Multiple Splanchnic Venous Thromboses: A Fatal Complication of Recurrent Pancreatitis
Richmond R Gomes*
Medicine, Ad-din Women’s Medical College Hospital, Bangladesh
Submission:December 11, 2023; Published:January 19, 2024
*Corresponding author: Richmond Ronald Gomes, Professor, Medicine, Ad-din Women’s Medical College Hospital, Dhaka, Bangladesh, Email: rrichi.dmc.k56@gmail.com
How to cite this article: Richmond R G. Multiple Splanchnic Venous Thromboses: A Fatal Complication of Recurrent Pancreatitis. Adv Res Gastroentero Hepatol, 2024; 20(2): 556034. DOI: 10.19080/ARGH.2024.20.556034.
Abstract
Splanchnic Venous Thrombosis (SVT) is a condition associated with high morbidity. The etiologies of SVT include intra-abdominal inflammation or infection, surgical intervention, abdominal malignancies such as hepatocellular carcinoma (HCC) and pancreatic carcinoma, or abnormality in coagulation caused by various reasons such as liver cirrhosis. Most cases of pancreatitis are mild and self-limited. On the other hand, approximately one quarter of patients with pancreatitis may develop vascular complications such as venous thrombosis. Pancreatitis in combination with vascular complications is dangerous and potentially lethal. The survival of patients with pancreatitis and vascular complications depends on the early diagnosis of these complications. We report a case of a middle-aged male who had recurrent pancreatitis. On radiological imaging, patients were found to have portal vein, splenic vein and superior mesenteric vein thrombosis. The etiology of thrombosis was inflammation around the main portal trunk caused by pancreatitis. The patient recovered after emergent and timely management with initially low molecular weight heparin and bridged by oral apixaban therapy. The article focuses on the aspects of etiology, pathogenesis, diagnosis and management of acute pancreatitis with venous thrombosis.
Keywords: Splanchnic venous thrombosis; Pancreatitis; Low molecular weight heparin; Apixaban; Systemic anticoagulation
Keywords: SVT: Splanchnic Venous Thrombosis; HCC: Hepatocellular Carcinoma; PV: Portal Vein; SV: Splenic Vein; SMV: Superior Mesenteric Vein; EN-Vie: European Network for Vascular Disorders of the Liver
Introduction
Acute pancreatitis is a sudden inflammation of the pancreas. It can have severe complications and high mortality despite treatment. While mild cases are often successfully treated with conservative measures, severe cases may require admission to the intensive care unit or even surgery to deal with impending complications. Isolated Splanchnic vein thrombosis is a rare complication of acute pancreatitis as well as chronic pancreatitis [1-3].
i) It involves the portal vein (PV), splenic vein (SV) and superior mesenteric vein (SMV), either in combination or separately. Splanchnic vein thrombosis is often an incidental finding on radiological imaging performed to assess the severity of an attack of acute pancreatitis; however, its clinical manifestations may include signs and symptoms that overlap with those of the pancreatitis.
ii) Splanchnic vein thrombosis is associated with prothrombotic or hypercoagulable disorders, but in the context of acute pancreatitis a more direct inflammatory process has been implicated.
iii) Although the natural history of splanchnic vein thrombosis in AP is unclear, severe hemorrhage, bowel ischemia, portal hypertension and liver failure have been reported.
