Early Decompression in Traumatic Cervical Dislocation Improve Patient Neurology Outcome
Juzaily Fekry Leong*, Tan Jin Aun, Kamalnizat Ibrahim, Azmi Baharudin, Mohd Hisam Muhamad Ariffin and Shaharuddin Abdul Rhani
Department of Orthopaedic and Traumatology, Faculty of Medicine, University Kebangsaan Malaysia, Malaysia
Submission: September 03, 2018;Published: September 12, 2018
*Corresponding author: Juzaily Fekry Leong, Department of Orthopaedic and Traumatology, Faculty of Medicine, University Kebangsaan Malaysia Medical Centre, 56000 Cheras Kuala Lumpur, Malaysia, Tel: 006-03-91455555; Email: Fekrly@hotmail.com
How to cite this article: Juzaily F L, Tan J A, Kamalnizat I, Azmi B, Md Hisam M A, et al. Early Decompression in Traumatic Cervical Dislocation Improve Patient Neurology Outcome. Theranostics Brain Spine Neuro Disord. 2018; 3(5): 555623. DOI: 10.19080/TBSND.2018.03.555623
Abstract
There have been vast numbers of studies looking at the timing of surgical intervention for traumatic spinal cord injuries but still no consensus has been reached on the optimum timing of spinal decompression surgery. A review of the current literature revels varying results with some indicate potential neurological benefit associated with “early” decompression, while others do not. We have demonstrated that early surgical intervention within 24 hours in our patient with cervical dislocation improve neurological outcome without any complications.
Keywords: Decompression; Spinal Cord injury; Neurology outcome
Introduction
Traumatic cervical spine fractures or dislocations are often associated with cervical spinal cord injury (SCI) as a result of several mechanisms, including narrowing of the cervical spinal canal or by direct displacement of one cervical spine component with direct focal compression on the spinal cord. This will lead to worsening neurological condition due to haematoma formation, oedema progression and spinal instability. Reduction of the cervical spine displacement can restore the spinal cord diameter or relieve the focal compression on the spinal cord. Spinal decompression surgery is then beneficial for decreasing neurological impairment after post spinal cord injury (SCI). Some studies have shown that it improves patient outcome by preventing the activation of secondary injury mechanism [1,2].
Case Report
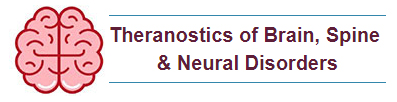
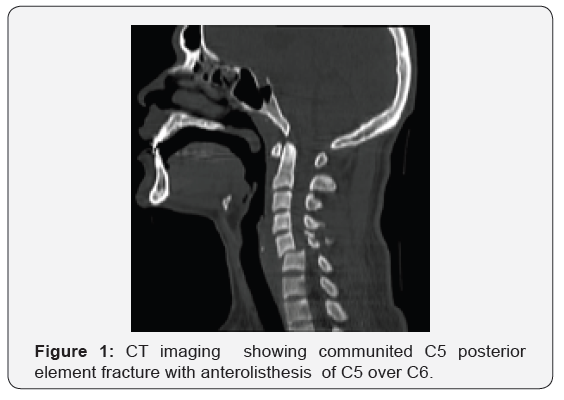
We present a case of a 23-year-old Malay gentleman who sustained C5/C6 fracture dislocation after neck injury during rugby match. Post trauma he complained of bilateral upper and lower limbs weakness with reduced sensation on all limbs. His upper limb power were grade 3 from C5 to T1 bilaterally and lower limb were 0 from L2 to S1 bilaterally. His sensation was reduced from C7 to T2 and absent from T3 downwards bilaterally. Anal tone was intact. Urgent CT (Figure 1) and MRI (Figure 2) of his cervical spine have shown comminuted left C5 posterior element fracture with disruption of the left C5/C6 facet joint causing anterolisthesis and significant spinal canal stenosis at C5/C6 level complicated by spinal cord compression and oedema.
