Mammosomatotropic Adenoma and Acromegaly; What Particularities?
Sara Askaoui* ,Guizlane El Mghari , Nawal El Ansari and Hanane Raiss
Department of Endocrinology, Med VI University Hospital Center, Morocco
Submission: March 20, 2019;Published: May 20, 2019
*Corresponding author: Sara Askaoui, Department of Endocrinology, Diabetology and Metabolic Diseases, Med VI University Hospital Center, Marrakech, Morocco
How to cite this article: Sara A, Guizlane E M, Nawal E A, Hanane R. Mammosomatotropic Adenoma and Acromegaly; What Particularities?. 0030 Theranostics Brain,Spine & Neural Disord. 2019; 4(2): 555632.DOI:10.19080/JOJS.2019.04.555632
Abstract
Acromegaly is a rare condition, usually secondary to excessive production of somatotropic hormone (GH) by a pituitary adenoma, which is clinically expressed either by acromegaly or by gigantism depending on the age of onset. Several histological types are involved. We usually distinguish somato-prolactin adenoma. The mammosomatotropic adenoma is a particular entity, characterized by an intense anti-GH immunohistochemistry and a lower anti-prolactin immunopositivity, but within the same cell. We report 4 observations of a histological type: mammosomatotropic adenoma.
Keywords: Acromegaly Mammosomatotropic adenoma GH prolactin IGF1 Immunohistochemistry
Introduction
Acromegaly is a disease related to hypersecretion of growth hormone (GH), a pituitary adenoma somatotropic in more than 90% of cases [1,2]. She is responsible for an acquired dysmorphic syndrome, and rheumatological, cardiovascular, respiratory, metabolic, etc. consequences. Which condition the prognosis: they are indeed all the more severe as the excess of GH has been prolonged and important [3,4]. The severity of acromegaly can also, of course, stem from the pituitary tumor that is the cause, and which can be the cause of a tumor syndrome, marked by headaches and / or visual disturbances (by chiasmatic compression).
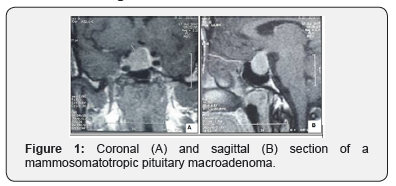
The diagnosis of acromegaly is based on the demonstration of a high plasma concentration of GH and especially non-breakable by oral hyperglycemia (greater than 0.4 μg l-1). Once the diagnosis of acromegaly has been made, it is necessary to evaluate, by magnetic resonance imaging [MRI], the volume and possible expansions of the pituitary tumor [5-10]. Several histological types are involved. Immunohistochemistry provides conclusive evidence that significant diversity exists between tumors secreting excess growth hormone (GH). We report 4 observations of a particular histological type: mammosomatotropic adenoma.
Observation
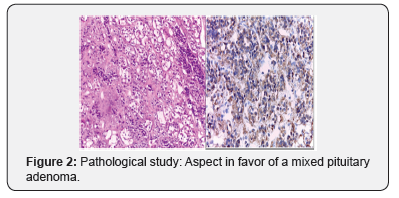
It is about four patients consulting at the endocrinology department of Med VI University Hospital of Marrakech for an acromegaloid syndrome (in 3 cases) with a case of acrogigantism. The average age was 42.7 years, with a sex ratio H / F of 0.25. The biology has shown a high level of IGF1 in all cases, with a highprolactin level in a single patient. Magnetic resonance imaging of the hypothalamic-pituitary region has demonstrated the presence of a pituitary macroadenoma in all these patients. (Figure 1) The latter benefited from first line transsphenoidal surgery, whose anatomopathological and immunohistochemical study objectified an aspect in favor of a mamo somatotropic adenoma (Figure 2), for which our patients were all placed under cabergoline with a somatostatin analogue.
Discussion
Acromegaly is a rare condition, usually secondary to excessive production of somatotropic hormone (GH) by a pituitary adenoma, either alone or in combination with another hormone, including prolactin. We usually distinguish somato-prolactin adenoma. The mamo somatotropic adenoma is characterized by an intense anti-GH immunohistochemistry and a lower antiprolactin immunopositivity, but within the same cell. Electron microscopy confirms this granular colocalization of the two hormones. The diagnosis of pluro hormonal somatotropic adenomas requires the routine practice of immunohistochemical tests because there is no specific clinical presentation. Even if they remain rare, their treatment does not differ from the other types described in acromegaly [11-19].