Case Report
A 45-year male patient, a chronic smoker and nonalcoholic, presented with the complaints of epigastric pain for 3 days. The pain was severe, squeezing in character, radiating to back, increased on exertion, not responding to NSAIDs and anti-spasmodic. Patients had recurrent vomiting episodes containing food particles, non-projectile, non-bilious and non-blood stained. There was no history of abdominal distention, fever, jaundice, decreased urine output, respiratory discomfort or altered behavior. There was no history of diabetes, hypertension, tuberculosis or any other chronic illness but had similar attacks in the last 3 years. On general examination, the patient was conscious and well oriented. His pulse rate was 96/minute and blood pressure were 130/80 mm of Hg. There was no pallor, icterus, cyanosis, clubbing or lymphadenopathy. Patient had average built with BMI of 28 kg/m2. On systemic examination, tenderness was elicited at epigastric region on superficial palpation. Bowel sounds were absent. The rest of the per abdominal examination was normal. Cardiovascular, respiratory and central nervous system examination was normal. On the day of admission, the laboratory examination revealed; hemoglobin of 12.5 g/dL, total leucocyte counts of 21500/ mm3 with predominant polymorphonuclear cells, platelet count of 450×103/ μL. CRP was raised(211.8mg/dl). Renal and liver functions were normal with blood urea of 27 mg/dL, serum creatinine of 1.1 mg/ dL, serum uric acid of 2.6 mg/dL, corrected serum calcium of 9.3 mg/dL, serum phosphate of 2.1 mg/dL, aspartate aminotransferase of 63 U/L, alanine aminotransferase, of 26 U/L, serum alkaline phosphatase of 87 U/L, total serum protein of 5.8 g/dL, total serum bilirubin of 0.8 mg/ dL, serum triglycerides of 190 mg/dL, total serum cholesterol of 107 mg/dL, high density lipoprotein of 27mg/ dL, low density lipoprotein of 62 mg/d. The evidence of pancreatitis was evident with serum amylase of 3568 U/L, serum lipase of 1206 U/L. The fasting blood sugar of the patient was 92 mg/dL and HbA1c was 5.5%. The urine complete examination was within normal limits.
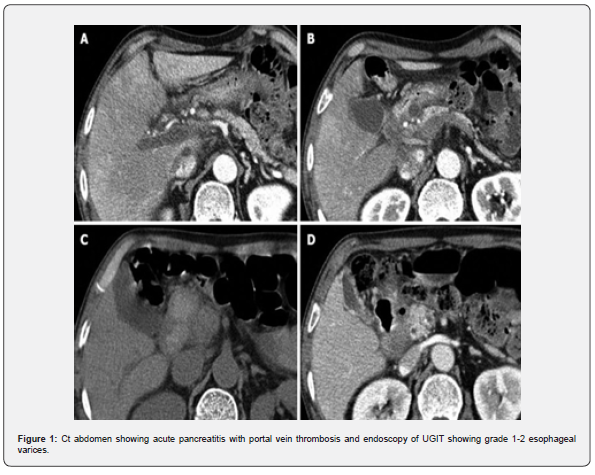
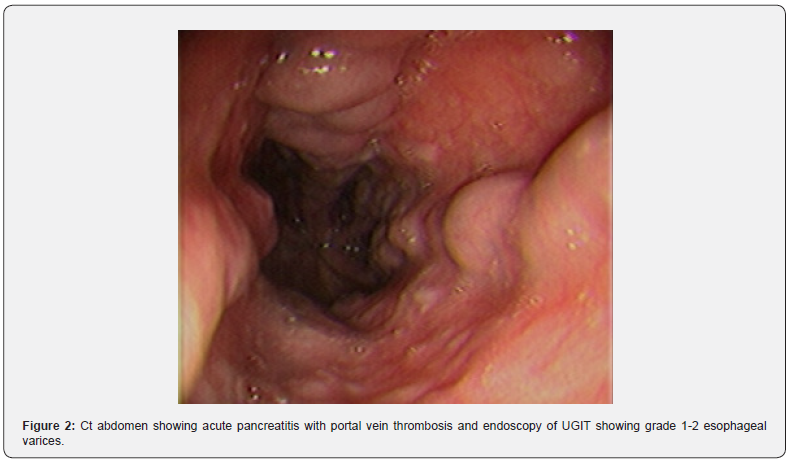
Arterial blood gas analysis was normal. Tests for Hbs Ag and Anti-HCV were negative. Serum anti-nuclear antibody by immune- fluorescence technique was negative. The thrombophilia profile (including protein C level, protein S level, Anti thrombin 3 level, Anti-phospholipid antibodies) was normal. The Chest X-ray and ECG was normal. Ultrasound abdomen revealed hypoechoic and non-homogenous pancreatic parenchyma compatible with acute pancreatitis. CT abdomen showed pancreatitis with dilated portal vein suggestive of thrombosis extending to splenic vein and superior mesenteric vein and splenomegaly (Figure 1). Upper gastrointestinal endoscopic study showed grade 1-2 varices (Figure 2). After the exclusion of secondary causes for the venous thrombi, the cause was attributed to acute pancreatitis. Patient was managed timely with analgesics, parenteral nutrition and antibiotics. He also started subcutaneous low molecular weight heparin which was later bridged with oral apixaban. With treatment his condition improved. He was discharged with propranolol and oral apixaban. On discharge his CRP was 37.9 mg/dl, serum amylase of 168 U/L, serum lipase of 96 U/L. There is a plan to continue apixaban for 3 months and follow up the patient at outpatient door with repeat CT abdomen.