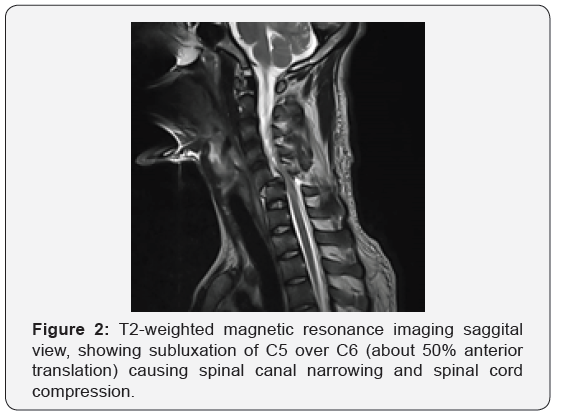
He was diagnosed with C5/C6 fracture dislocation with spinal stenosis and anterolisthesis with incomplete neurology ASIA C (American Spinal Injury Association). Spinal cord decompression and posterior instrumentation (Figure 3) with fusion from C3 to C7 was done within 12 hours from time of injury. Post-operative day one, he has shown regain power of his upper limb bilaterally and right lower limb. At post-operative day 5 he regained almost normal power to his bilateral upper limb and right lower limb with some residual weakness on left lower limb (L2-S1). Patient was then discharge with outpatient physiotherapy and occupational therapy.
At follow up of three months post-surgery, patient have complete regain his upper and lower limb power with sensation back to normal (ASIA E). Early surgical compression for this patient has improved his neurology status from ASIA C to ASIA E.
Discussion
Cervical spinal injury usually happened in the young male patient with an average age of 35 years. The most frequent etiologies of injury are motor vehicle accidents and falls, followed by violence and sports-related injuries. Approximately 40% of cervical spinal cord injury patients present with complete spinal cord injuries, 40% with incomplete injury, and 20% with either no cord or only root lesions [3]. Early intervention has been recommended to enhance neurology recovery, but some have argue that delaying surgery decrease physiologic complications and prevents iatrogenic cord injuries [4]. Neural injury occurs during the first hours after SCI leading to hypo-perfusion, ischemia and eventually death of neural cells (first phase of injury), while the majority of injuries occur in the second phase, which starts within few days after trauma. This phase includes apoptosis induction, formation of glial scar, central chromatolysis, disruption in expression of myelin genes, myelin destruction in remained axons, immune cells attacking the site of lesion and release of inflammatory cytokines and etc [5]. Hence decompression in the first hours after injury can prevent secondary injures or lower its severity. A systemic review by Mahmoud Yousefifard et al., have shown that early decompression surgery, within 24 hours of injury, is associated with improved neurologic recovery and decreased post-surgical complications compared to late intervention [6].
The optimum timing of surgery in the first 12 hours after trauma was associated with the best neurologic recovery. The outcomes of treatment within 72 hours and after, did not differ significantly [6]. Another study STASCIS (Surgical Timing in Acute Spinal Cord Injury Study) that represents the largest prospective multi-center study comparing early versus late surgical decompression in the setting of acute traumatic spinal cord injury. They have concluded that decompression prior 24 hours after SCI can be performed safely and is associated with improved neurologic outcome, defined as at least 2 grade AIS improvement at 6 months follow-up [7]. This has been evidently shown in our patient where he showed AIS improvement by 2 grade from ASIA C to ASIA E In conclusion, decompression surgery prior 24 hours after SCI when performed safely can be associated with improved neurologic outcome defined as at least 2 grade AIS improvement at three months follow-up as shown in our case. So it is recommended that surgical decompression be carried out in the first 12 hours after injury and postponing the procedure to later than 24 hours is associated with significant decrease in neurologic improvement and more post-surgical complications.
References
- Sjovold SG, Mattucci SF, Choo AM, Lui J, Dvarak MF, et al. (2013) Histological effects of residual compression sustained for 60 minutes at different depths in a novel rat spinal cord injury contusion model. J Neurotrauma 30(15): 1374-84.
- Wilson J, Singh A, Craven C, Verrier MC, Drew B, et al. (2012) Early versus late surgery for traumatic spinal cord injury: The results of a prospective cancadian cohort study. Spinal Cord 50(11): 840-843.
- Rizzolo SJ, Vaccaaro AR, Cotler JM (1994) Cervical spine trauma. Spine 19(20): 2288-2298.
- Lee AS, MacLean JC, Newton DA (1994) “Rapid traction for reduction of cervical spine dislocations”. J Bone Joint Surg Br 76(2): 352-356.
- Oyinbo CA (2011) Secondary injury mechanisms in traumatic spinal cord injury: A nugget of this multiply cascade. Acta Neurobiol Exp 71(2): 281-299.
- Yousefifard M, Movaghar RV, Baikpour M, Ghelichkhani P, Hosseini M, et al. (2017) Early versus Late decompression for traumatic spinal cord injuries: A systematic review and meta-analysis. Emerg 5(1): e37
- Fehlings MG, Vaccaro A, Wilson JR, Singh A, Cadotte WD, et al. (2012) Early versus delayed decompression for traumatic cervical spinal cord injury: Results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS). PLoS One 7(2): e32037.