: 1149082.
- O'Sullivan S, Nevejans N, Allen C, Andrew B, Simon L, et al. (2019) Legal, regulatory, and ethical frameworks for development of standards in artificial intelligence (AI) and autonomous robotic surgery. Int J Med Robot 15(1): e1968.
- Vellido A (2019) Societal Issues Concerning the Application of Artificial Intelligence in Medicine. Kidney Dis (Basel) 5(1): 11-17.
- (2021) Ethics and governance of artificial intelligence for health: WHO guidance. Geneva: World Health Organization.
- Ahmed MI, Spooner B, Isherwood J, Lane M, Orrock E, et al. (2023) A Systematic Review of the Barriers to the Implementation of Artificial Intelligence in Healthcare. Cureus 15(10): e46454.
- Petersson L, Larsson I, Nygren JM, et al. (2022) Challenges to implementing artificial intelligence in healthcare: a qualitative interview study with healthcare leaders in Sweden. BMC Health Serv Res 22: 850.
- Pepito JA, Locsin R (2019) Can Nurses Remain Relevant in A Technologically Advanced Future? Int J Nursing Sci 6: 106-110.
- Kohli R, Tan SSL (2016) National University of Singapore Electronic Health Records: How Can IS Researchers Contribute to Transforming Healthcare? MIS Q 40: 553-573.
- Klumpp M, Hintze M, Immonen M, Francisco Rodenas R, Fernando Aparicio M, et al. (2021) Artificial Intelligence for Hospital Health Care: Application Cases and Answers to Challenges in European Hospitals. Healthcare (Basel) 9(8): 961.
- Sweeney C, Potts C, Ennis E, Edel E, Raymond B, et al. (2021) Can chatbots help support a person’s mental health? Perceptions and views from mental healthcare professionals and experts. ACM Trans Comput Healthcare 2(3): 1-15.
- Esmaeilzadeh P (2024) Challenges and strategies for wide-scale artificial intelligence (AI) deployment in healthcare practices: A perspective for healthcare organizations. Artif Intell Med 151: 102861.
- Michel JP, Ecarnot F (2020) The shortage of skilled workers in Europe: its impact on geriatric medicine. Eur Geriatr Med 11: 345-347.
- European commission (2020) Population structure and ageing.
- Karaferis D, Balaska D (2024) Violence in the workplace of the health sector-main causes of presentation and development of the phenomenon. J Clin Med Img Case Rep 4(1): 1-7.
- Karaferis D, Aletras V, Raikou M, Niakas D (2022) Factors Influencing Motivation and Work Engagement of Healthcare Professionals. Mater Sociomed 34(3): 216-224.
- Krishnan G, Singh S, Pathania M, Siddharth G, Shuchi A, et al. (2023) Artificial intelligence in clinical medicine: catalyzing a sustainable global healthcare paradigm. Front Artif Intell 6: 1227091.
- Dave M, Patel N (2023) Artificial intelligence in healthcare and education. Br Dent J 234: 761-764.
- Shaji G, Hovan G, Baskar T (2024) Artificial Intelligence and the Future of Healthcare: Emerging Jobs and Skills in 2035. Partners Universal Multidiscip Res J 1(1): 1-21.
- Karaferis DC, Niakas DA, Balaska D, Flokou A (2024) Valuing Outpatients’ Perspective on Primary Health Care Services in Greece: A Cross-Sectional Survey on Satisfaction and Personal-Centered Care. Healthcare 12(14): 1427.
- Karaferis DC, Niakas DA (2024) Exploring Inpatients’ Perspective: A Cross-Sectional Survey on Satisfaction and Experiences in Greek Hospitals. Healthcare 12(6): 658.