Discussion
Most cases of pancreatitis are mild and self-limiting. However, around one fourth of the cases may develop various complications and can lead to mortality. Among the major complications occurring, vascular complications are well recognized and seek emergency care. In the literature, major vascular complications of pancreatitis occur with a frequency of 1.2-14%, with a greater incidence seen in chronic pancreatitis (7-10%) than acute pancreatitis (1-6%). The overall mortality rate due to hemorrhage in acute pancreatitis has been reported to reach ranges as high as 34-52% and is significantly higher than in cases of patients without bleeding [4]. Isolated splenic vein thrombosis is relatively uncommon in patients with pancreatitis, occurring in about 1-2% of cases [5]. Although much less common, portal and superior mesenteric vein thrombosis can also occur because of pancreatitis [6]. Pulmonary thromboembolism is also a known complication following venous thrombosis after pancreatitis [7,8]. Various mechanisms are postulated to cause these splanchnic and extrasplanchnic venous thromboses. The splanchnic veins especially, superior mesenteric vein, portal vein and splenic vein possibly get thrombosed due to release of proteolytic enzymes from the inflamed pancreas. As the splenic vein lies immediately adjacent to the pancreas, it is the most affected vein. Thromboses of distant veins are postulated to be due to inflammatory vasculitis and hypercoagulable states [8,9]. Venous thrombosis may also occur due to extrinsic compression by the edematous gland or pseudocyst. Pseudocysts of the caudal pancreas are complicated by splenic vein obstruction in nearly 30% of cases. Intimal injury and venous thrombosis can occur especially when SVT is due to acute pancreatitis or recurrent episodes of pancreatitis. In either the intrinsic or extrinsic mechanisms stasis of blood flow occurs and eventually leads to thrombosis.
The European Network for Vascular Disorders of the Liver (EN-Vie) recommends the utilization of anticoagulation early in patients with acute SVT in non-cirrhotic, non-malignant patients. The rate of recanalization is higher if anticoagulants are started earlier. But the use of anticoagulants in this scenario. poses challenge as these patients are at increased risk of hemorrhage because of pseudo-aneurysms and the need for surgical interventions for management of pancreatic necrosis and abscess [10]. Ascites and SVT were identified as factors predictive of worse evolution [11]. Mortality associated with acute SMV thrombosis in the general population is high, at 20-50%, [12] depending on the grade of obstruction, the collateral vascularization, comorbidities, and delay in diagnosis and treatment. In the present case SMV thrombosis did not appear to be an indication for anticoagulation therapy. According to a study by Gonzelez et al. [13] anticoagulation could be administered if there is evidence of progression of PV thrombosis, ascites or SMV thrombosis. The controversy regarding anticoagulant therapy is persistent and guidelines need to be framed in this regard to make the therapeutic decisions simpler. Our patient did not have any known inherited prothrombotic state or pseudocyst compressing the veins which were found thrombosed. Hence, the most probable reason for thrombosis in our patient was systemic inflammation. These venous thromboses are known to respond to anticoagulation [14,15]. Our patient responded to anticoagulation as well with partial resolution of thrombosis. To conclude, thrombosis of splanchnic vascular bed can occur in pancreatitis. This can be effectively treated with anticoagulation and hence, mortality related complications such as pulmonary embolism can be prevented.