Conclusion
The mamo somatotropic adenoma is very rare, characterized by an intense anti-GH immunohistochemistry and a lower antiprolactin immunopositivity, but within the same cell. Electron microscopy confirms this granular colocalization of the two hormones.
References
- Chanson P Acromégalie (2006) Encyclopédie médico chirurgicale. Br J Ophthalmol 56(4): 377.
- Melmed S (2006) Medical progress: acromegaly. N Engl J Med 355(24): 2558-2573.
- Giustina A, Casanueva FF, Cavagnini F, Chanson P, Clemmons D, et al. (2003) Diagnosis and treatment of acromegaly complications. J Endocrinol Invest 26(12): 1242-1247.
- Colao A, Ferone D, Marzullo P, Lombardi G (2004) Systemic complications of acromegaly: epidemiology, pathogenesis, and management. Endocr Rev 25(1): 102-152.
- Freda PU, Reyes CM, Nuruzzaman AT, Sundeen RE, Bruce JN (2003) Basal and glucose-suppressed GH levels less than 1g/l in newly diagnosed acromegaly. Pituitary 6(4): 175-180.
- Bayle M, Chevenne D, Dousset B, Lahlou N, Le Bouc Y, et al. (2004) Recommandations pour la standardisation des dosages d’hormone de croissance. Ann Biol Clin (Paris) 62 : 155-163.
- Trainer PJ, Barth J, Sturgeon C, Wieringaon G (2006) Consensus statement on the standardisation of GH assays. Eur J Endocrinol 155:1-2.
- Pokrajac A, Wark G, Ellis AR, Wear J, Wieringa GE, et al. (2007) Variation in GH and IGF-I assays limits the applicability of international consensus criteria to local practice. Clin Endocrinol (Oxf) 67(1): 65-70.
- Souberbielle JC, Noel M (2007) Les dosages d’hormone de croissance et d’IGF1. Med Clin Endocrinol Diabete.
- Cazabat L, Souberbielle JC, Chanson P (2008) Dynamic tests for the diagnosis and assesment of treatment efficacy in acromegaly. Pituitary 11(2): 129-139.
- Mukherjee A, Monson JP, Jonsson PJ, Trainer PJ, Shalet SM (2003) Seeking the optimal target range for insulin-like growth factor-I during the treatment of adult growth hormone disorders. J Clin Endocrinol Metab 88(12): 5865-5870.
- Giustina A, Barkan A, Casanueva FF, Cavagnini F, Frohman L, et al. (2000) Criteria for cure of acromegaly: a consensus statement. J Clin Endocrinol Metab 85(2): 526-529.
- Colao A, Attanasio R, Pivonello R, Cappabianca P, Cavallo LM, et al. (2006) Partial surgical removal of growth hormone-secreting pituitary tumors enhances the response to somatostatin analogs in acromegaly. J Clin Endocrinol Metab 91(1): 85-92.
- Cozzi R, Montini M, Attanasio R, Albizzi M, Lasio G, et al. (2006) Primary treatment of acromegaly with octreotide LAR: a long-term (up to 9 years) prospective study of its efficacy in the control of disease activity and tumor shrinkage. J Clin Endocrinol Metab 91(4):1397-1403.
- Scotti G, Yu CY, Dillon WP, Norman D, Colombo N, et al. (1988) MR imaging of cavernous sinus involvement by pituitary adenomas. AJR Am J Roentgenol 151(4): 799-806.
- Bourdelot A, Coste J, Hazebroucq V, Gaillard S, Cazabat L, et al. (2004) Clinical, hormonal and magnetic resonance imaging (MRI) predictors of transsphenoidal surgery outcome in acromegaly. Eur J Endocrinol 150(6): 763-771.
- Colao A, Ferone D, Lastoria S, Marzullo P, Cerbone G, et al. (1996) Prediction of efficacy of octreotide therapy in patients with acromegaly. J Clin Endocrinol Metab 81(6): 2356-2362.
- Plockinger U, Bader M, Hopfenmuller W, Saeger W, Quabbe HJ (1997) Results of somatostatin receptor scintigraphy do not predict pituitary tumor volume – and hormone – response to ocreotide therapy and do not correlate with tumor histology. Eur J Endocrinol 136(4): 369-376.
- Borson-Chazot F, Houzard C, Ajzenberg C, Nocaudie M, Duet M, et al. (1997) Somatostatin receptor imaging in somatotroph and nonfunctioning pituitary adenomas: correlation with hormonal and visual responses to octreotide. Clin Endocrinol 47(5): 589-598.