Conclusion
Splanchnic vein thrombosis is a relatively uncommon observation in patients with acute, chronic or recurrent pancreatitis. Control of the underlying disease may be the first choice for treatment of this kind of PVT. The association with portal, splenic and mesenteric vein is rare. Recanalization is observed in almost a third of patients, irrespective of whether they receive systemic anticoagulation, and this may reflect the resolution of the pancreatitis itself. As the venous thrombi could lead to fatal complications, early diagnosis and timely management would prevent hazardous outcomes.
References
- Butler JR, Eckert GJ, Zyromski NJ, Leonardi MJ, Lillemoe KD, et al. (2011) Natural history of pancreatitis-induced splenic vein thrombosis: a systematic review and meta-analysis of its incidence and rate of gastrointestinal bleeding. HPB (Oxford)13(12): 839-845.
- Nicolas De PI, Corral De La CMA, Nicolas De PJM, Gallardo SF, Medranda MA (2005) Vascular complications of pancreatitis. Rev Clin Esp 205: 326-332.
- Nordback I, Sisto T (1989) Peripancreatic vascular occlusions as a complication of pancreatitis. Int Surg 74(1): 36-39.
- Barge JU, Lopera JE (2012) Vascular complications of pancreatitis: Role of interventional therapy. Korean J Radiol 13(Suppl 1): 45-55.
- Mallick I, Winslet M (2004) Vascular complications of pancreatitis. J Pancreas 5: 328-337.
- Rattner DW, Warshaw AL (1990) Venous, biliary, and duodenal obstruction in chronic pancreatitis. Hepatogastroenterology 37: 301-306.
- Jorge CJ, Mansilla RA, Paz YA, Segura JI, Ferron Orihuela JA (2012) Urgent vascular complications in acute pancreatitis. Cir Esp 90(2): 134-136.
- Zhang Q, Zhang QX, Tan XP, Wei-Zheng W, Chang-Hua H, et al. (2012) Pulmonary embolism with acute pancreatitis: A case report and literature review. World J Gastroenterol 18(6): 583-586.
- Orr DW, Patel RK, Lea NC, Westbrook RH, O'Grady JG, et al. (2010) The prevalence of the activating JAK2 tyrosine kinase mutation in chronic portosplenomesenteric venous thrombosis. Aliment Pharmacol Ther 31: 1330-1336.
- Kumar S, Sahu SK, Ray JP (2014) A Case of Acute Necrotizing Pancreatitis Complicated by Portal Vein Thrombosis. J Surgery 10(2): 171-172.
- Plessier A, Darwish-Murad S, Hernandez-Guerra M, Yann C, Federica F, et al. (2010) Acute portal vein thrombosis unrelated to cirrhosis: a prospective multicentre follow-up study. Hepatology 51(1): 210-218.
- Boley S, Kaleya R, Brandt L (1992) Mesenteric venous thrombosis. Surg Clin North Am 72(1): 183-201.
- Gonzelez HJ, Sahay SJ, Samadi B, Davidson BR, Rahman SH (2011) Splanchnic vein thrombosis in severe acute pancreatitis: a 2-year, single-institution experience. HPB (Oxford) 13(12): 860-864.
- Jiao HB, Qiao Z, Tan XL, Jun-dong D, Yang F, et al. (2004) Effects of anticoagulation therapy with low molecular weight heparin in acute pancreatitis. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue 16(12): 712-714.
- Alvi AR, Bibi S, Rehman Z, Niazi SK (2010) Acute mesenteric, portal and inferior vena cava (IVC) venous thrombosis: optimal outcome achieved with anticoagulation. J Pak Med Assoc 60(5): 397-399.